
Video-assisted thoracoscopic sleeve lobectomy for endobronchial neoplasm: a video case series
Introduction
Carcinoma involving the bronchial tree is a rare and challenging clinical entity. The standard of care for resection of these tumors has evolved from open pneumonectomy to sleeve lobectomy since the sleeve approach has been shown to improve both long-term survival and quality of life (1,2). Since then, minimally invasive techniques for sleeve lobectomy have been developed and many centers have reported excellent short- and long-term outcomes (3-6). Our centre has successfully adopted a multiportal video-assisted thoracoscopic surgery (VATS) approach to sleeve lobectomy. The aim of this report is to present our technique through three case videos.
Patient selection and workup
Three cases of VATS sleeve lobectomy were selected to illustrate our operative technique. Written informed consent was obtained from all patients for publication of this article and accompanying media. Publication of these cases has been approved by our institution’s research ethics board. All cases were performed at Surrey Memorial Hospital in Surrey, British Columbia, Canada.
Case #1
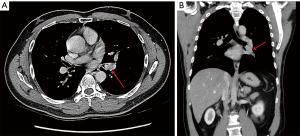
A 46-year-old male with a 30-year smoking history presented with hemoptysis. Past medical history was significant only for nasal polyps. Computed tomography (CT) revealed a 1.6 cm × 1.9 cm lesion which was confined to the left lower lobe (LLL) bronchus (Figure 1). Bronchoscopy revealed an endobronchial mass within the LLL bronchus which was found to be mucoepidermoid carcinoma on biopsy. Positron emission tomography (PET) did not show any distant disease. Figure 2 shows our surgical approach for this patient.

Case #2
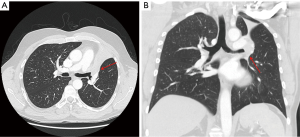
A 55-year-old male with a 35 pack-year smoking history had an incidental finding of a left hilar mass on a chest X-ray for muscle pain. He had no respiratory symptoms. Past medical history was significant only for hypothyroidism secondary to Hashimoto’s thyroiditis. CT scan revealed a large mass obstructing left upper lobe bronchus, which was confirmed on bronchoscopy (Figure 3). Biopsy showed squamous cell carcinoma of the lung. PET scan showed no distal disease and mediastinal staging via mediastinoscopy was also negative. Figure 4 shows our surgical approach for this patient.
Case #3
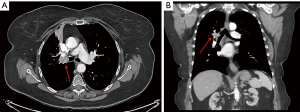
An 80-year-old previously healthy woman with a 40-pack-year smoking history was referred to our service with a 5-day history of cough and hemoptysis. Her CT scan showed a 2.2 cm × 1.0 cm mass located in the right upper lobe bronchus, along with a 1.1 cm ground-glass density in the right upper lobe (Figure 5). Bronchial biopsy confirmed a diagnosis of squamous cell carcinoma. PET scan showed no distal disease. Figure 6 shows our surgical approach to this patient.

Preoperative preparation
All patients underwent detailed pre-operative work-up including bronchoscopy, CT scan, pulmonary function testing, electrocardiogram, echocardiogram, PET scan, and outpatient anesthetic consult.
Equipment performance card
Standard VATS instruments were used in all cases. Special instruments unique to our approach include:
- Stryker 1488HD camera with a 30o scope (Stryker Corporation, Kalamazoo, MI, USA).
- Sonicision ultrasonic dissection device (Medtronic, Minneapolis, MN, USA).
- #15 scalpel blade.
- 3-0 or 4-0 p-dioxanone (PDS) and Vicryl (Ethicon, Somerville, NJ, USA) absorbable suture for bronchial anastomosis.
- Medtronic EndoGIA stapler with straight- and curved-tip reloads (Medtronic, Minneapolis, MN, USA).
Procedure
Our procedural technique is described in detail throughout the associated videos. The general approach for these cases is as follows.
Patients were brought to the operating room and given a general anesthetic with single lung ventilation. They were positioned in the manner of a standard VATS lobectomy according to the affected side. Four standard VATS ports were created for surgical access.
Initial steps involved division of the major vascular structures. In a manner similar to standard lobectomy, the pulmonary vein was divided first. The fissure was then opened to expose the pulmonary artery lobar branches, which were divided using a Medtronic EndoGIA stapler with vascular load. The fissure was then completed and focus was turned to the affected bronchus.
The bronchus was completely encircled with an umbilical tape and incised proximal to lesion. The specimen was then removed en bloc through a small extension to our utility port. Bronchoplasty was then accomplished using interrupted monofilament 3-0 or 4-0 PDS and Vicryl sutures. In some cases, these were tied exclusively on the outside of the anastomosis, in other cases some were tied both on the exterior and interior of the lumen, depending on surgical access and location of vascular structures. Pleural coverage was then placed over the anastomosis and secured to reduce the chance of a bronchopleural fistula. Immediate post-operative bronchoscopy was performed in all patients.
Post-operative management
All patients were extubated in the operating room and cared for in our thoracic surgery step-down unit at Surrey Memorial Hospital. There were no major in-hospital complications and patients were discharged home in stable condition.
All final pathology revealed good oncologic resection and patients remained well at follow-up. Outpatient bronchoscopy revealed well-healed anastomoses.
Tips, tricks & pitfalls
VATS bronchoplastic resection can be performed by surgeons who are well trained in standard VATS lobectomy. There are several key components that aid in minimizing risk and improving outcome. These will be listed in a systematic manner as follows:
- Staging: all patients must be adequately staged with a CT, PET, as well as EBUS and/or cervical mediastinoscopy.
- Patients must undergo detailed cardio-respiratory work-up prior to surgery and optimization must be undertaken by a multidisciplinary team including surgeons, respirologists, and anesthetists.
- During the diagnostic bronchoscopy, the ipsilateral endobronchial tree must be assessed to ensure a complete resection can be obtained. The contralateral lung must be examined to rule out synchronous pathology.
- An initial VATS staging must rule out pleural metastasis and also allow for assessing resectability.
- Vascular and fissural dissection and division must be completed prior to dealing with the bronchus. The mediastinal pleura as well as the inferior pulmonary ligament must be completely dissected and free of adhesions.
- The main bronchus must be mobilized and encircled with an umbilical tape. This mobilization must be performed carefully in order to avoid ischemia of the airway. Non-energy dissection is preferred at this phase.
- The bronchus distal to the lesion must be carefully mobilized, respecting the same principles as the main bronchial dissection. A scalpel must be used to divide the airway.
- An intra-operative frozen section must be performed to ensure the margins are microscopically free of cancer. This should be done prior to performing the anastomosis.
- The anastomosis is started in the back-wall and the most difficult part must be done first.
- Where the anastomosis will be closest to the vessels, the knots must be placed on the inside to reduce the chance of fistula formation and Vicryl suture must be used.
- Multiple interrupted sutures must be placed prior to tying the knots.
- The sutures must be approximately 3 mm deep and 3 mm apart.
- Once the sutures are no longer in proximity to vascular structures the knots can be tied on the outside and a PDS suture can be used.
- Once all the sutures are applied and the knots are tied, the anastomosis must be submerged in saline and a leak test must be performed. Additional sutures can be applied if a leak is identified.
- We prefer covering all of our anastomoses, usually with pleura. Other structures that can be used to cover the anastomosis including pericardial fat pad, intercostal muscles, and other muscles of the chest wall but a well vascularized anastomosis performed according to the above principles can be safely covered with pleura only.
- An intra-operative bronchoscopy must be performed to ensure: (i) the anastomosis remains well vascularized; (ii) the anastomosis is not stenotic; (iii) the distal airway is patent and all secretions and blood are cleared; (iv) there is no visible defect in the anastomosis.
- Airway anastomoses heal slower than gastrointestinal anastomoses and we prefer to watch the patients for slightly longer periods of time in hospital. We have a very low threshold to perform repeat bronchoscopy prior to discharging the patient.
Discussion
Sleeve lobectomy provides a suitable method to accomplish resection of tumors with bronchial involvement. The technique has been shown to be not only equivalent to- but sometimes superior to pneumonectomy for management of these lesions (1). Given the success of VATS lobectomy in improving many relevant clinical outcomes over open surgery, interest in the development of a video-assisted technique for sleeve lobectomy has grown. Although many centres continue to publish favourable outcomes related to video-assisted sleeve lobectomy, the procedure has been slow to gain widespread acceptance.
In the past decade, our centre has developed an experience with video-assisted sleeve lobectomy and bronchoplasty. We have found success with this procedure in terms of both oncologic and clinical outcomes. The cases presented in these videos show our technique for this procedure when applied to tumors involving three different bronchial areas. Our technique is similar to that of others who have published reports, although we tend to favour interrupted anastomosis for ease of approximation during bronchoplasty (10,11). We also prefer to use Vicryl suture tied on the inside of the anastomosis when there is close proximity to vascular structures.
We appreciate the opportunity to share our techniques with the wider community and hope our report will encourage further adoption of this procedure.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.09.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferguson MK, Lehman AG. Sleeve lobectomy or pneumonectomy: optimal management strategy using decision analysis techniques. Ann Thorac Surg 2003;76:1782-8. [Crossref] [PubMed]
- Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. [Crossref] [PubMed]
- Zhou S, Pei G, Han Y, et al. Sleeve lobectomy by video-assisted thoracic surgery versus thoracotomy for non-small cell lung cancer. J Cardiothorac Surg 2015;10:116. [Crossref] [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [Crossref] [PubMed]
- Li S, Chai H, Huang J, et al. Hybrid video-assisted thoracic surgery with segmental-main bronchial sleeve resection for non-small cell lung cancer. Surg Innov 2014;21:180-6. [Crossref] [PubMed]
- Wang X, Jiao W, Zhao Y, et al. Two-incision approach for video-assisted thoracoscopic sleeve lobectomy treating the central lung cancer. Indian J Cancer 2015;51:e18-20. [PubMed]
- Percy ED, McNeely C, Coffin T, et al. Video description of our technique for VATS sleeve lobectomy resection of LLL endobronchial lesion. Asvide 2018;5:749. Available online: http://www.asvide.com/article/view/27212
- Percy ED, McNeely C, Coffin T, et al. Video description of our technique for VATS sleeve lobectomy of LUL lesion with bronchial involvement. Asvide 2018;5:750. http://www.asvide.com/article/view/27213
- Percy ED, McNeely C, Coffin T, et al. Video describing our technique for VATS sleeve lobectomy for RUL lesion with bronchial involvement. Asvide 2018;5:751. Available online: http://www.asvide.com/article/view/27214
- Han Y, Zhou S, Yu D, et al. Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy with partial pulmonary artery resection. J Thorac Dis 2013;5:S301-3. [PubMed]
- Ostrowski M, Marjański T, Rzyman W. Video-assisted thoracoscopic bronchial sleeve lobectomy - a case report. Adv Respir Med 2017;85:250-2. [Crossref] [PubMed]
Cite this article as: Percy ED, McNeely C, Coffin T, Kearns MJ, Hafizi A, Al-Khaboori S, Razzak R, Ong S, Ashrafi AS. Video-assisted thoracoscopic sleeve lobectomy for endobronchial neoplasm: a video case series. J Vis Surg 2018;4:198.


