
Notes on the first uniportal video-assisted thoracic surgery lobectomy on June 25, 2009
My journey to uniportal video-assisted thoracic surgery (VATS)
20 years ago open thoracotomy was considered the standard approach for thoracic surgery. My journey in thoracic surgery started in 1999 at the University of Manitoba in Canada, where I learned to perform the full range of thoracic surgery using the open thoracotomy technique. At that time we performed multiportal VATS for pleural conditions only.
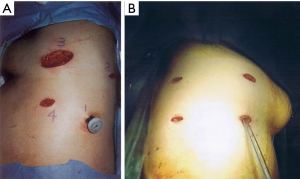
In 2005 I did a minimally invasive thoracic surgery fellowship at the University of Pittsburgh Medical Centre where I learned to perform multiportal VATS for the full range of thoracic surgery conditions, including VATS lobectomy. At the time, the standard was using 4 to 5 ports, including an accessory incision (Figure 1A,B). This technique was a major improvement from open thoracotomy, where trauma to the rib was avoided. Nevertheless, multiple skin incisions were still involved, multiple areas of the chest wall muscles were still traumatized by the ports, and multiple levels of intercostal nerves can still be affected.
In 2006 I started my practice as a Consultant in Thoracic Surgery at the National University of Singapore. I started with the 4 to 5 ports technique which I learned before. Having become a minimally invasive thoracic surgeon, the lingering question in my mind is whether VATS can become less invasive? Why do we need 4 to 5 ports? Is each of the ports indispensable?
This line of thinking and questioning led me to reduce the number of ports from 5 to 4 to 3, and by 2007 I started performing VATS lobectomy using a 2-port technique (Figure 2). I presented this technique in an international VATS conference held in Xiamen, China in 2007, in which Professor Robert McKenna and Professor Anthony Yim were fellow invited faculties.
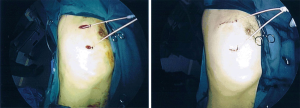
Patients were benefiting from this evolution, as it was clearly evident that each port reduction resulted in incremental reduction in their postoperative discomfort and pain medication usage, which translated into smoother recovery and reduced length of hospitalization. During that time, surgical advances were happening and single incision laparoscopic surgery (SILS) was introduced. The quest for less invasiveness in thoracic surgery continued, and by 2008 I was performing uniportal VATS (UVATS) using a 2–3 cm incision for a variety of thoracic surgery conditions such as bullectomies, pleurectomies, decortications, and mediastinal surgeries (Figure 3).

Major lung resections using UVATS posed a challenge, and I contemplated for 1 year on how this can be done. Having reduced form 5 down to 2 ports, it may appear that it was a small leap to go down to a single port, but in actuality it was a big step. The approach of multiportal VATS and UVATS was actually quite different. The most important differences were the direct angle and shorter distance of visualization through the thoracoscope, and the lesser acuity of the angle of surgical staplers towards the vital hilar structures. In a real sense, the visualization and approach to hilar dissection using UVATS has more similarities to open surgery than to multiportal VATS, except everything was performed through one small 2–3 cm cut without rib spreading while looking through a thoracoscope. This required a mindset shift (Figure 4).

The placement of the uniport incision is closer to the hilar structures, and the use of long surgical cutters represented potential safety hazard. In my reflection it became clear that UVATS lobectomy was feasible in all lobes. The one step that required special care was bronchial division for UVATS left upper lobe (LUL) lobectomy. At the time, angled tip staplers were yet to be available, and linear cutter posed a threat to the underlying pulmonary artery and aorta which is closely behind the LUL bronchus.
Surgical innovations are evolutions which progress through small incremental steps of improvements. Patient safety is paramount while each step is undertaken. “First do no harm” is a timeless adage that we will do well to bear foremost in mind during our pursuit for surgical advancement and betterment for our patients. In 2009, I had rehearsed all the steps necessary and was ready to perform UVATS lobectomy safely.
First UVATS lobectomy
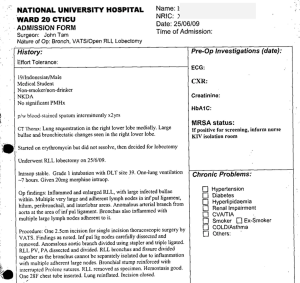
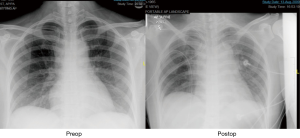
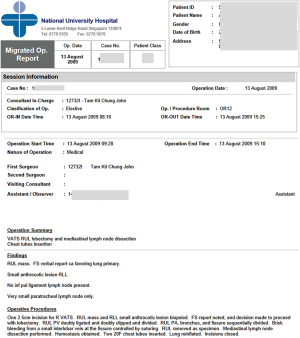
My first uniportal VATS lobectomy was performed on June 25, 2009 in the National University Hospital of Singapore. My patient was a 19-year-old medical student from Indonesia. He had right lower lobe sequestration and multiple infected bullaes (Figures 5,6). He suffered from frequent infections (fever, cough with minor hemoptysis) for many years despite maximal medical therapy, and required multiple hospitalizations each year resulting in significant interruptions in his studies. The patient was admitted to the hospital on June 24, 2009 (Figure 7).
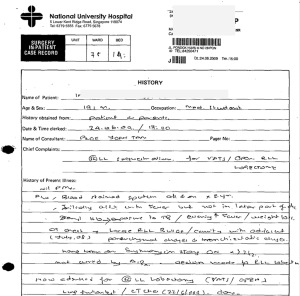
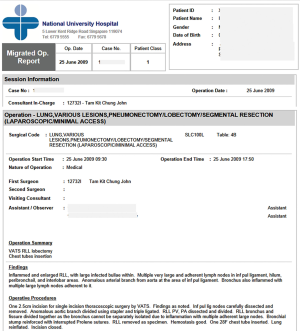
UVATS right lower lobectomy was performed on June 25, 2009 (Figures 8,9). One 2.5cm incision was made on the right 5th intercostal space at the anterior axillary line using the muscle sparing technique. No additional ports or access incisions were made. Dense adhesions were present due to multiple prior episodes of infection. The right lower lobe was found to be inflamed and enlarged, with multiple large infected bullaes within the lung parenchyma. Multiple very large and adherent lymph nodes were found in the inferior pulmonary ligament, hilum, peribronchial, and interlobar areas. The nodes were carefully dissected and removed. Anomalous arterial branch from the descending aorta was found near the inferior pulmonary ligament and it was ligated and divided. Standard anatomical dissection was performed. The right lower lobe pulmonary vein, pulmonary artery, bronchus and fissure were divided using surgical stapler through the same uniport. One chest drain was placed through the same uniport.

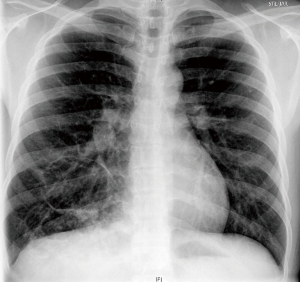
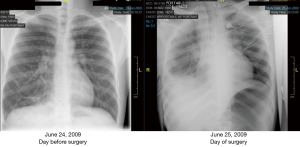
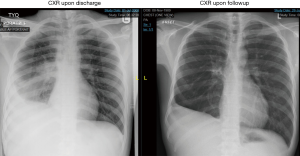
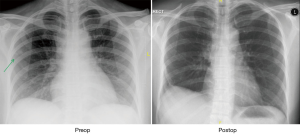
The patient’s postoperative CXR was satisfactory (Figure 10), and he was observed overnight in the cardiothoracic high dependency unit (Figure 11). Patient had an uneventful recovery. His chest drain was removed on postoperative day (POD) 5, and he was discharged from the hospital on POD 6 (Figure 12).

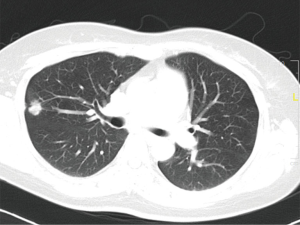
His follow up chest radiograph in the clinic showed expected volume loss of the right lung post-lobectomy (Figure 13). Histology report showed right lower lobe bullae with organization, congestion, mixed inflammation, and bronchiectasis. All dissected lymph nodes showed reactive hyperplasia (Figure 14). This patient has no further lung infections after surgery, and remains well until this day.
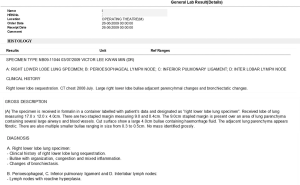
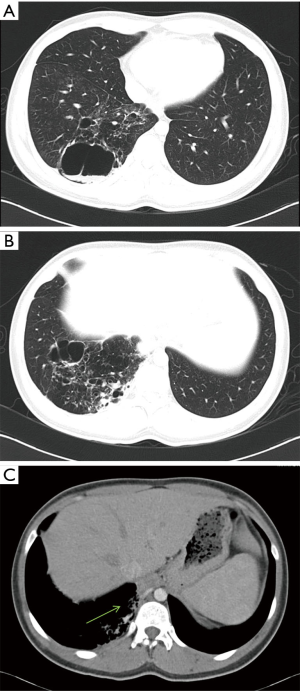
First UVATS lobectomy for lung cancer
My first UVATS lobectomy for lung cancer was performed in the National University Hospital in Singapore on August 13, 2009. The patient was a 44 year old lady with a 2-cm nodule in the right upper lobe (Figures 15,16). Surgery was performed through a 2.5-cm uniport at the 4th intercostal space in the anterior axillary line on the right chest. Standard anatomical dissection was performed for the bronchovascular structures and mediastinal nodal dissection was performed (Figure 17). Postoperative chest radiograph was normal (Figure 18). Histology report showed a 1.5-cm moderately differentiated adenocarcinoma resected from the right upper lobe. All resected lymph nodes were negative for malignancy (Figure 19).
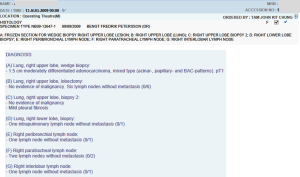
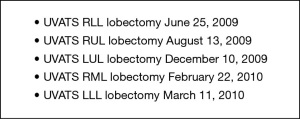
Subsequently, UVATS lobectomies were performed on the other lobes in the following months (Figure 20). A case series of our early experiences with UVATS lobectomy was submitted to an international thoracic surgery journal on February 9, 2012. This was however rejected by the journal editor on the basis that our case series was not randomized and a comparison group was absent. With this delay, the article was eventually submitted to The Annals of Thoracic Surgery and was accepted as on July 1, 2013 for publication in the December 2013 edition of the Annals (1) (Figure 21).
Epilogue
Since the first UVATS lobectomy was performed in 2009, a routine UVATS program was offered in the National University Hospital in Singapore. A new generation of thoracic surgeons in Singapore and in Asia was trained in this technique. Thousands of patients in Singapore have since benefited from the UVATS approach.
In the words of Professor Gaetano Rocco, “it doesn’t actually matter today who devised uniportal VATS—what really matters today is for the technique to stand the test of time”. This is true indeed and the wish is for all UVATS surgeons to work together in friendship and cooperation to propagate this excellent technique to all corners of the earth.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jose Luis Danguilan) for the series “Dedicated to the 6th Asian Single-port VATS Symposium 2018” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.07.24). The series “Dedicated to the 6th Asian Single-port VATS Symposium 2018” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [Crossref] [PubMed]
Cite this article as: Tam JKC. Notes on the first uniportal video-assisted thoracic surgery lobectomy on June 25, 2009. J Vis Surg 2018;4:173.


