Multimodal pain management strategies in penile implant recipients
Introduction
Penile surgeries, especially the insertion of a penile prosthesis can be associated with exquisite peri-operative discomfort and pain. Most commonly, opioids were used and prescribed to alleviate perioperative pain. However, narcotics have a well-demonstrated addictive potential and can lead to undesirable side effects such as constipation, drowsiness and urinary retention. Many contend that the recent opioid crisis in the United States has been fueled in part by the over-prescription of narcotics by medical professionals (1,2).
It is well recognized that there are multiple different pathways for the treatment of pain and multimodal analgesic (MMA) protocols have been suggested to alleviate pain and discomfort for a variety of surgical procedures (3). Although MMA protocols have been discussed elsewhere, there remains a paucity of data regarding its effect on pain reduction in urologic surgery recipients. In fact, MMA protocols have most clearly been assessed in radical cystectomy recipients but the focus of these investigations often centers on hospital length of stay and not pain reduction (4-12). As such, aside from opioids, other classes of medications such as non-steroid anti-inflammatory (NSAIDs), acetaminophen and gabapentinoids are often used as a part of MMA/enhanced recovery after surgery (ERAS) protocols. Additionally, as it relates to genital procedures, various types of penile blocks have been suggested used as well.
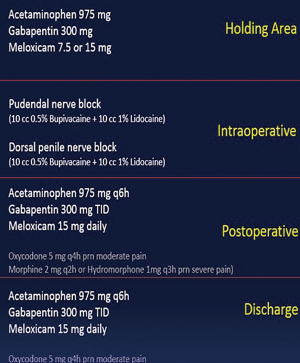
At our institution, a novel multi-modal analgesic protocol was developed (Figure 1) and utilized in penile implant recipients demonstrating dramatic reduction in pain following surgery. This multi-agent protocol spans the entire surgical time period, including the pre-, intra- and postoperative period. The results were published previously (13) and a multi-institutional study utilizing the same MMA protocol and rigorously assessing pain reduction is currently underway. A thorough review of the various agents utilized for pain reduction with penile implant recipients is discussed in this review with a focus on the recently described novel MMA protocol.
Basic principles and recommendations
MMA protocols involve various medications that target the various different components of the pain pathway and work synergistically to treat acute pain and maximize patient comfort (14,15). The following describes the basic description/information of medications commonly used as part of the ERAS/MMA pain management strategies. Some of these medications are administered preoperatively for preemptive oral analgesia with the aim to decrease production of inflammatory mediators that could sensitize nociceptors.
Commonly utilized medications
Non-steroidal anti-inflammatory drugs
NSAIDs act as potent inhibitors of prostaglandin and cyclooxygenase (COX) synthesis (16). Some examples of commonly used NSAIDs are ibuprofen, meloxicam and toradol. This class of medications, however, can be associated with adverse effects such as renal impairment and gastrointestinal ulcers (17,18). Regardless, meta-analyses have demonstrated the utilization of NSAIDs in patients with pre-existing normal renal function to not cause future renal impairment (18). As such, NSAIDs should be used with caution in those with pre-existing kidney impairment or gastrointestinal ulcers. In the recently described novel MMA protocol for penile implant patients, patients received either 7.5 or 15 mg oral meloxicam prior to induction of anesthesia and continued on meloxicam 7.5 or 15 mg daily postoperatively (13).
Acetaminophen
While the exact mechanism of acetaminophen remains under investigation, it has been shown to selectively inhibit COX activities in the brain and thus reduce pain (19). Notably, it carries a risk of hepatotoxicity and should be used with caution in those with liver disease (20). Acetaminophen comes in both intravenous and oral formulations. As part of our MMA protocol, patients received 975 mg of oral acetaminophen prior to induction of anesthesia and continued to receive acetaminophen 975 mg 4 times a day post-operatively (13).
Gabapentinoids
Gabapentin is a gabapentinoids that modulates GABA receptors centrally to modulate nociceptors in the spinal cord and brain (21,22). In our protocol, patients received 300 mg oral gabapentin prior to induction of anesthesia. Post-operatively, patients received 300 mg oral gabapentin 3 times a day around the clock (13).
Opioids
Narcotic medications are probably one of the most commonly used medications for peri-operative pain control. Opioids relieve pain by acting as an agonist on µ, κ and/or δ receptors (23,24). As part of our protocol, patients received no narcotics pre-operatively. Post-operatively, oxycodone was prescribed 5 mg every 4 hours as needed for moderate pain. Additionally, patients were prescribed morphine 2 mg every 2 hours as needed for severe pain (13).
Many local anesthetics had also been incorporated into MMA protocols to reduce post-operative pain/discomfort. Commonly used anesthetic agents and penile nerve blocks are described below.
Local anesthetics
Anesthetic agents
Lidocaine and bupivacaine are two of the commonly used anesthetic agents for penile blocks. Lidocaine works by prolonging the inactivation of the fast voltage-gated Na+ channels in the neuronal cell membrane (25). It has a shorter onset of action that aims to provide immediate pain relief. Similar to lidocaine, bupivacaine also works on voltage-gated sodium channels and blocks sodium influx into nerve cells; it can achieve up to 3 hours of action and perhaps prevent pain sensitization. Previous studies have shown local penile blocks utilizing lidocaine alone or in combination with bupivacaine to reduce pain from penile prosthesis placement (26-30).
Penile blocks
Dorsal penile nerve block
The dorsal penile nerve is a branch of the pudendal nerve and provides sensation to penile skin. It courses just lateral to the deep dorsal arteries and vein within Buck’s fascia. A dorsal penile nerve block has shown to reduce immediate post-operative pain for those undergoing penile surgeries (31). It is performed by inserting the needle in between the base of the penis and suspensory ligament. Additionally, locals were injected at the 2- and 10-o’clock position for right and left dorsal penile nerves. Intraoperatively, prior to incision, an 18 gauge ×1.25 in (3.18 cm) needle connected to a 20-cc syringe was used to inject a 20-cc local anesthetic of 50/50 mixture of 1% lidocaine and 0.5% bupivacaine without epinephrine. The technique is demonstrated in Figure 2.
Pudendal nerve block
The pudendal nerve originates in the S2–S4 nerve root and exits through the greater sciatic foramina. It then crosses the posterior aspect of the sacrospinous ligament at the level of the ischial spine, re-enters the pelvis through the lesser sciatic foramina, and courses through Alcock’s canal. Pudendal nerve blocks have been shown to reduce postoperative pain urologic surgeries such as urethroplasty and penile prosthesis placement (28,33). For our protocol, intraoperatively, prior to incision, an 18 gauge ×1.25 in (3.18 cm) needle connected to a 20-cc syringe was used to inject a 20-cc local anesthetic of 50/50 mixture of 1% lidocaine and 0.5% bupivacaine without epinephrine into the Alcock’s canal. The penile nerve distribution of the pudendal nerve was targeted. This technique is also demonstrated in Figure 2.
Crural nerve block
Cavernous nerves are post-ganglionic parasympathetic nerves that arise from cell bodies in the inferior hypogastric plexus where they receive the pre-ganglionic pelvic splanchnic nerves (S2–S4). A block targeting this nerve was described by Hsu and colleagues as inserting a needle at a 45-degree angle oblique to the coronal plane approximately 1.5 fingerbreadths below the penoscrotal junction. When used in combination with a penile dorsal nerve block, they reported similar pain control when compared to pudendal block alone (30).
Ring block
This block was initially developed to reduce pain from circumcision, however, it has been shown previously to be adequate for pain control in a cohort of 159 patients of patient who underwent penile prosthesis (27). It is performed by injection of local agents in the infrapubic space followed by subcutaneous penile ring infiltration at the base of the penile shaft.
Conclusions
Penile prosthesis insertion is associated with significant perioperative pain and discomfort. Adequate pain control will not only alleviate patient discomfort but also aide in patient satisfaction and potentially device success. MMA protocols involving different drugs targeting various pain pathways have been shown to be effective in not only decreasing narcotics usage but also providing excellent pain reduction in the recovery period.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Visualized Surgery for the series “Penile Prosthesis Surgery”. The article has undergone external peer review.
Conflicts of Interest: The series “Penile Prosthesis Surgery” was commissioned by the editorial office without any funding or sponsorship. JS served as the unpaid Guest Editor of the series. Senior author is a paid consultant of Boston Scientific and Coloplast Corp. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Vital Statistics System. Mortality Multiple Cause-of-Death: 2016 Mortality. Available online: https://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm. [Accessed 4 February 2018].
- Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research (WONDER). Available online: http://wonder.cdc.gov. [Accessed 4 February, 2018].
- American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248-73. [Crossref] [PubMed]
- Baack Kukreja JE, Kiernan M, Schempp B, et al. Quality Improvement in Cystectomy Care with Enhanced Recovery (QUICCER) study. BJU Int 2017;119:38-49. [Crossref] [PubMed]
- Arumainayagam N, McGrath J, Jefferson KP, et al. Introduction of an enhanced recovery protocol for radical cystectomy. BJU Int 2008;101:698-701. [Crossref] [PubMed]
- Saar M, Ohlmann CH, Siemer S, et al. Fast-track rehabilitation after robot-assisted laparoscopic cystectomy accelerates postoperative recovery. BJU Int 2013;112:E99-106. [Crossref] [PubMed]
- Daneshmand S, Ahmadi H, Schuckman AK, et al. Enhanced recovery protocol after radical cystectomy for bladder cancer. J Urol 2014;192:50-5. [Crossref] [PubMed]
- Pruthi RS, Nielsen M, Smith A, et al. Fast track program in patients undergoing radical cystectomy: results in 362 consecutive patients. J Am Coll Surg 2010;210:93-9. [Crossref] [PubMed]
- Dutton TJ, Daugherty MO, Mason RG, et al. Implementation of the Exeter enhanced recovery programme for patients undergoing radical cystectomy. BJU Int 2014;113:719-25. [Crossref] [PubMed]
- Karl A, Buchner A, Becker A, et al. A new concept for early recovery after surgery for patients undergoing radical cystectomy for bladder cancer: results of a prospective randomized study. J Urol 2014;191:335-40. [Crossref] [PubMed]
- Maffezzini M, Campodonico F, Capponi G, et al. Fast-track surgery and technical nuances to reduce complications after radical cystectomy and intestinal urinary diversion with the modified Indiana pouch. Surg Oncol 2012;21:191-5. [Crossref] [PubMed]
- Smith J, Meng ZW, Lockyer R, et al. Evolution of the Southampton Enhanced Recovery Programme for radical cystectomy and the aggregation of marginal gains. BJU Int 2014;114:375-83. [PubMed]
- Tong CMC, Lucas J, Shah A, et al. Novel Multi-Modal Analgesia Protocol Significantly Decreases Opioid Requirements in Inflatable Penile Prosthesis Patients. J Sex Med 2018;15:1187-94. [Crossref] [PubMed]
- Elia N, Lysakowski C, Tramer MR. Does multimodal analgesia with acetaminophen, nonsteroidal anti-inflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology 2005;103:1296-304. [Crossref] [PubMed]
- McDaid C, Maund E, Rice S, et al. Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: a systematic review. Health Technol Assess 2010;14:1-153. iii-iv. [Crossref] [PubMed]
- Noble S, Balfour JA. Meloxicam. Drugs 1996;51:424-30, discussion 431-2. [Crossref] [PubMed]
- Rostom A, Dube C, Wells G, et al. Prevention of NSAID-induced gastroduodenal ulcers. Cochrane Database Syst Rev 2002;CD002296 [PubMed]
- Lee A, Cooper MG, Craig JC, et al. Effects of nonsteroidal anti-inflammatory drugs on postoperative renal function in adults with normal renal function. Cochrane Database Syst Rev 2007;CD002765 [PubMed]
- Ghanem CI, Pérez MJ, Manautou JE, et al. Acetaminophen from liver to brain: New insights into drug pharmacological action and toxicity. Pharmacol Res 2016;109:119-31. [Crossref] [PubMed]
- Larson AM, Polson J, Fontana RJ, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology 2005;42:1364-72. [Crossref] [PubMed]
- Wick EC, Grant MC, Wu CL. Postoperative Multimodal Analgesia Pain Management With Nonopioid Analgesics and Techniques: A Review. JAMA Surg 2017;152:691-7. [Crossref] [PubMed]
- Mishriky BM, Waldron NH, Habib AS. Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. Br J Anaesth 2015;114:10-31. [Crossref] [PubMed]
- Ordóñez Gallego A, González Barón M, Espinosa Arranz E. Oxycodone: a pharmacological and clinical review. Clin Transl Oncol 2007;9:298-307. [Crossref] [PubMed]
- Pathan H, Williams J. Basic opioid pharmacology: an update. Br J Pain 2012;6:11-6. [Crossref] [PubMed]
- Catterall WA. Molecular mechanisms of gating and drug block of sodium channels. Novartis Found Symp 2002;241:206-18; discussion 218-32. [PubMed]
- Cotta BH, Welliver C, Brahmamdam A, et al. Long-acting liposomal bupivacaine decreases inpatient narcotic requirements in men undergoing penile prosthesis implantation. Turk J Urol 2016;42:230-4. [Crossref] [PubMed]
- Ghanem H, Fouad G. Penile prosthesis surgery under local penile block anaesthesia via the infrapubic space. Int J Androl 2000;23:357-9. [Crossref] [PubMed]
- Park SS, Wilson SK, Valenzuela RJ. Subcoronal IPP can be performed under local anesthesia. Presented at the 21st Annual Fall Scientific Meeting of SMSNA, Las Vegas, USA, November 19-22, 2015.
- Dos Reis JM, Glina S, Da Silva MF, et al. Penile prosthesis surgery with the patient under local regional anesthesia. J Urol 1993;150:1179-81. [Crossref] [PubMed]
- Hsu GL, Hsieh CH, Wen HS, et al. Outpatient penile implantation with the patient under a novel method of crural block. Int J Androl 2004;27:147-51. [Crossref] [PubMed]
- Raynor MC, Smith A, Vyas SN, et al. Dorsal penile nerve block prior to inflatable penile prosthesis placement: a randomized, placebo-controlled trial. J Sex Med 2012;9:2975-9. [Crossref] [PubMed]
- Lee AS, Foote C, Simhan J. Multimodal analgesic for andrology procedures. Asvide 2019;6:242. Available online: http://www.asvide.com/watch/32927
- Kalava A, Pribish AM, Wiegand LR. Pudendal nerve blocks in men undergoing urethroplasty: a case series. Rom J Anaesth Intensive Care 2017;24:159-62. [PubMed]
Cite this article as: Lee AS, Foote C, Simhan J. Multimodal pain management strategies in penile implant recipients. J Vis Surg 2019;5:71.