Subxiphoid single-port pulmonary bilateral metastasectomy
Introduction
In the field of thoracic surgery, medical technology and surgical procedures are progressing, and there is a shifting trend toward minimally invasive surgery.
Recently, video-assisted thoracoscopic surgery (VATS) is a minimally invasive procedure in the field of thoracic surgery, has been performed in conventional multi-port surgery and has also enabled single-port surgery, in which all manipulations are performed via a single wound. Single-port surgery for pulmonary wedge resection was reported by Rocco et al. in 2004, and single-port lobectomy was reported by Gonzalez-Rivas et al. in 2011. Furthermore, based on the results of these groups, single-port surgery is indicated for surgery associated with a higher degree of difficulty, such as pulmonary angioplasty and sleeve resection (1-4). Recently, the subxiphoid approach has been used in thoracic surgery. In 1999, Kido et al. reported thymectomy via the subxiphoid approach (5). They inserted the Laparolift system (Origin Medsystems Inc., Santa Clara, USA) via a subxiphoid wound, and by lifting the sternum, they ensured the working space behind the sternum. Furthermore, in 2000, Mineo et al. performed hand-assisted thoracoscopic surgery, in which bilateral pulmonary wedge resection was performed, while directly palpating the lung with the hand inserted via a subxiphoid wound (6). In 2012, we reported on single-port thymectomy via the subxiphoid approach (subxiphoid single-port thymectomy). In this approach, carbon dioxide (CO2) is insufflated through a single subxiphoid wound to ensure the operative visual field for thymus removal. In 2014, we reported on subxiphoid single-port bilateral pulmonary metastasectomy via the same approach (7,8). This approach, in which all manipulations are performed through a 3-cm single wound in the epigastric fossa, enables one-stage bilateral pulmonary resection with the patient maintained in the supine position, and because the intercostal space is not involved, it does not cause intercostal neuralgia. It is a useful approach that enables minimally invasive surgery for patients who require surgery of bilateral lungs, such as bilateral metastatic pulmonary tumors and bilateral spontaneous pneumothorax. Herein we describe the surgical method of the subxiphoid single-port pulmonary bilateral metastasectomy and associated tips, tricks, and pitfalls.
Patient selection
Resectable metastatic pulmonary tumors located in the peripheral lung are well indicated. Unless the tumor is directly beneath the pleura, it cannot be palpated; therefore, preoperative marking is needed. The procedure is contraindicated for patients with tumors located deep in the lungs because it is difficult to confirm the margin owing to difficulties in palpating. Furthermore, when the tumor is located near the left pulmonary ligament, manipulations are difficult because of the obstruction of the heart. Furthermore, when the tumor lies dorsally, although not impossible, manipulations are difficult. An advantage of this approach is that intercostal neuropathy can be avoided; therefore, this procedure should be indicated even in patients with unilateral lung metastasis.
Preoperative preparation
Under general anesthesia, differential lung ventilation of the operative side is performed using a double-lumen tube. The patient is placed in an open-legged supine position. In the lung resection, one-lung ventilation of the contralateral side is performed. If hypoxia or hypercapnia occurs as a result of CO2 insufflation and one-lung ventilation, it is treated by increasing the respiratory rate, and two-lung ventilation is performed in a timely manner.
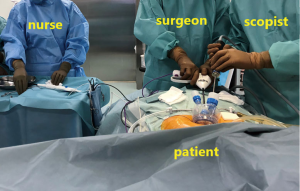
The surgeon stands between the patient’s legs; however, when it is difficult to perform manipulations, the surgeon will shift to the right or left side of the patient as needed. The scopist essentially stands to the right of the patient but may move occasionally depending on the position of the surgeon. The nurse stands to the left of the patient. A video monitor is placed cranial side of the patient (Figure 1).
Equipment preference card
A 5-mm rigid endoscope camera with a 30° oblique view is used. The port used for the single-port surgery was the GelPOINT Mini (Applied Medical, Rancho Santa Margarita, CA, USA) or Lapsingle (Sejong Medical Co. Paju, Korea). These ports enable 2–4 miniports to be inserted into the port platform, and if a 12-mm port is inserted, a stapler can be inserted. Furthermore, it enables CO2 insufflation. A vessel-sealing device is used for dissection from the rear surface of the sternum and reaches the bilateral thoracic cavities. To grasp the lungs, we used SILSTM Hand Instruments [single-incision laparoscopic surgery (SILS) clinch 36 cm Covidien, Mansfield, MA, USA] as forceps; however, they are no longer commercially available. For manipulations in this surgery, long lung-grasping forceps with bending or bent tip are needed. As the stapler, we selected Endo GIA (Covidien, Mansfield, MA, USA) capable of tip flexion for manipulations at hand. The distance of the pulmonary apex from below the xiphoid process is long; therefore, a standard-type stapler should be prepared rather than a short-type device.
Procedure
Port placement
Two 10-mm miniports and a 12-mm miniport for stapler insertion are inserted into the GelPOINT® Mini platform. If the Lapsingle, which is a port for single-port surgery, is used, the type with four miniports, including a 15-mm miniport, is selected. A 3-cm transverse skin incision is made 1 cm caudally below the xiphoid process. The linea alba connected to the xiphoid process is separated from the xiphoid process, and a finger is inserted behind the sternum to blindly detach the thymus from the posterior surface of the sternum. The linea alba separated previously is sectioned at approximately 1.5 cm caudally. A space is blindly created between the peritoneum and rectus abdominis to enable insertion of the single-type port. At this time, caution should be exercised to avoid opening the peritoneal cavity by tearing the peritoneum. If the peritoneal cavity is opened, surgery can be continued; however, when insufflating CO2, CO2 will enter the peritoneal cavity, which will inflate the abdominal cavity, thereby making the surgery slightly more difficult. The port for the single-port surgery is inserted through the subxiphoid incision.
Thymus dissection: bilateral pleurectomy
After performing CO2 insufflation at 8 mmHg, a vessel-sealing device is used to detach the thymus from the posterior surface of the sternum, and an incision is made into the mediastinal pleura to open bilateral thoracic cavities. When making an incision into the mediastinal pleura, a sharp incision to open the thoracic cavity may injure the lungs; therefore, the thoracic cavity is opened bluntly. In pulmonary wedge resection, there is no need to section the thymic tissue up to the neck, as done in thymectomy.
Pulmonary wedge resection
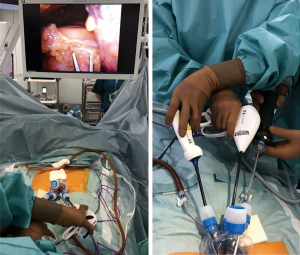
One-lung ventilation is performed for the contralateral lung. Using two cotton swabs, the surgeon identifies the location of the lesion. The range of motion of the two cotton swabs for thoracoscopy is expanded by crossing over within the port, making it easier to expose the lungs. Once the lesions have been identified, the lung is grasped using bent-tip gripping forceps, and the lung is lifted. After bending the tip of the stapler with the flexible tip so that the forceps and stapler do not interfere, the lung is resected. The resected lung is placed within the thoracic cavity. Via the same procedure, lesions of the contralateral side are also resected. The resected lungs are collectively placed in a pouch in the thoracic cavity and extracted via the subxiphoid incision (Figure 2).

Sealing test: drain placement
The sealing test cannot be performed for both lungs simultaneously. When water is poured into the bilateral thoracic cavities, the lungs dilate owing to the pooled water, which can cause damage and ventilation failure. In the event of bilateral lung resection, two 19-Fr Blake drains (ETHICON, New Jersey, USA) are inserted into the bilateral thoracic cavities via the 3-cm subxiphoid incision, with one drain on each side. Two layers comprising the rectus abdominis and subcutaneous tissue are sutured, and the wound is closed using intradermic sutures.
Tips, tricks, and pitfalls
- When setting up positions, lowering the foot side of the patient helps prevent interference of the surgeon’s arms and patient’s thigh and makes it easier for the vessel-sealing device to reach the posterior surface of the sternum.
- When the subxiphoid wound is too close to the xiphoid process, the forceps can barely reach the posterior surface of the sternum; therefore, the incision made is one finger-breadth caudal from the xiphoid process.
- For the incised wound of the skin, rather than a vertical incision, a transverse incision enables less interference between the forceps and camera.
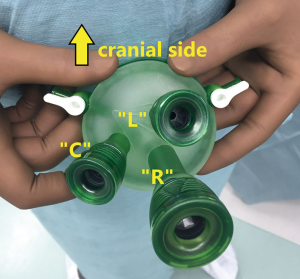
- The miniport of GelPOINT Mini should be placed as shown Figure 3 to minimize interference between the surgeon’s forceps and assistant’s camera. When using Lapsingle port, placement of the miniports is determined from the start.
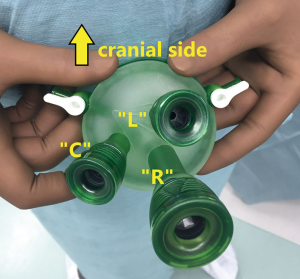 Figure 3 The camera is inserted into the GelPOINT Mini port “C”. The SILSTM Hand Instrument, SILS clinch, is inserted into the “L” port with the surgeon’s left hand. The LigaSure and Endo GIA are inserted into the “R” port with the surgeon’s right hand. Then, 10-mm ports are placed in “C” and “L,” and a 12-mm port is placed into “R”.
Figure 3 The camera is inserted into the GelPOINT Mini port “C”. The SILSTM Hand Instrument, SILS clinch, is inserted into the “L” port with the surgeon’s left hand. The LigaSure and Endo GIA are inserted into the “R” port with the surgeon’s right hand. Then, 10-mm ports are placed in “C” and “L,” and a 12-mm port is placed into “R”. - To ensure a good visual field and wide working space, differential lung ventilation and CO2 insufflation should be done simultaneously. CO2 insufflation enables atelectasis and displaces the lungs and mediastinum dorsally, which expands the space in the thoracic cavity and widens the working space for surgery.
- In one-lung ventilation in the supine position under CO2 insufflation, due care should be exercised because hypoxemia can readily occur. When hypoxemia occurs, the manipulation should be discontinued and CO2 insufflation should be terminated. Then, two-lung ventilation should be performed again until the patient’s respiratory status improves.
- The stapler is inserted from below the grasping forceps, and it makes the tip of the stapler can be inserted below the lifted lung.
- Compared with the intercostal single-port approach, in single-port bilateral pulmonary wedge resection via the subxiphoid approach, the distance from the port to the lesion is longer, which restricts manipulations.
- The surgeon performs manipulations, while keeping in mind the orientation of lung traction and of the stapler tip force to minimize interference between the instruments in both hands. When the lung has to be extended to the right of the patient and resected, the surgeon should perform surgery with the left and right hands crossed over (Figure 4).
- Via this approach, the camera tip can touch the fatty tissue in the anterior mediastinum and that above the pericardium, which consequently stains the camera tip. The trick for keeping the tip clean is to advance the scope deep into the thoracic cavity in one movement and to change the angle to a 30° oblique view.
- If the camera scope tip ends up entering between the surgeon’s forceps in the thoracic cavity, it can interfere with the forceps and camera. If interference is felt, via a 30° oblique view and change in the position of the camera, the scope tip will help the surgeon visualize the desired location. Outside of the port, when the camera head is between the hands of the surgeon and assistant, it will cause an interference between their hands. To prevent the camera head from interfering with the surgeon’s hands, using a long camera scope is a solution to prevent interference between instruments. The scopist always strives to prevent interference between instruments and to visualize the location that the surgeon wishes to see, so that the surgeon can proceed comfortably with the surgery both inside and outside the thoracic cavity.
- Compared with the lateral approach, the lungs cannot be palpated via the subxiphoid incision. Therefore, for lesions that cannot be seen from the lung surface, preoperative marking is needed. When the location of a lesion is unclear and when the tumor margin is unknown, placing an additional port in the lateral chest is recommended.
- For wedge resection of the left lower lobe, the forceps and camera need to reach the thoracic cavity beyond the heart; therefore, direct observation of the lesion, lifting the lung, and performing resections may be difficult. Furthermore, due care is required because heart compression caused by the forceps and camera scope can cause arrhythmia. When viewing the lungs is difficult because of fatty tissue obstruction above the pericardium, fatty tissue removal should be considered.
Comment
If metastasis affects both lungs, six incisional wounds are usually needed in both sides, comprising three incisions in each side of the chest. Bilateral intercostal neuropathy causes pain and numbness. Furthermore, for elderly patients and patients with surgical risks, two-stage surgery is performed; however, two-stage surgery is very stressful for the patient. Compared with the lateral intercostal approach, single-port bilateral pulmonary wedge resection via the subxiphoid approach enables a one-stage approach to the bilateral lungs via a single wound, and intercostal neuropathy, which always occurs owing to the lateral intercostal approach, does not occur. This approach without intercostal neuropathy might be well indicated for thoracoscopic lung biopsy in interstitial pneumonia and unilateral pulmonary wedge resection in selected patients. At our hospital, subxiphoid uniportal pulmonary wedge resection was performed for 25 lesions of 16 patients between November 2011 and February 2019. Among these patients, the approach was switched to a lateral thoracic approach in one patient due to entire adhesion and a port was added at the fourth intercostal space in the anterior axillary line in another patient, who had a palpable tumor. None of the patients experienced complications or died following operation. We deem this procedure to be safe. However, this approach has a limitation; because palpation is not possible, tumor marking is needed unless the tumor is directly beneath the pleura and resection of the lungs on the dorsal side or near the left pulmonary ligament is difficult. When forceful manipulations are performed for lung resection of the lower left lobe, the instruments compress the heart and cause arrhythmia (10). Surgery of the lower left lobe via the subxiphoid approach should be performed with caution. Via this approach, when the mediastinal pleura is opened bilaterally, the left and right thoracic cavities can interconnect even after surgery. When the both thoracic cavities are interconnected, if air leakage or recurrence of pneumothorax occurs, bilateral pneumothorax may result. Furthermore, when unilateral malignant pleural effusion occurs, the malignant pleural effusion may flow into the contralateral side.
In 2012, Lui et al. reported lobectomy via the subxiphoid approach (11). This lobectomy, which is considered the least invasive, and bilateral pulmonary wedge resection, which we presently report, has not yet gained popularity because of the difficulties in the manipulations involved.
Future development in instruments and surgical techniques, such as in new single-port robot systems, might help the subxiphoid approach, which offers advantages to the patient, and it may become a major surgical approach in the field of thoracic surgery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Michel Gonzalez) for the series “Advancement in the Surgical Treatment of Pulmonary Metastasis” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.05.02). The series “Advancement in the Surgical Treatment of Pulmonary Metastasis” was commissioned by the editorial office without any funding or sponsorship. TS serves as an unpaid editorial board member of Journal of Visualized Surgery from Feb 2018 to Jan 2020. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49:i6-16. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]
- Kido T, Hazama K, Inoue Y, et al. Resection of anterior mediastinal masses through an infrasternal approach. Ann Thorac Surg 1999;67:263-5. [Crossref] [PubMed]
- Mineo TC, Pompeo E, Ambrogi V, et al. Video-assisted approach for transxiphoid bilateral lung metastasectomy. Ann Thorac Surg 1999;67:1808-10. [Crossref] [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Negi T, Suda T. Subxiphoid single-port pulmonary bilateral metastasectomy. Asvide 2019;6:132. Available online: http://www.asvide.com/article/view/31761
- Hernandez-Arenas LA, Guido W, Jiang L. Learning curve and subxiphoid lung resections most common technical issues. J Vis Surg 2016;2:117. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [Crossref] [PubMed]
Cite this article as: Negi T, Suda T. Subxiphoid single-port pulmonary bilateral metastasectomy. J Vis Surg 2019;5:50.