
Aortic valve sparing techniques: pearls and pitfalls
“Aortic valve sparing” (AVS) operations were developed with the aim of preserving the native and functionally intact aortic valve in the aneurysmal disease of the aortic root. These procedures are known as the “reimplantation” technique, introduced by T. David (1) and the “remodeling” technique, described by Sir M. Yacoub (2) in the early 1990s. However, despite 30 years of experience of AVS, disorientation still exists on the strengths and weaknesses of the two AVS operations. Over the past decades fundamental advancements have occurred in the field of aortic valve repair, such as the clarification of AVS techniques, establishment of a classification system for aortic insufficiency (AI) and specific surgical approaches to cusp disease with bicuspid or tricuspid anatomy (3).
The basic concept of both procedures is to eliminate the aortic root aneurysm and recovering the function of the aortic valve. In the early iterations of these procedures, the remodeling operation aims to replace the sinuses of Valsalva with a tubular Dacron graft shaped in a three-tongue fashion; the edges of the graft are then sewn to the crown-shaped annulus and the 1-to-2-centimeter remnant of the aortic sinus. The remodeling operation needs a careful suturing between the graft and the valve and aortic remnants. In particular, to limit the risk of bleeding it is paramount to anchor the graft exactly at the crown-shaped cusp insertion where the border is composed mostly of fibrous tissue. It is fundamental to keep in mind that this anastomosis is directly exposed to the open pericardium and may lead to small bleedings which are not easy to treat when the aorta is closed and under pressure. Moreover, this anastomosis is exposed to great tension and a watertight suture is of primary importance. The remodeling procedure was originally conceived to nicely recreate the geometry of the root; but it did not address the aortic annulus and in some patients led to “splaying of the graft tongues” over time with development of AI as a consequence of loss of central leaflet coaptation.
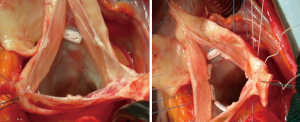
On the other hand, in the classic reimplantation procedure a Dacron cylinder is placed around the aortic root complex to completely enclose it rather than sitting atop of it. Therefore, with one maneuver it corrects annular ectasia in addition to dilatation of the sino-tubular junction. The reimplantation fixes the graft proximally at the virtual basal ring (VBR) below the leaflets and the commissure are sewn inside the prosthetic conduit. This explains the rationale for an accurate root dissection in order to be really able to “pull” the valve out of the heart and reach the level of the VBR from the external wall of the root (Figure 1). The suture of the remnants of the aortic root into the Dacron allows optimal support for the aortic wall and reduces the chance of bleeding.
However, from a theoretical point of view the main issue with the classic reimplantation is the elimination of Valsalva’s sinuses that are involved in leaflets motion. The theoretic standpoints favoring the use of grafts with re-creation of pseudo-sinuses encompass, among other reasons, decreased closing velocities of the aortic leaflets, reduced diastolic stresses on the cusps, therefore a potentially enhanced valve durability (4-6). Nevertheless, long-term results of classic reimplantation technique without sinuses also demonstrate long-term good results (7,8). However, over the time the reimplantation technique has been modified towards the re-creation of sinuses, therefore it is difficult to draw definite conclusions. With this concept in mind, a Dacron conduit designed specifically for aortic root operation was introduced by our group in the early 2000. This graft, called the “Valsalva” graft (Vascutek, Terumo) has been our choice for AVS since the beginning of our experience (9). Since then, for reimplantation procedure we followed the key steps first described by David, but we introduced some details necessary to adapt the graft to each “patient’s aortic valve” (Figure 2).

Besides the key role of the sinuses, the importance of re-establishing a normal geometry and dimension of the valve inside the reconstructed root has appeared as the most important single step for a long-lasting optimal result. In particular likewise in mitral valve diseases, the annuloplasty is efficient in re-establishing the dilated aortic annulus which is often part of the problem. It goes without saying that a stable annuloplasty become even more important in cases of evident annular ectasia, such as in patients with diseases of the connective tissue.
However, it has to be emphasized that, independently on the preferred procedure, remodeling or reimplantation, it is paramount to normalize cusp configuration and cusp geometry. In fact, when suturing the Dacron to the valve remnant, attention must be paid not to distort the orientation and distance of the commissures (2 or 3 depending on the valve phenotype). The distortion may indeed provoke leaflet prolapse that will need to be treated to avoid any early residual AI with an eccentric jet. In order to standardize the assessment of leaflet prolapse and cusp configuration, the use of the caliper is recommended. Using the effective height of 9–10 mm as a reference for an expected normal coaptation, helps in identifying and correct the possible leaflets prolapse (11). The simple shortening of the leaflets free margin can eliminate the tissue redundancy and normalize cusp geometry. On this topic, the use of central plicating sutures at the level of the nodule of Arantio appears easy to apply and reproducible. Moreover, the central part of aortic leaflets is exposed to less stress in comparison to the portion close to the commissure due to the opening and closing motion which leads to a higher stress. Employing a fine polytetrafluoroethylene (PTFE) suture along the length of the free margin to reduce its length is an alternative method, however it is more difficult, less reproducible, and slightly less accurate to perform.
The two valve sparing procedures are not competitive to each other; for aortic root aneurysm with normal annulus [ventriculo-aortic junction (VAJ) <26 mm] the remodeling could be preferred because annular diameter remains stable over time, when the aortic valve is competent.
In young patients and genetic syndromes with dilatated annulus (VAJ >28–30 mm) the reimplantation has proven to be highly effective with excellent long-term outcomes. The reimplantation procedure is generally preferred for its intrinsic ability to reduce and stabilize the annulus diameter, while the addition of some form of annuloplasty is becoming more frequent for those who prefer the remodeling technique. Over the past years AVS techniques have been significantly improved, therefore nowadays it is feasible to perform a reimplantation procedure with a vascular graft with pseudo-sinuses (12-14) or a remodeling technique with annular stabilization (15,16). For the associated annuloplasty there are mostly two different options. The one proposed by Schäfers et al. (17) consists of an external annuloplasty with a CV-0 PTFE suture placed from outside the aortic wall, under the coronaries, at the level of the VBR in a circumferential fashion and tighten around a Hegar dilator of an appropriate size (frequently 23 to 25 mm). This annuloplasty requires limited root dissection and shorter time to be performed, therefore is an appealing option. The other option is an external ring as proposed by Lansac (18), or a strip of Dacron, Teflon or similar material that are fixed to the annulus with a series of pledgeted sutures passed below the aortic valve similarly to the technique used for the reimplantation. Soft fabric such as Dacron or Teflon for external annuloplasty, if compared to less flexible rings, adapt better to the heart tissue in particular at the right coronary sinus where the presence of right ventricular muscle acts as a barrier to properly reach the level of the VBR.
AVS procedures are safe in terms of operative mortality and long-term survival: data from the current literature indeed, report a mortality rate from 0% to 10% and a 10-year survival around 90%, which is comparable to standard aortic valve surgery. The major issue is therefore the long-term durability of the spared valves in terms of recurrence of AI and freedom from reintervention. Current data on the long-term follow-up (>10 years) report a freedom from AI and from reoperation around 90%. Small discrepancies in the outcomes may depend on the single center experience or the chosen technique (8,12,15,16,19).
Overall, the outcomes are satisfactory in particular considering the relatively “young age” of these procedures. Suboptimal results may depend on a wrong patient selection, a failure to correct lesions on the leaflet, or an incorrect surgical procedure that distorts the geometry of the valve. AVS procedures resulting in a more than trivial and central regurgitation early after the operation, will invariably lead to a later reoperation. As warranty of a long-lasting valve function, it is fundamental to achieve a satisfactory coaptation height inside the reconstructed aortic root.
The key-points to achieving long-lasting AVS have become clearer over the last years. The disparity between the two technique have narrowed and today both comprise a physiological root reconstruction and prolonged long-term durability. The choice for reimplantation technique is founded on the impression of a better standardization of the surgical technique, a lower risk of surgical bleeding and larger amount of data on favorable long-term results. Even if it is useful to be acquainted with both remodeling or reimplantation procedures, it is suggested to perform routinely 1 of the 2 techniques and get familiar with all the “tips and tricks” which are fundamental to achieve good and stable reproducibility of the results. It is not advisable switching before having mastered one of the two approaches.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Filip Casselman and Johan van der Merwe) for the series “Aortic and Mitral Valve Innovative Surgery” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.09.02). The series “Aortic and Mitral Valve Innovative Surgery” was commissioned by the editorial office without any funding or sponsorship. RDP reports other from Terumo Aortic, during the conduct of the study; in addition, RDP has a patent Valsalva Graft with royalties paid. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg 1992;103:617-21; discussion 622. [PubMed]
- Yacoub MH, Fagan A, Stassano P, et al. Results of valve conserving operations for aortic regurgitation. Circ J 1983;68:311-21.
- Boodhwani M, de Kerchove L, Glineur D, et al. Repair-oriented classification of aortic insufficiency: impact on surgical techniques and clinical outcomes. J Thorac Cardiovasc Surg 2009;137:286-94. [Crossref] [PubMed]
- Grande-Allen KJ, Cochran RP, Reinhall PG, et al. Re-creation of sinuses is important for sparing the aortic valve: a finite element study. J Thorac Cardiovasc Surg 2000;119:753-63. [Crossref] [PubMed]
- De Paulis R, De Matteis GM, Nardi P, et al. Opening and closing characteristics of the aortic valve after valve-sparing procedures using a new aortic root conduit. Ann Thorac Surg 2001;72:487-94. [Crossref] [PubMed]
- De Paulis R, De Matteis GM, Nardi P, et al. Analysis of valve motion after the reimplantation type of valve-sparing procedure (David I) with a new aortic root conduit. Ann Thorac Surg 2002;74:53-7. [Crossref] [PubMed]
- Shrestha ML, Beckmann E, Abd Alhadi F, et al. Elective David I Procedure Has Excellent Long-Term Results: 20-Year Single-Center Experience. Ann Thorac Surg 2018;105:731-8. [Crossref] [PubMed]
- David TE, Feindel CM, David CM, et al. A quarter of a century of experience with aortic valve-sparing operations. J Thorac Cardiovasc Surg 2014;148:872-9; discussion 879-80. [Crossref] [PubMed]
- De Paulis R, De Matteis GM, Nardi P, et al. A new aortic Dacron conduit for surgical treatment of aortic root pathology. Ital Heart J 2000;1:457-63. [PubMed]
- De Paulis R, Scaffa R, Salica A, et al. Reimplantation procedure with the Valsalva graft. Asvide 2019;6:257. Available online: http://www.asvide.com/watch/32942
- Schäfers HJ, Bierbach B, Aicher D. A new approach to the assessment of aortic cusp geometry. J Thorac Cardiovasc Surg 2006;132:436-8. [Crossref] [PubMed]
- De Paulis R, Chirichilli I, Scaffa R, et al. Long-term results of the valve reimplantation technique using a graft with sinuses. J Thorac Cardiovasc Surg 2016;151:112-9. [Crossref] [PubMed]
- Tasca G, Lindner J, Barandon L, et al. Aortic root surgery with the CARDIOROOT vascular graft: results of a prospective multicenter post-market surveillance study. J Cardiothorac Surg 2019;14:94. [Crossref] [PubMed]
- Schmidtke C, Sievers HH, Frydrychowicz A, et al. First clinical results with the new sinus prosthesis used for valve-sparing aortic root replacement. Eur J Cardiothorac Surg 2013;43:585-90. [Crossref] [PubMed]
- Lansac E, Di Centa I, Sleilaty G, et al. Remodeling root repair with an external aortic ring annuloplasty. J Thorac Cardiovasc Surg 2017;153:1033-42. [Crossref] [PubMed]
- Schneider U, Feldner SK, Hofmann C, et al. Two decades of experience with root remodeling and valve repair for bicuspid aortic valves. J Thorac Cardiovasc Surg 2017;153:S65-71. [Crossref] [PubMed]
- Aicher D, Schneider U, Schmied W, et al. Early results with annular support in reconstruction of the bicuspid aortic valve. J Thorac Cardiovasc Surg 2013;145:S30-4. [Crossref] [PubMed]
- Lansac E, Di Centa I, Varnous S, et al. External aortic annuloplasty ring for valve-sparing procedures. Ann Thorac Surg 2005;79:356-8. [Crossref] [PubMed]
- Mastrobuoni S, de Kerchove L, Navarra E, et al. Long-term experience with valve-sparing reimplantation technique for the treatment of aortic aneurysm and aortic regurgitation. J Thorac Cardiovasc Surg 2019;158:14-23. [Crossref] [PubMed]
Cite this article as: De Paulis R, Scaffa R, Salica A, Weltert L, Guerrieri Wolf L, Folino G. Aortic valve sparing techniques: pearls and pitfalls. J Vis Surg 2019;5:74.


