
Awake thoracoscopic pericardial window is safe and feasible
Highlight box
Key findings
• Pericardial effusive disease can be effectively treated with awake thoracoscopic pericardial window.
What is known and what is new?
• There is scant literature on awake thoracoscopic pericardial window.
• Thoracoscopic pericardial window can be safely performed without general anesthesia.
What is the implication, and what should change now?
• Patients who are not candidates for general anesthesia can be offered this procedure.
Introduction
Awake minimally invasive thoracic surgery has been increasingly performed as surgeons attempt to minimize the complications associated with general anesthesia on an ever-increasing population of patients with co-morbidities. Traditional thoracoscopic surgery under general anesthesia with an immobile patient and immobile lung can be safely performed with good outcomes but there remains a subset of patients for which general anesthesia is of higher or even prohibitive risk. Awake video-assisted thoracic surgery (VATS) procedures described in the literature have been primarily focused on pulmonary resections and pleural procedures but there remains a paucity of literature (1,2) in regards to pericardial procedures and their safety and efficacy. We present a retrospective, non-consecutive case series of awake VATS pericardial window procedures in a tertiary care hospital by a senior thoracic surgeon with extensive experience in minimally invasive surgery (Table 1). We present this case series in accordance with the PROCESS reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-37/rc).
Table 1
| Case | Demographics | Prior drainage | Side | Operative time (min) | Sedation administered | Local anesthesia | Pressor support | Associated procedures | Pathology |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 80-year-old, F | Yes | Right | 52 | Dexmedetomidine: 27.2 mcg | Lidocaine, marcaine | None | Pleural biopsy, talc pleurodesis | Chronic fibrous pericarditis |
| Fentanyl: 112.5 mcg | |||||||||
| Midazolam: 1 mg | |||||||||
| Propofol: 42.24 mg | |||||||||
| 2 | 69-year-old, M | Yes | Right | 95 | Midazolam: 4 mg | Lidocaine, marcaine | Phenylephrine 100 mcg | Pneumolysis, pleural biopsy | Fibrous pericarditis |
| Ketamine: 20 mg | |||||||||
| Fentanyl: 250 mcg | |||||||||
| 3 | 64-year-old, M | Yes | Left | 60 | Dexmedetomidine: 98.9 mcg | Lidocaine, marcaine | None | None | Acute fibrous and organizing pericarditis |
| Midazolam: 2 mg | |||||||||
| Fentanyl: 250 mcg | |||||||||
| 4 | 31-year-old, F | No | Left | 57 | Dexmedetomidine: 1 mcg/kg/h | Lidocaine, marcaine | Phenylephrine 0.5 mcg/kg/min | Incisional biopsy of mediastinal mass | Acute T-cell lymphoblastic lymphoma |
| Midazolam: 2 mg | |||||||||
| Fentanyl: 150 mcg |
F, female; M, male.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series. A copy of the written consent is available for review by the editorial office of this journal.
Case 1
The patient was an 80-year-old female visiting from Asia with a history of stroke and atrial fibrillation who presented with increasing shortness of breath to a primary care physician. She was found to have a large pericardial effusion on echocardiogram and sent into the hospital. She underwent pericardiocentesis with drainage of 1.3 L of bloody fluid prior to consultation. This raised the concern for malignant etiology. Computed tomography (CT) scan revealed bilateral pleural effusions and bilateral subsegmental pulmonary emboli so she was started on a heparin drip. She underwent pigtail drainage of her right pleural space but both pleural and pericardial fluid cytologies were negative for malignancy so tissue biopsy was recommended to definitively rule out malignancy.
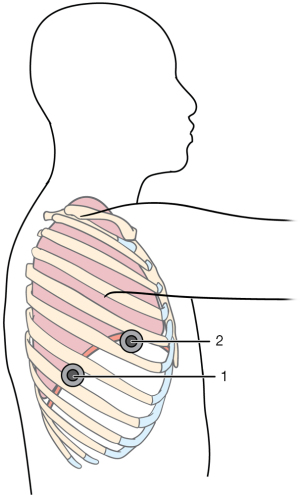
The patient was brought to the operating room. Once she was adequately sedated, she was placed in the left lateral decubitus position. All pressure points were appropriately padded. The patient was prepped and draped and local anesthesia was administered. A 10-mm incision was made in the 7th intercostal space in the posterior axillary line and the pleural cavity was entered under direct visualization using electrocautery. A 10-mm 30-degree thoracoscope was inserted and the pleural contents were visualized. The right pleural effusion was drained and pleural biopsy was performed. A 10-mm access incision was made in the 5th intercostal space in the anterior axillary line as a working port. We performed the pericardial window procedure and the piece of pericardium was sent to pathology. Talc pleurodesis was performed of the right pleural space and chest tube was placed through the camera port and secured with a prolene stitch. The access incision was closed with vicryl sutures for the deep layers and Monocryl for the skin (Figure 1).
Operative time was 52 minutes and anesthesia time was 2 hours 14 minutes. Post-operatively, the patient did well with resolution of her symptoms. The chest tube was removed on post-operative day 3 and she was discharged home on post-operative day 7. Pathology and culture results came back negative for malignancy and tuberculosis, showing chronic fibrous pericarditis with hemosiderin deposition.
Case 2
The patient was a 69-year-old male former smoker with prior asbestos exposure with a history of hypertension, hyperlipidemia, end-stage renal disease on hemodialysis, and stroke with dementia requiring 1:1, who presented with shortness of breath and cough, and found to have a partially loculated right effusion with pleural thickening and pericardial effusion. He had previously undergone right thoracentesis prior to this admission and cytology was non-diagnostic. He was now admitted after pericardiocentesis with pericardial drain placement. The drain had persistent bloody output and cytology was negative. Given these findings, tissue biopsy was recommended to rule out malignancy.
The patient was brought to the operating room. Once adequate sedation had been provided, the patient was turned to the left lateral decubitus position. Local anesthesia was administered and two incision thoracoscopy was performed. There were extensive adhesions and dense pleural peel. The adhesions were broken up and the pleural biopsy and pericardial window procedures were performed. Pericardial and pleural drains were then placed.
Operative time was 1 hour 35 minutes and anesthesia time was 3 hours 9 minutes. Post-operatively, the patient did well. The pericardial drain was removed post-operative day 4, the chest tube was removed on post-operative day 7, and the patient was discharged to subacute rehab on post-operative day 10. Pathology revealed fibrous pericarditis and no evidence of malignancy.
Case 3
The patient was a 64-year-old male former smoker with a history of HIV, hypertension, diabetes, angiodysplasia of colon, and chronic renal insufficiency who presented with nausea, vomiting, and general malaise. He also complained of shortness of breath and intermittent cough. He was found to have a right lower lobe consolidation for which antibiotics were started, and a pericardial effusion that was drained with dramatic improvement of symptoms prior to consultation. However, repeat imaging revealed re-accumulation. Therefore, a pericardial window was recommended. A CT scan revealed bilateral pleural effusions, left greater than right, so a decision was made to approach through the left chest.
The patient was brought to the operating room. Once adequate sedation was provided, the patient was turned to the right lateral decubitus position. Given poor partial pressure of oxygen (PaO2) of 54 on blood gas, a decision was made not to intubate the patient. Local anesthesia was given and two-incision thoracoscopy was performed. The pleural effusion was drained and the pericardial window procedure was performed. Pericardial and pleural drains were then placed.
Operative time was 1 hour and anesthesia time was 1 hour 59 minutes. Post-operatively, the patient did well. The pericardial drain was removed on post-operative day 2, the chest tube was removed post-operative day 4, and the patient was discharged home on post-operative day 5. Pathology revealed acute fibrinous and organizing pericarditis.
Case 4
The patient was a 31-year-old female never smoker with no significant past medical history who presented with worsening dyspnea on exertion, night sweats, chest discomfort, and dry cough. She was noted to be tachycardic on presentation. She had profound leukocytosis with a white blood cell count of 137.6×109/L. On work-up, she was found to have a large anterior mediastinal mass as well as a left pleural effusion and pericardial effusion. The echocardiogram was concerning for impending tamponade physiology with a moderate to large effusion with partial right ventricular diastolic collapse. Pericardiocentesis could not be performed as the presence of the anterior mediastinal mass prohibited a window for drainage. The anterior mediastinal mass was highly suspicious for lymphoma. Given the echo findings prohibiting general anesthesia and the need for tissue diagnosis, awake surgery was recommended.
The patient was brought to the operating room. Once the patient was adequately sedated, she was turned to the right lateral decubitus position. Local anesthesia was provided and two-incision thoracoscopy was performed. The left effusion was drained and the pericardial window procedure and biopsy of the mediastinal mass were performed. A pleural drain was placed.
Operative time was 57 minutes and anesthesia time was 2 hours 4 minutes. Pathology of the mass and cytology of both the pericardial and pleural effusions were consistent with acute T-cell lymphoblastic lymphoma. Post-operatively, she did well. The pleural drain was removed on post-operative day 2 and she was discharged later that day to start treatment for her newly diagnosed lymphoma.
Discussion
Key findings
Traditionally, the surgical treatment for pericardial effusion has been an open procedure via either a subxiphoid or trans-thoracic approach with or without general anesthesia. With the advent of single lung ventilation, regional anesthesia was largely abandoned as thoracic surgeons were able to operate on a completely immobilized collapsed lung, thus enabling minimally invasive approaches. However, as surgeons determine that an immobile collapsed lung is less of a necessity for safe thoracic procedures, awake minimally invasive surgery utilizing regional anesthesia has become even more important as the morbidity involved with general anesthesia (3) and mechanical ventilation (4) can be avoided.
Thoracoscopic approaches to pericardial effusion allow better visualization of the pericardium, allowing potentially better directed drainage and biopsy, as well as better concomitant evaluation of the pleural space. VATS pericardial window has been available to surgeons since the turn of the century, however abrupt drop in blood pressure upon induction remains a concern (5).
Strengths and limitations
Potential risks and complications of the awake VATS pericardial window include conversion to general anesthesia, conversion to open thoracotomy, myocardial injury, post-operative bleeding, and prolonged air leak, none of which our patients experienced. The ability to make definitive conclusions is limited by the small number of cases and selection bias as all patients who could undergo general anesthesia underwent traditional VATS, and awake VATS was reserved only for patients deemed high risk for general anesthesia. Despite this, our case series shows that awake VATS pericardial window can be safely performed with good results.
Comparison with similar searches
Although there are no large randomized studies looking at the efficacy of awake VATS procedures compared to traditional procedures with general anesthesia, there is some data to suggest that there are several benefits of awake surgery. These potential advantages include quicker recovery times, lower procedural costs, reduced morbidity, shorter hospital stays, and better respiratory function in the early post-operative period (6). In addition, awake VATS can potentially be offered to patients who are generally contraindicated for general anesthesia. More importantly, for patients in which malignancy may be the diagnosis, the decreased effect of awake surgery on both the stress response and the immune response may offer some oncologic benefit (7,8).
Explanation of findings
Aside from a few case reports and brief anecdotes in papers discussing the diversity of awake VATS, there has been very little literature addressing the feasibility of awake VATS in the drainage of pericardial effusions. Our small case series reinforces that this procedure can be performed safely and effectively for patients, without the need for conversion to either general anesthesia or open thoracotomy. Given the potential benefits of awake VATS, pericardial drainage with this technique should be considered as an option for patients.
Implications and actions needed
In particular, it becomes a more significant option in patients with larger pericardial effusions as avoidance of the induction of anesthesia can obviate the possible acute drop in blood pressure in patients with hemodynamic concerns, especially those in whom pericardiocentesis is not a feasible option.
Conclusions
As the technique continues to evolve and as more thoracic surgeons become more facile and comfortable with awake VATS (6), the utilization of this technique continues to expand. From relatively minor procedures, awake VATS has expanded to anatomic lung resections and mediastinal procedures (9,10). Therefore, it behooves the thoracic surgeon to consider this as an option on a patient population that is becoming increasingly older and sicker with more comorbidities.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PROCESS reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-37/rc
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-37/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-37/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ohuchi M, Inoue S, Ozaki Y, et al. Single-trocar thoracoscopic pericardio-pleural fenestration under local anesthesia for malignant pleural effusion: a case report. Surg Case Rep 2019;5:136. [Crossref] [PubMed]
- Park CY, McGonigle NC. Single-Port Thoracoscopic Pericardial Window Under Local Anesthesia. Innovations (Phila) 2018;13:62-4. [Crossref] [PubMed]
- Parker BM. Anesthetics and anesthesia techniques: impacts on perioperative management and postoperative outcomes. Cleve Clin J Med 2006;73:S13-7. [Crossref] [PubMed]
- Della Rocca G, Coccia C. Acute lung injury in thoracic surgery. Curr Opin Anaesthesiol 2013;26:40-6. [Crossref] [PubMed]
- Flores RM, Jaklitsch MT, DeCamp MM Jr, et al. Video-assisted thoracic surgery pericardial resection for effusive disease. Chest Surg Clin N Am 1998;8:835-51. [PubMed]
- Pompeo E, Sorge R, Akopov A, et al. Non-intubated thoracic surgery-A survey from the European Society of Thoracic Surgeons. Ann Transl Med 2015;3:37. [PubMed]
- Tacconi F, Pompeo E, Sellitri F, et al. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact Cardiovasc Thorac Surg 2010;10:666-71. [Crossref] [PubMed]
- Vanni G, Tacconi F, Sellitri F, et al. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg 2010;90:973-8. [Crossref] [PubMed]
- Pompeo E. Awake thoracic surgery--is it worth the trouble? Semin Thorac Cardiovasc Surg 2012;24:106-14. [Crossref] [PubMed]
- Mineo TC, Tacconi F. From "awake" to "monitored anesthesia care" thoracic surgery: A 15 year evolution. Thorac Cancer 2014;5:1-13. [Crossref] [PubMed]
Cite this article as: Lee DS, Flores RM. Awake thoracoscopic pericardial window is safe and feasible. J Vis Surg 2024;10:4.


