
Subcostal uniportal video-assisted thoracoscopic resection of a pulmonary nodule using a diode laser: a case report
Introduction
Minimally invasive surgery has experienced a marked progress over the last decade. One of the cornerstones of this evolution was the application of the uniportal technique for lung resections. Initially, this approach was applied for simple wedge resections. With growing experience and development of special instruments, the uniportal approach was widespread throughout the whole world (1). Nowadays, spectrum of the uniportal minimally invasive approach includes all thoracic surgical procedures except for lung transplantation. Lobectomies, segmentectomies, complex trachea-bronchial and tracheal resections and reconstructions are performed by uniportal video-assisted thoracoscopic surgery (VATS) (1,2). Subxiphoid uniportal VATS for lung resections and resection of tumors of the anterior mediastinum represents a further development of the uniportal approach by reducing the pain caused by the intercostal irritation during conventional uniportal VATS.
Application of laser for lung-parenchyma sparing resections during open-surgical and minimally invasive thoracic procedures has been reported in several studies (3-5).
In the present case, we describe the subcostal uniportal video-assisted thoracoscopic resection of a lung nodule using the dual-wavelength diode laser. This case report was prepared in accordance with the CARE reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-55/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
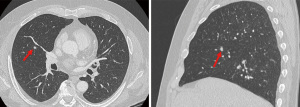
A 51-year-old male patient was admitted to our department due to suspect pulmonary lesions in the middle lobe. Six months earlier the patient was diagnosed for pancreatic head adenocarcinoma and received neoadjuvant chemotherapy. Prior to the planned pancreatic resection, re-staging computed tomography (CT) scan of the thorax revealed suspect pulmonary lesions in the middle lobe (Figure 1). Therefore, surgical evaluation of the pulmonary lesion was indicated.
Under general anesthesia, single-lung ventilation was initiated by a left-sided Robertshaw double-lumen endobronchial tube. The patient was placed in a left-sided lateral decubitus position using a vacuum mattress. An incision of 4 cm was performed parallel to the right costal arch (Figure 2, Video 1). The pleural cavity was entered through the subcostal space and a GelPOINT advanced access platform® (Applied Medical, Rancho Santa Margarita, CA, USA) was used (Figure 3) to enable a precise insertion and utilization of the laser probe, thereby minimalizing larger movements while applying the laser.
After inspection of the pleural cavity, the middle lobe was palpated, and a superficial lesion was detected. A wedge resection using the Endo Gia Universal Stapling System® (Medtronic, Minneapolis, MN, USA) was performed. Subsequently, the middle lobe was palpated thoroughly to identify the suspect lesion, as seen in the CT scan (Figure 1). The lesion was located close to the horizontal fissure and a pulmonary vein branch (Figure 1). After mobilization of the fissure, the lesion was palpated. Due to the location of the lesion, parenchyma-sparing resection using laser was performed. A dual-wavelength diode laser (LEONARDO® DUAL 100, Biolitec, Jena, Germany) was utilized. The lesion was enucleated with sufficient safety margins using the laser at a power level of 55 watts. After resecting the specimen, it was investigated macroscopically and sufficient resection margins were confirmed. Subsequently, lung parenchyma was sealed using the laser at a power level of 35 watts. A 28F chest tube was inserted through the subcostal incision and the right lung was re-ventilated showing a full re-expansion of the lung parenchyma. Skin closure was performed, and the chest tube was connected to a digital suction system (Thopaz+, Medela, Dietersheim, Germany). No air leakage was detected. The patient was extubated in the operation room and transferred to the normal ward. The postoperative course was uneventful. No postoperative pain was reported by the patient. Chest tube was removed on POD 3 and chest X-ray showed complete re-expansion of the lungs. The patient was discharged on POD 4 in good condition.
Histological examination revealed intrapulmonary lymph nodes without any signs of malignancy. Therefore, pancreatic resection was scheduled and successfully performed. The patient recovered well from surgery and is in complete remission.
Discussion
Application of laser in thoracic surgery is a well-established concept in pulmonary metastasectomy (3,6). The main advantages of the laser technique are enabling parenchyma-sparing resection of deep-located lesions and for lesions located near a major bronchus or vessel resection with sufficient safety margins may be performed without injury to these adjacent structures (6). Single-wavelength (1,318 nm) Nd:YAG (neodymium-doped yttrium aluminum garnet) laser is the most applied form of laser resection in thoracic surgery (3,4). The laser enables both resection and sealing of the lung tissue. However, both modes of action (resection, sealing) are controlled by the distance of the laser to the lung parenchyma. This results sometimes in less precise resections or sealing of the lung tissue, since distance to the lung tissue is a variable factor, which cannot be standardized easily. The newer generation of dual-wavelength diode laser (LEONARDO® DUAL 100, Biolitec) represent a valuable alternative to the single-wavelength laser. The combination of two wavelengths, 980 and 1,470 nm, enables a variety of tissue interactions. Each wavelength can be individually selected or combined to obtain the desired tissue effect such as incision, excision, vaporization, hemostasis and coagulation of soft tissue depending on the intraoperative situation. This laser is much compacter than the single-wavelength lasers which facilitates its application in different operating rooms and in a variety of fields, including thoracic surgery, phlebology, proctology, gynecology, and urology.
Conventional uniportal VATS offers limited exposure of the middle lobe. Endo-stapler assisted wedge resection are sometimes demanding due to the difficult angle obtained during conventional uniportal VATS, which is usually located at the 5th intercostal space. The subcostal approach offers an excellent exposure of the middle lobe and provides a good angle for endo-stapler or laser-assisted resections. A further advantage of the subcostal technique is reducing the pain caused by the intercostal irritation during conventional uniportal VATS.
Conclusions
In the present case, we applied the dual-wavelength diode laser during minimally invasive resection of a deep-located pulmonary nodule close to a branch of the pulmonary artery. This approach allowed for safe and precise parenchyma-sparing resection of the lung nodule, thereby enabling sufficient sealing of the lung tissue. The subcostal approach accounted for a quick postoperative recovery with no postoperative pain, thereby enabling excellent surgical site exposure.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-55/rc
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-55/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-55/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gonzalez-Rivas D, Yang Y, Ng C. Advances in Uniportal Video-Assisted Thoracoscopic Surgery: Pushing the Envelope. Thorac Surg Clin 2016;26:187-201. [Crossref] [PubMed]
- Reinersman JM, Passera E, Rocco G. Overview of uniportal video-assisted thoracic surgery (VATS): past and present. Ann Cardiothorac Surg 2016;5:112-7. [Crossref] [PubMed]
- Baier B, Kern A, Kaderali L, et al. Retrospective survival analysis of 237 consecutive patients with multiple pulmonary metastases from advanced renal cell carcinoma exclusively resected by a 1318-nm laser. Interact Cardiovasc Thorac Surg 2015;21:211-7. [Crossref] [PubMed]
- Kirschbaum A, Braun S, Rexin P, et al. Comparison of local tissue damage: monopolar cutter versus Nd:YAG laser for lung parenchyma resection. An experimental study. Interact Cardiovasc Thorac Surg 2014;18:1-6. [Crossref] [PubMed]
- Meyer C, Bartsch D, Mirow N, et al. Video-Assisted Laser Resection of Lung Metastases-Feasibility of a New Surgical Technique. Thorac Cardiovasc Surg 2017;65:382-6. [Crossref] [PubMed]
- Venuta F, Rolle A, Anile M, et al. Techniques used in lung metastasectomy. J Thorac Oncol 2010;5:S145-50. [Crossref] [PubMed]
Cite this article as: Kösek V, Thiel B, Al Masri E, Cenal U, Abuagrab N, Redwan B. Subcostal uniportal video-assisted thoracoscopic resection of a pulmonary nodule using a diode laser: a case report. J Vis Surg 2023;9:25.




