Endoscopic treatment of Zenker’s Diverticulum—the modified transoral approach
Introduction
Zenker’s diverticulum is a herniation of hypopharyngeal mucosa between the cricopharyngeus and inferior constrictor muscles. It is an uncommon but surgically treatable cause of dysphagia, and has a predilection for males over 70 years of age (1). Head and neck examination is usually unremarkable. In-office endoscopy may show increased pooling in the left pyriform sinus (2). Preoperative evaluation relies primarily on barium esophagography to confirm the diagnosis which reveals a pharyngeal pouch filling with contrast medium posterior to the cricopharyngeus muscle bar and the esophagus. Open surgical excision and endoscopic stapling are commonly employed to alleviate symptoms. In 2010, transoral laser—assisted partial myectomy of the cricopharyngeus muscle was described to improve symptom relief and decrease symptom recurrence (3). Also in 2010, Mortensen et al. detailed the technique of transoral resection of diverticula (TORD), wherein the sack itself is excised, not simply divided as in the classic stapler-assisted endoscopic approach (4). The modified transoral resection of diverticula (MTORD) is an endoscopic approach presented in this manuscript wherein a diverticulectomy is performed in conjunction with partial cricopharyngeal myectomy. MTORD affords a purely endoscopic approach for diverticulectomy, and avoids the morbidity of a transcervical approach. This paper describes the technique.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Stanford University Institutional Review Board (IRB number: 42705) and written informed consent was obtained from all patients. Patients are evaluated for unfavorable physical factors to diverticuloscope placement such as Mallampati class 3 or 4, class 2 occlusion, trismus, unstable dentition, and limited neck extension (5). Patients with these findings should be counseled pre-operatively for the possibility of conversion to an open transcervical approach in case an adequate endoscopic view of the diverticulum cannot be achieved. Additionally, patients should be counselled of the risk of conversion to the open approach if the procedure is complicated by pharyngeal perforation.
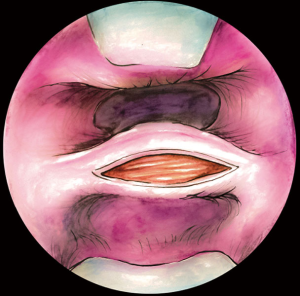
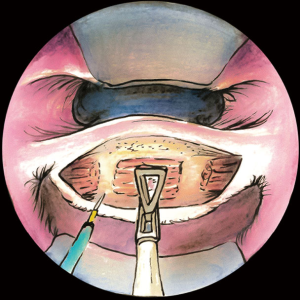
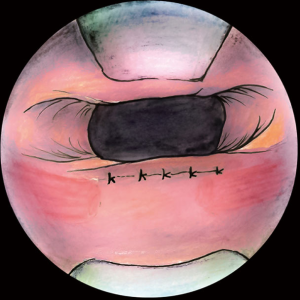
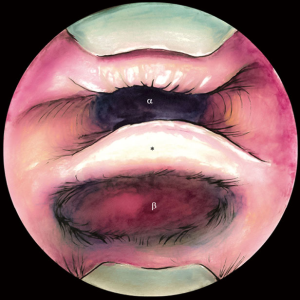
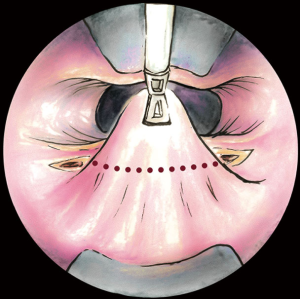
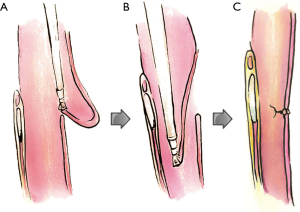
The patient is placed in the supine position. General anesthesia is induced and preoperative antibiotic prophylaxis is given, usually cefazolin. The patient is endotracheally intubated with a wire reinforced endotracheal tube. A shoulder roll is placed. The upper dentition is protected with a rubber dental guard. The procedure usually begins with esophagoscopy to exclude concomitant unexpected esophageal pathology. Once this is excluded, the Weerda distending diverticuloscope (Karl Storz, Tuttlingen, Germany) is then placed into position and suspended from a Dedo- Mayo stand to achieve clear visualization of the esophageal lumen, diverticulum and the cricopharyngeal bar (Figure 1). An operating microscope with attached micromanipulator is placed. CO2 laser or endoscopic electrocautery can be used. When a laser is chosen, we prefer to use a continuous power setting at 8 watts. The patient’s eyes are protected with wet gauze pads and the face is covered with wet towels. A horizontal incision is made in the mucosa to expose the cricopharyngeal bar (Figure 2). Submucosal flaps are elevated anteriorly, inferiorly and posteriorly to the cricopharyngeal bar (Figure 3). The full thickness of muscle is grasped, divided fully bilaterally and excised to the level of the distal connective tissue (Figure 4). Lateral incision are made parallel to the long axis of the diverticulum sack. It is then advanced inferiorly to gauge the degree of mucosa required for resection. Enough mucosa should be removed to obliterate the diverticular lumen but also to allow a tension free mucosal closure. The sack is then advanced inferiorly into the esophageal inlet, and the desired amount of tissue excised (Figure 5). Frequently, small blood vessels are encountered during the myectomy or diverticulectomy that may require electrocautery for hemostasis. A tension-free primary closure is performed in a horizontal fashion using interrupted 3-0 vicryl suture on an RB-1 needle (Ethicon, Inc.; Somerville, NJ) (Figure 6). Knots are tied externally and advanced with a knot pusher or triangular forceps. The closure should be performed in a tension free manner (Figure 7). A nasogastric feeding tube is then placed under direct visualization (Video 1).
Patients are observed for 48 hours postop. If there is no clinical indication of leakage (i.e., subcutaneous emphysema), patients are started on a liquid diet, which is advanced to a regular diet by postoperative day 7. A broad-spectrum antibiotic, delayed oral diet and continued tube feeding should be considered if there is clinical suspicion for a leak.
Results
Eighteen patients were treated in this fashion. Postoperative esophagram can confirm complete sack excision. To date no surgical complications have been observed with MTORD but theoretically include dental trauma, subcutaneous emphysema, mediastinitis, hypopharyngeal injury, bleeding, pharyngoesophageal stenosis, fistula, need for reoperation and persistent symptoms of dysphagia (6,7). We believe that mucosal closure tends to lower the incidence of these complications, and is an important part of the procedure (8,9).
Discussion
The mainstay of treatment of Zenker’s diverticulum has evolved from the conventional open, transcervical approach to the more popular transoral, endoscopic techniques with either rigid or flexible scopes due to the lower complication rates, faster recovery, shorter operative time and shorter hospital stay (10,11).
Endoscopic treatment of Zenker’s diverticula is conventionally performed by making a vertical myotomy through the cricopharyngeus muscle bar and dividing the common wall shared by the esophagus and the anterior diverticular sack. However, these techniques report higher stricture and recurrence rates than the cricopharyngeal myectomy technique (3). We favor this approach combined with a modification of the TORD procedure described by Mortensen (3,4). In this modified technique, a horizontal mucosal incision facilitates wider exposure of the cricopharyngeus muscle resection and facilitates the mucosal closure. Primary mucosal closure may mitigate pharyngeal leakage, subcutaneous emphysema and infection while facilitating pouch excision (8).
Inpatient observation and delayed resumption of oral alimentation are considered disadvantages of the endoscopic laser diverticulotomy when compared to the endoscopic stapling approach, which postoperatively allows immediate oral diet with no requirement of nasogastric feeding tube placement. However, Mortensen et al. reported resuming a liquid diet on the morning of the first post-operative day after transoral crycopharyngeal myotomy or TORD without any complications. Several patients in our experience have also started liquid intake after MTORD on post-operative day one without any complications. In addition, the endoscopic laser approach offers other advantages including complete pouch excision, lower complication rate compared to transcervical excision, greater improvement in dysphagia and regurgitation, and a lower rate of recurrence of symptoms and need for revision surgery (6,12).
Conclusions
MTORD is a safe and effective endoscopic treatment of Zenker’s diverticulum, affording diverticulectomy and myomectomy. Complication rates are comparable to stapling, and lower than conventional external excision. However, long-term recurrence rates need to be evaluated.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Douglas Z Liou) for the series “Advancement in Treatment for Esophageal Diseases” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs.2020.03.05/coif). The series “Advancement in Treatment for Esophageal Diseases” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Stanford University Institutional Review Board (IRB number: 42705) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roden DF, Altman KW. Causes of dysphagia among different age groups: a systematic review of the literature. Otolaryngol Clin North Am 2013;46:965-87. [Crossref] [PubMed]
- Ongkasuwan J, Yung KC, Courey MS. Pharyngeal stasis of secretions in patients with Zenker diverticulum. Otolaryngol Head Neck Surg 2012;146:426-9. [Crossref] [PubMed]
- Peretti G, Piazza C, Del Bon F, et al. Endoscopic treatment of Zenker's diverticulum by carbon dioxide laser. Acta Otorhinolaryngol Ital 2010;30:1-4. [PubMed]
- Mortensen M, Schaberg MR, Genden EM, et al. Transoral resection of short segment Zenker's diverticulum and cricopharyngeal myotomy: an alternative minimally invasive approach. Laryngoscope 2010;120:17-22. [Crossref] [PubMed]
- Damrose EJ, Ho AS. Endoscopic cricopharyngeal myotomy. Operative Tech Otol Head Neck Surg 2012;23:144-8. [Crossref]
- Parker NP, Misono S. Carbon dioxide laser versus stapler-assisted endoscopic Zenker's diverticulotomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2014;150:750-3. [Crossref] [PubMed]
- Verhaegen VJ, Feuth T, van den Hoogen FJ, et al. Endoscopic carbon dioxide laser diverticulostomy versus endoscopic staple-assisted diverticulostomy to treat Zenker's diverticulum. Head Neck 2011;33:154-9. [Crossref] [PubMed]
- Anagiotos A, Feyka M, Gostian AO, et al. Endoscopic laser-assisted diverticulotomy without versus with wound closure in the treatment of Zenker's diverticulum. Eur Arch Otorhinolaryngol 2014;271:765-70. [Crossref] [PubMed]
- Ho AS, Morzaria S, Damrose EJ. Carbon dioxide laser-assisted endoscopic cricopharyngeal myotomy with primary mucosal closure. Ann Otol Rhinol Laryngol 2011;120:33-9. [Crossref] [PubMed]
- Aiolfi A, Scolari F, Saino G, et al. Current status of minimally invasive endoscopic management for Zenker diverticulum. World J Gastrointest Endosc 2015;7:87-93. [Crossref] [PubMed]
- Orthopoulos G, Oriel BS, Siegert CJ, et al. Results of a Tailored Approach to Zenker's Diverticulum: A Single VA Experience. J Laparoendosc Adv Surg Tech A 2016;26:806-7. [Crossref] [PubMed]
- Pollei TR, Hinni ML, Hayden RE, et al. Comparison of carbon dioxide laser-assisted versus stapler-assisted endoscopic cricopharyngeal myotomy. Ann Otol Rhinol Laryngol 2013;122:568-74. [Crossref] [PubMed]
Cite this article as: Junlapan A, Boonipat T, Sung CK, Damrose EJ. Endoscopic treatment of Zenker’s Diverticulum—the modified transoral approach. J Vis Surg 2020;6:42.