Transanal repair of a recto-urethral fistula after robotic prostatectomy
Introduction
Acquired Recto-urethral fistula (RUF) is an uncommon post-operative complication of prostatectomy that can be challenging to treat. Although the incidence of RUFs is relatively low, estimated to be 0.9% to 9% after prostatectomy, it has a significant effect on a patient’s quality of life (1). Conservative management often involves fecal and urinary diversion to allow the fistula to close spontaneously or the inflammation to subside. Unfortunately, conservative measures often fail requiring some type of definitive surgical intervention (2). Multiple methods of repair have been described in the literature including abdominoperineal, transabdominal, transanal, transperineal, parasacral and transsphincteric approaches (3). The use of tissue interposition flaps or prosthetic meshes have also been described with varying degrees of success (4). Here we present the case of a transanal repair of a post prostatectomy RUF with rectal advancement flap.
Case presentation
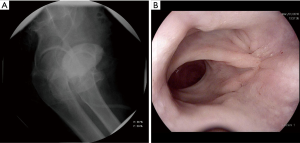
The patient is a 66-year-old male with a history of prostate cancer who underwent robotic prostatectomy. His post-operative course was complicated by the development of a RUF. The patient underwent both fecal and urinary diversion with a colostomy and supra-pubic catheter in an attempt to allow the fistula to heal. After failure of conservative measures, the patient presented to our center for definitive repair. A pre-operative flexible sigmoidoscopy revealed a small fistula in the anterior aspect, 3 cm above the dentate line, with healthy rectal mucosa surrounding the tract. Pre-operative MRI and lower GI study further delineated the defect and excluded any signs of surrounding inflammation (Figure 1). He was eventually scheduled for elective repair of the RUF 6 months after the diversions.

Patient selection and workup
Candidates for transanal repair have a few key factors in common. Location of the fistula is paramount to successful repair. A defect low enough in the rectum allows for easy accessibility and facilitates a smooth repair. Having healthy rectal tissue surrounding the defect is also important. This often means that patients with active infections or prior radiation therapy are not ideal candidates. Prior to pursuing repair of the fistula, the defect should be endoscopically visualized to facilitate surgical planning. Fecal and urinary diversion should also be considered in the cases of complex fistulas.
Pre-operative preparation
In our practice, patients undergo a full mechanical bowel preparation with oral antibiotics the day prior to surgery. Pre-operative intravenous antibiotics are administered prior to initial incision.
Equipment preference card
- Anorectal tray;
- Lonestar retractor;
- Headlight;
- Needlepoint electrocautery;
- 4-0, 3-0, 2-0 absorbable sutures;
- Suction device.
Surgical procedure
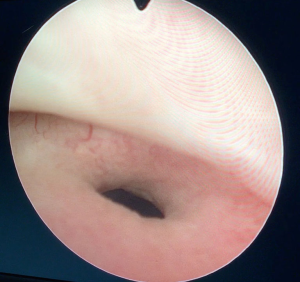
After induction of general anesthesia, cystoscopy was performed in the lithotomy position. The defect was clearly visualized and ureteral stents were placed by urology (Figure 2). The patient was then turned and placed in the prone jack-knife position. The buttocks were spread and taped in place. The anal area was prepped with povidone iodine solution and draped in the usual fashion. A Lone Star retractor was placed and examination revealed the fistula defect. The defect was confirmed to be at the cysto-urethral junction. Needlepoint electrocautery was used to create proximal and distal full thickness rectal flaps. The bladder wall was exposed and the fistula epithelium was removed in its entirety. The lumen of the bladder and urethra were identified. The lateral rectal tissue was released from the bladder wall to allow for a tension free repair. The cysto-urethral defect was closed primarily using transverse 4-0 PDS interrupted sutures. The bladder was then filled with water and a water-leak test was then performed to confirm adequate repair of the cysto-urethral defect. The rectal defect was then repaired primarily with alternating 2-0 and 3-0 Vicryl interrupted sutures. Particular attention was paid to ensure that full-thickness bites of healthy rectal tissue were incorporated in each suture (Figure 3).
Post-operative course
Once the repair was completed, the patient was discharged home. Two months after the procedure, the patient was brought for evaluation of his repair. Endoscopic evaluation showed a healthy rectal repair and cystogram was negative for signs of extravasation of contrast (Figure 4). His colostomy was subsequently reversed 3 months from the repair. At 30-month follow-up there was no evidence of fistula recurrence.
Tips, tricks, pitfalls
- A conservative approach is recommended. Inflammation should be allowed to subside. On average, a 3–6 months waiting period is advised.
- Both fecal and urinary diversion can aid in achieving a successful repair.
- A detailed pre-operative visualization of the defect is done using flexible sigmoidoscopy and cystoscopy.
- Higher patient BMI is favorable due to the excess tissue for approximation.
- The use of ureteral stents is advised for guidance. This is especially helpful if the lesion is close to the trigone and can help prevent injury to the cysto-ureteral junction. Stent placement can sometimes be challenging after prostatectomy due to shift of the cysto-urethral junction.
- If primary closure of the urethral defect is intended, then the edges of the urethral defect should be debrided until healthy tissue is reached.
- Lateral release of the full thickness rectal flaps provides increased mobility of the flap and aids in creating a tension-free repair.
- When developing the full thickness flap, the scar tissue between the bladder and the rectum can act as a guideline. While elevating the flap more proximally, Denonvilliers’ fascia should be identified and dissection is carried along this recognizable plane.
- A water leak test is beneficial in assessing adequacy of the repair.
- When dealing with larger defects or a prior history of radiation, consideration should be made for the use of an interposition graft with omentum or a gracilis muscle flap.
Conclusions
Management of RUF can be challenging for any surgeon and a multitude of approaches are available. The transanal approach has been shown to be both a safe and an effective method of repair for selected patients (4,6-9). Here we demonstrated a surgical technique for transanal repair of an acquired RUF with an endorectal advancement flap in an ideal candidate.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.10.03). JJP serves as an unpaid editorial board member of Journal of Visualized Surgery from Sep 2017 to Aug 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kitamura H, Tsukamoto T. Rectourinary fistula after radical prostatectomy: review of the literature for incidence, etiology, and management. Prostate Cancer 2011;2011:629105 [Crossref] [PubMed]
- Nyam DC, Pemberton JH. Management of iatrogenic rectourethral fistula. Dis Colon Rectum 1999;42:994-7; discussion 997-9. [Crossref] [PubMed]
- Hechenbleikner EM, Buckley JC, Wick EC. Acquired rectourethral fistulas in adults: a systematic review of surgical repair techniques and outcomes. Dis Colon Rectum 2013;56:374-83. [Crossref] [PubMed]
- Dreznik Z, Alper D, Vishne TH, et al. Rectal flap advancement--a simple and effective approach for the treatment of rectourethral fistula. Colorectal Dis 2003;5:53-5. [Crossref] [PubMed]
- Kim TD, Thomas S, Kochar K, et al. Transanal repair of a recto-urethral fistula. Asvide 2018;5:825. Available online: http://www.asvide.com/article/view/27962
- Ozuner G, Hull TL, Cartmill J, et al. Long-term analysis of the use of transanal rectal advancement flaps for complicated anorectal/vaginal fistulas. Dis Colon Rectum 1996;39:10-4. [Crossref] [PubMed]
- Jones IT, Fazio VW, Jagelman DG. The use of transanal rectal advancement flaps in the management of fistulas involving the anorectum. Dis Colon Rectum 1987;30:919-23. [Crossref] [PubMed]
- Razi A, Yahyazadeh SR, Gilani MA, et al. Transanal repair of rectourethral and rectovaginal fistulas. Urol J 2008;5:111-4. [PubMed]
- Garofalo TE, Delaney CP, Jones SM, et al. Rectal advancement flap repair of rectourethral fistula: a 20-year experience. Dis Colon Rectum 2003;46:762-9. [Crossref] [PubMed]
Cite this article as: Kim TD, Thomas S, Kochar K, Park JJ, Marecik S. Transanal repair of a recto-urethral fistula after robotic prostatectomy. J Vis Surg 2018;4:226.