
Role of 3-dimensional computed tomography in a rare mediastinal A5 and A9 variation in video-assisted thoracoscopic surgery left upper lobectomy—a case report
Introduction
Video-assisted thoracoscopic surgery (VATS) lobectomy has been accepted as a standard approach for early pulmonary malignancy owing to advantages from minimally-invasive surgery: less post-operative pain and morbidity, quicker recovery and equivalent oncological outcomes compared to conventional thoracotomy (1,2). Disadvantages of VATS compared to thoracotomy include lack of tactile sensation and stereotypic vision as the whole surgical view is through a 2-dimensional monitor. On the other hand, anatomical variation of pulmonary vessels is not uncommon and failure to identify preoperatively may lead to inadvertent extended resection and bleeding especially in VATS.
Performing a preoperative 3-dimensional (3D) computed tomography (CT) image reconstruction is one of the effective ways to detect the variation and avoid such complications (3-6). The 3D image reconstruction has the advantages of identifying pulmonary artery branching up to 95–98% (4-6), lowering incidences of postoperative complications and reducing operative time than those without 3D image reconstruction (4). We present a rare case of mediastinal A5 and A9 detected in preoperative 3D-CT thorax of a patient with left upper lobe lung adenocarcinoma for which he underwent uniportal VATS upper lobectomy uneventfully. We present this case in accordance with the CARE reporting checklist (available at https://jovs.amegroups.org/article/view/10.21037/jovs-22-21/rc).
Case presentation
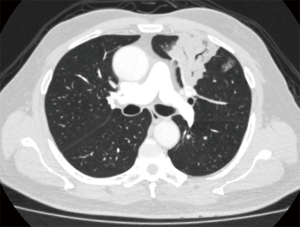
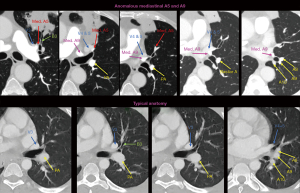
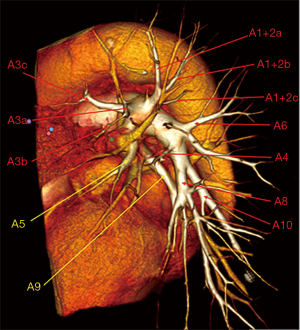
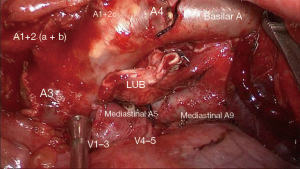
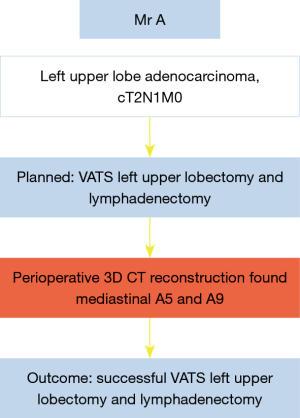
Mr. A is a 71-year-old man diagnosed with left upper lobe adenocarcinoma cT2N1M0. His CT thorax showed a centrally located tumor with suspected involvement of superior pulmonary vein (Figures 1,2). We performed a 3D-CT thorax reconstruction preoperatively for verification, which showed anomalous mediastinal A5 and A9 (Figure 3). He underwent uniportal VATS left upper lobectomy and lymphadenectomy uneventfully. Intraoperatively, the anomalous mediastinal A5 and A9 were identified as portrayed in the reconstructed 3D image, and the mediastinal A9 was preserved (Figure 4). He was discharged home on day 2 of surgery (Video 1).
The timeline of the case is shown in Figure 5.
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Variation of pulmonary vessels is common with the reported rate 16.4% in those who underwent lung resection (7). Failure to identify these variations may increase the risk of vessel injury and critical mistakes during anatomical pulmonary resection, especially through VATS. The 3D-CT reconstruction is reliable to detect anatomical variations of pulmonary vessels, visualize the course of the artery and thus help in planning the surgery ahead to ensure safe pulmonary resection (8). Hagiwara et al. reported that all anomalous or uncommon pulmonary artery and vein branching patterns were precisely shown in 3D-CT imaging (4). Our preoperative 3D-CT image reconstruction detected a rare variation, mediastinal A9, along with mediastinal A5. The intraoperative findings confirmed the anomaly, and the surgery was performed smoothly without inadvertent damage to the anomalous A9. If the mediastinal A9 was not detected preoperatively, it may be divided assuming that it was mediastinal lingular artery, which is the most common variation, consisting of 27.3% of left pulmonary artery (9). This mistake will be eminent if a left anterior segmentectomy, lingulectomy or trisegmentectomy is planned. Agasthian reported a mediastinal A8, which was mistaken for mediastinal A4+5 and thus ligated while performing a VATS left upper lobectomy. The A8 was successfully reconstructed thereafter (10). A preoperative 3D-CT reconstruction would help to prevent such complication.
Pulmonary artery variation is more frequently seen on the left than on the right (11). A mediastinal basal pulmonary artery is extremely rare with the incidence of 0.05% (12). Despite so, it is imperative to be fully aware about this rare variation to perform a safe surgery. Detecting these anomalies from a CT thorax is possible but it requires a long time to learn. If 3D reconstruction is not possible or not available for early detection of the variation, a careful hilar dissection is paramount to avoid intraoperative complications.
The 3D-CT image reconstruction is performed by the thoracic surgeons in our center using the free open-source HOROS software, the 3D volume rendering method. The 3D-CT images can be amplified and rotated in any angle thus providing the surgeon an overview of the 3D relationships of the pulmonary vessels and facilitate planning of surgery for each patient, along with detecting the variation (Figure 2). Based on our experience, the preparation of the 3D-CT image is simple and feasible which takes 5 to 10 minutes and the results are reproducible amongst the surgeons. There will be no additional cost for processing data because the contrast-enhanced CT thorax is performed routinely to all patients. Hence it is recommended before anatomical lung resections.
Disadvantages of 3D-CT reconstruction include missing of the small vessels less than 2mm diameter (4-6), not suitable for patients contraindicated to the use of intravenous contrast such as allergies and chronic renal disease. Besides that, the operating surgeon needs to orientate the 3D image displayed in anatomical inflated lung into deflated lung in operative field (8).
Conclusions
In conclusion, identifying the rare mediastinal A5 and A9 is vital in this case to prevent surgical complications. 3D-CT reconstruction is a simple non-invasive investigation which provides precise information on pulmonary vessels. This simple preparation helps to increase the safety of the procedure and reduces surgical morbidity in anatomical pulmonary resection. Hence preoperative 3D-CT reconstruction should be performed in all anatomical lung resection preoperatively and this case re-emphasizes its importance.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jovs.amegroups.org/article/view/10.21037/jovs-22-21/rc
Peer Review File: Available at https://jovs.amegroups.org/article/view/10.21037/jovs-22-21/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.org/article/view/10.21037/jovs-22-21/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nwogu CE, D'Cunha J, Pang H, et al. VATS lobectomy has better perioperative outcomes than open lobectomy: CALGB 31001, an ancillary analysis of CALGB 140202 (Alliance). Ann Thorac Surg 2015;99:399-405. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. Video-assisted thoracic surgery versus open thoracotomy for non-small cell lung cancer: a meta-analysis of propensity score-matched patients. Interact Cardiovasc Thorac Surg 2013;16:244-9. [Crossref] [PubMed]
- Yao F, Wang J, Yao J, et al. Three-dimensional image reconstruction with free open-source OsiriX software in video-assisted thoracoscopic lobectomy and segmentectomy. Int J Surg 2017;39:16-22. [Crossref] [PubMed]
- Hagiwara M, Shimada Y, Kato Y, et al. High-quality 3-dimensional image simulation for pulmonary lobectomy and segmentectomy: results of preoperative assessment of pulmonary vessels and short-term surgical outcomes in consecutive patients undergoing video-assisted thoracic surgery†. Eur J Cardiothorac Surg 2014;46:e120-6. [Crossref] [PubMed]
- Fukuhara K, Akashi A, Nakane S, et al. Preoperative assessment of the pulmonary artery by three-dimensional computed tomography before video-assisted thoracic surgery lobectomy. Eur J Cardiothorac Surg 2008;34:875-7. [Crossref] [PubMed]
- Watanabe S, Arai K, Watanabe T, et al. Use of three-dimensional computed tomographic angiography of pulmonary vessels for lung resections. Ann Thorac Surg 2003;75:388-92; discussion 392. [Crossref] [PubMed]
- Subotich D, Mandarich D, Milisavljevich M, et al. Variations of pulmonary vessels: some practical implications for lung resections. Clin Anat 2009;22:698-705. [Crossref] [PubMed]
- Yao F, Wang J, Yao J, et al. Three-dimensional image reconstruction with free open-source OsiriX software in video-assisted thoracoscopic lobectomy and segmentectomy. Int J Surg 2017;39:16-22. [Crossref] [PubMed]
- Matsumoto K, Yamasaki N, Tsuchiya T, et al. Three-dimensional computed tomography for a mediastinal basal pulmonary artery. Ann Thorac Surg 2012;94:e115-6. [Crossref] [PubMed]
- Agasthian T. Anomalous mediastinal left lower lobe anterior segmental artery (A8) accidentally divided during left VATS upper lobectomy, a case presentation. J Vis Surg 2021; [Crossref]
- Amore D, Casazza D, Caterino U, et al. Variations in the branching patterns of pulmonary artery during thoracoscopic pulmonary resection. Surg Radiol Anat 2021;43:1331-6. [Crossref] [PubMed]
- Hong JH, Kim HJ, Han DH, et al. Arteria praebronchialis found on MDCT: potentially dangerous aberrant artery supplying the left lower lobe. Surg Radiol Anat 2015;37:1021-6. [Crossref] [PubMed]
Cite this article as: Diong NC, Sathiamuthy N, Dharmaraj B, Balasubbiah N. Role of 3-dimensional computed tomography in a rare mediastinal A5 and A9 variation in video-assisted thoracoscopic surgery left upper lobectomy—a case report. J Vis Surg 2023;9:39.


