Insertion of inflatable penile prosthesis into a neophallus (single cylinder)
Introduction
The aim of total phallic construction is to create an aesthetically acceptable and sensitivity phallus with an incorporated neo-urethra. It should allow the patient to empty into the upright position as performed by most males. However, it should have a sufficient size to accommodate a prosthesis that can guarantee sufficient rigidity for penetrative sexual relations (1-9).
One of the major challenges is to allow patients to reach a rigidity necessary for sexual penetration. This goal is made particularly difficult by the lack of an effective substitute for the corpora cavernosa in the phallic construction (10,11).
To date there is no agreement on what is the ideal method for implanting a penile prosthesis (PP) in a neophallus. In fact, even today the choice of the best method to achieve PP stability, prevent erosion and safely anchor the PP are a source of difficulty.
In this article we will demonstrate the technique we used to perform this procedure in detail.
Female to Male gender sexual reassignment is a complex multi-stage surgical challenge based on the creation of a functional and cosmetically acceptable phallus. The first stage is fashioning the neophallus. Different flaps can be adopted, but in this case we used a radial artery based forearm free flap (RAFFF). Once the phallus is made, the next step is the laparoscopic hysterectomy salpingo-oophorectomy, join up urethroplasty, vaginectomy, burying of the clitoris, glans sculpting, and scrotoplasty. PP implantation is performed as the last surgical procedure.
Before proceeding with a PP implantation, 1 year is the minimum time required to wait from the last operation on the phallus.
In this video we demonstrate a single cylinder PP insertion technique in RAFFF neophallus (Video 1). The PP can be inflatable or malleable and during the preoperative examination the number of cylinders to be implanted is decided based on the size and shape of the phallus and the patient’s preferences. The authors antibiotic prophylaxis preference is a single dose of Gentamicin and Amoxicillin/Clavulanic Acid 1.2 g administered at induction and a scrub of the operative field of at least 10 min with povidone-iodine is also performed.
Methods
This study is waived from ethical approval by the ethics committee or institutional review board. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Surgical technique
The first step of the procedure is the insertion of a urethral catheter with the help of an introducer after which an inguinal incision is performed.
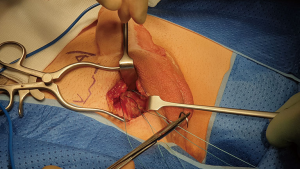
Pubis anchorage sutures positioning (00.41)
The incision was made and dissection of subcutaneous tissues to reach the pubic bone and all subcutaneous tissues retracted medially to expose the central aspect of the symphysis pubis.
To allow for anchoring of the prosthesis, were inserted three J-needle 0 Polyester (Ethibond™) sutures into the pubic bone (Figure 1).
The number and position of the anchoring sutures changes according to the number of cylinders implanted. In the case of a single cylinder two parallel sutures are positioned on one side and a single one on the contralateral side (as shown in the Figure 1). Two parallel rows approximately 2 cm apart for each cylinder. This can be repeated on the contralateral side if necessary.
Neophallus dilatation (01.46)
The space for inserting the prosthesis into the neophallus was initially formed using McIndoe’s scissors. This was done by using Hegar dilators of increasing size starting from 10 to size 22, in order to obtain sufficient space to position the cylinder and the polyethylene terephthalate (Dacron™) tip. During the dilatation, the urethral catheter should be palpable and moved securely away from the dilatation line so that the chances of performing a urethral lesion or extrusion of the prosthesis at a later date are minimized (Figure 2).
Formation of reservoir space (02.46)
An oblique incision is made in the lower right abdominal quadrant to perform the ectopic insertion of the reservoir. After exposing of the external obliquus muscle aponeurosis the muscles fibres are separated and an Hegar dilator is used in order to create space. An antibiotic soaked gauze is left in the space until the reservoir is ready for placement (Figure 3).
Measurement for cylinder length (03.10)
The choice of cylinder length is measured starting from the pubis up to the tip of the neophallus (Figure 4).
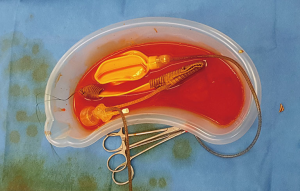
Preparation of the 3 pieces inflatable PP (03.16)
The neophallus lacks the native corpora, and therefore there is a risk of erosion and consequent infection or malfunction of the prosthesis cylinder that is inserted into the neophallus. This risk is reduced by fashioning a silver-coated Dacron™ covering for the tip of the cylinder and the base of the prosthesis extending up to the exit of the connection tubes to provide additional stability. Both cylinders can be inserted but in this video, only one cylinder is used. The other is cut and the tubing is secured with a true-lock connector (Figure 5). Once the prosthesis is prepared removing all the air from the device and the Dacron™ covering is secured to the cylinders, the implant is placed once again in the antibiotic solution.
Reservoir placement (07.37)
The reservoir was inserted into the previously prepared space and the tubes are passed deep to the lateral side of the fascia and brought out through the inguinal incision and secured using two shodded clips to prevent air from entering the system whilst protecting the tubing.
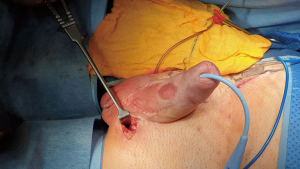
Testicular prosthesis insertion (07.52)
The testicular prosthesis is inserted into the scrotum through an opposite groin incision (Figure 6). Room for the testicular implant is made through the creation of a dartos pouch obtained by guided digital dilatation.
Insertion of the cylinder (08.13)
The Furlow introducer is used to deploy the needle and position the cylinder. The Dacron™ ‘sock’ (proximal end) is anchored to the pubis using the three Ethibond™ sutures placed at the start of the procedure. The device is then cycled.
Pump placement (10.07)
A right scrotal incision is made and the pump is placed in the right scrotal pouch following manual dilatation.
Final steps (10.40)
After flushing with saline solution, to ensure no air bubbles were introduced into the system, the tubes were connected and the socks removed before closing the incisions.
Results
Postoperative period (11.17)
On the first postoperative day the bladder catheter is removed and the patient was discharged with oral co-amoxiclav 625 mg three times/day for 5 days. One week later the PP was usually deflated in clinic. Three weeks later the patient was instructed on how to cycle the prosthesis, and encouraged to have penetrative sexual intercourse after 6 weeks.
Complications
The complications rate, type of revision surgery performed and long term results are summarised in Table 1 (12). When an infection or erosion occurs, all the components of the device were removed, including the Dacron sock and cap. A broad-spectrum antibiotic cover is given to the patient and a possible replacement of a prosthesis is offered at least 6 months later. In cases of mechanical failure, the defective component was identified and replaced intraoperatively. When the prosthesis showing problems and requiring revision has been implanted more than three years before, the replacement of the entire device is proposed to the patient. This is because the life expectancy of phalloplasty implants is much lower than those implanted in men with erectile dysfunction (11-18). The main causes of mechanical failure in our experience were cylinder breakage (69%), cylinder aneurysm (19%) and breakage of the connection pipe between the cylinder and the pump (12%).
Table 1
| Type of complication & long term results | % | Management |
|---|---|---|
| Type of complication | ||
| Infection of the device | 8.5 | Removal + delayed reimplantation |
| Mechanical failure | 15.4 | Replacement of the damaged component1 |
| Patient dissatisfaction | 48 | Repositioning of the cylinder(s) or insertion of a second cylinder |
| Long term results | ||
| 60% original prosthesis still IN-SITU at 10 years | ||
| 40% 10-year revision free survival | ||
1, revision surgery included exchange of the affected component only if the device was <3 years old, otherwise all components were exchanged.
Conclusions
In conclusion, with this video we wanted to show a standardized technique for inserting a PP into a neophallus. This surgical technique proved to be effective and reproducible with reasonable results in terms of function and safety. Despite this, is a very complex procedure with significant complication rates and should be performed only by experienced surgeons working in dedicated and high-volume centres.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Martin Gross, Jay Simhan and Faysal A. Yafi) for the series “Penile Prosthesis Surgery” published in Journal of Visualized Surgery. This article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs.2019.07.05/coif). The series “Penile Prosthesis Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study is waived from ethical approval by the ethics committee or institutional review board. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Garaffa G, Christopher NA, Ralph DJ. Total phallic reconstruction in female-to-male transsexuals. Eur Urol 2010;57:715-22. [Crossref] [PubMed]
- Doornaert M, Hoebeke P, Ceulemans P, et al. Penile reconstruction with the radial forearm flap: an update. Handchir Mikrochir Plast Chir 2011;43:208-14. [Crossref] [PubMed]
- Falcone M, Garaffa G, Raheem A, et al. Total Phallic Reconstruction Using the Radial Artery Based Forearm Free Flap After Traumatic Penile Amputation. J Sex Med 2016;13:1119-24. [Crossref] [PubMed]
- Garaffa G, Raheem AA, Christopher NA, et al. Total phallic reconstruction after penile amputation for carcinoma. BJU Int 2009;104:852-6. [Crossref] [PubMed]
- Perović S. Phalloplasty in children and adolescents using the extended pedicle island groin flap. J Urol 1995;154:848-53. [Crossref] [PubMed]
- Garaffa G, Spilotros M, Christopher NA, et al. Total phallic reconstruction using radial artery based forearm free flap phalloplasty in patients with epispadias-exstrophy complex. J Urol 2014;192:814-20. [Crossref] [PubMed]
- Massanyi EZ, Gupta A, Goel S, et al. Radial forearm free flap phalloplasty for penile inadequacy in patients with exstrophy. J Urol 2013;190:1577-82. [Crossref] [PubMed]
- Perovic SV, Djinovic R, Bumbasirevic M, et al. Total phalloplasty using a musculocutaneous latissimus dorsi flap. BJU Int 2007;100:899-905; discussion 905. [Crossref] [PubMed]
- Bouman FG. The first step in phalloplasty in female transsexuals. Plast Reconstr Surg 1987;79:662-4. [Crossref] [PubMed]
- Bogoras N. Uber die volle plastische wiederherstellung eines zum koitus fahigen penis (peniplastica totalis). Zentralbl Chir 1936;63:1271.
- Hage JJ, Bloem JJ, Bouman FG. Obtaining rigidity in the neophallus of female-to-male transsexuals: a review of the literature. Ann Plast Surg 1993;30:327-33. [Crossref] [PubMed]
- Falcone M, Garaffa G, Gillo A, et al. Outcomes of inflatable penile prosthesis insertion in 247 patients completing female to male gender reassignment surgery. BJU Int 2018;121:139-44. [Crossref] [PubMed]
- Hoebeke P, De Cuypere G, Ceulemans P, et al. Obtaining rigidity in total phalloplasty: experience with 35 patients. J Urol 2003;169:221-3. [Crossref] [PubMed]
- Hoebeke PB, Decaestecker K, Beysens M, et al. Erectile implants in Female-to-Male transsexuals: our experience in 129 patients. Eur Urol 2010;57:334-40. [Crossref] [PubMed]
- Carson CC, Mulcahy JJ, Govier FE. Efficacy, safety and patient satisfaction outcomes of the AMS 700CX inflatable penile prosthesis: results of a long-term multicenter study. AMS 700CX Study Group. J Urol 2000;164:376-80. [Crossref] [PubMed]
- Levine LA, Zachary LS, Gottlieb LJ. Prosthesis placement after total phallic reconstruction. J Urol 1993;149:593-8. [Crossref] [PubMed]
- Henry GD, Donatucci CF, Conners W, et al. An Outcomes Analysis of over 200 Revision Surgeries for Penile Prosthesis Implantation: A Multicenter Study. J Sex Med 2012;9:309-15. [Crossref] [PubMed]
- Levine LA, Estrada CR, Morgentaler A. Mechanical reliability and safety of, and patient satisfaction with the Ambicor inflatable penile prosthesis: results of a 2 center study. J Urol 2001;166:932-7. [Crossref] [PubMed]
Cite this article as: Ralph DJ, Chiriaco G, Venturino L, Falcone M, Satchi M, Christopher N. Insertion of inflatable penile prosthesis into a neophallus (single cylinder). J Vis Surg 2020;6:38.