Non-surgical treatment of pectus carinatum with the FMF® Dynamic Compressor System
Introduction
Pectus carinatum is a deformity of the anterior chest wall. Two subtypes have been described: the chondrogladiolar variant, which comprises up to 95% of the cases, and presents with protrusion of the sternal body, and the chondromanubrial variant, showing protrusion of the superior component of the sternum (manubrium).
Pectus carinatum goes far beyond a simple aesthetical problem. It can be responsible of physical signs and symptoms and also has significant psychological impact. Defects tend to worsen during pubertal growth spurts and even during adult life.
Recent evidence shows that these patients are at risk for a disturbed body image and reduced quality of life (1) and many patients refer feelings of discomfort, shame, shyness, anxiety, anguish, and even depression, which can lead to social isolation.
Chest pain or discomfort, especially when lying in prone position, intolerance to physical exercise, scoliosis, impaired shoulders and kyphotic position are some of the physical signs and symptoms.
Since cardio-respiratory disorders are very rare, and if present, mild in intensity, surgical reconstruction was traditionally indicated only to correct the most severe cases of pectus carinatum, leaving the vast majority of the patients undertreated.
Although surgery improves the chest’s shape and patients are satisfied with the results, surgery always leaves a visible scar behind and unfortunately cannot correct the flaring of ribs or completely remodel the thorax.
Several non-surgical approaches have been proposed for pectus carinatum patients (2-8) and during the mid 2000s, when non-operative approaches began to consolidate, major surgery was the only option.
In this article we will address the FMF® Dynamic Compressor System (DCS), which was co-created in Argentina by the author (MFM) and his partner, Dr. Carlos Fraire (9-11) in 2001 and is extensively used worldwide today.
Between years 2008 and 2013, teams led by Dr. Manuel Lopez from the Unit of Chest Wall Deformities at the University Hospital of Saint Etienne in France (12) and Dr. Robert E. Kelly from the Eastern Virginia Medical School, Children’s Hospital of The Kings Daughters in Norfolk, USA (13) have been able to validate the argentine experience with the FMF® DCS in their own patient populations. They have also concluded that this brace is an effective and minimally invasive tool for treatment of pectus carinatum.
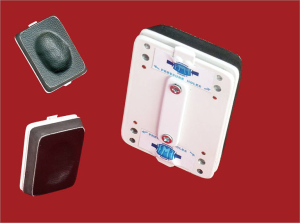
The FMF® DCS is a system (Figure 1), which comprises the following elements:

- A custom-fitted, expandable, low-profile, cushioned, ultra-light aluminum brace that is adjustable to any thoracic shape or size and has a locking system on one side to keep it in place;
- An adaptable compression plate to be placed against the chest wall protrusion.
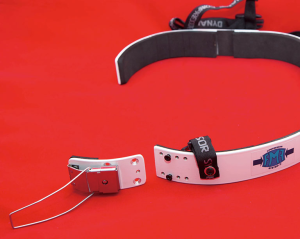
A tool kit is available for the physician. The briefcase contains the following items (Figure 2):
- A pressure measuring device (PMD) which can be docked to the brace’s compression plate and measures the pressure exerted to the patient in pounds per square inches (PSI) (Figure 3);
- A chest measuring ruler;
- A metric tape;
- A portable plate bender to curve the aluminum segments according to the patient’s initial chest size and shape and throughout the continuous re-shaping process;
- Magnetic screwdrivers and screws.
The FMF® DCS corrects pectus carinatum gradually by using the continuous anterior-posterior compression to widen and remodel the entire chest and cartilages, which accommodate, grow and finally ossify in the correct position.
Two measurements were defined by the authors and must be collected:
- Pressure of correction (PC): an indirect parameter of the chest wall’s flexibility. It is defined as the pressure applied to the patient, in the most protruding area of the chest, needed to accomplish a proper shape of the thorax.
- Pressure of treatment (PT): is the pressure required to treat the patient. It should be measured before and after adjusting the FMF® DCS.
Patient selection and workup
Stage 1: patient evaluation: medical history, measurements and request of the FMF® DCS
The first step in the patient selection process is to distinguish patients who are good candidates for the FMF® DCS from those who should be treated surgically.
Specific signs and symptoms possibly associated to pectus carinatum need to be addressed; also psychological and social impact must be evaluated. The patient’s column and thorax need to be inspected and palpated, to determine if the pectus carinatum is of the chondrogladiolar or chondomanubrial variant, to evaluate symmetry, rigidity of the chest wall, pain, etc.
The second step is to measure the baseline PC, as shown in Figure 4. To do this, the PMD will be used. The “AVERAGE” button of the device must be pressed so that it measures the average PC, taking into consideration its variation due to the patient’s respiratory movements.

If the pectus carinatum is of chondrogladiolar type and the PC is <14 PSI, a conservative, non-surgical approach should be implemented. Other measurements of the thorax are needed, so that the custom-fitted brace can be ordered, as shown in Figure 5.

- Thoracic perimeter.
- Transverse diameter of the chest.
- Anterior-posterior diameter of the chest.
- Pectus carinatum elevation.
Patient identification details, PC, thoracic measurements and position of the pectus carinatum (left, right, center) are to be registered in the Order Form. The size of the compression plate must also be indicated, and although most will do well with the standard size, five other sizes are available, as well as a hollow plate for patients with very sharp-edged pectus carinatum (Figure 6). The number of pads can also range from 1 to 3, depending on the size of the breasts, to maximize comfort in females.
Usually, pictures are taken with the patient’s consent, to keep a record of the baseline status and evaluate progress at subsequent visits. In our experience, being able to review the changes with the patient enhances motivation and compliance.
A set of six pictures is enough: left and right 3/4 profile and full profile, front view of the thorax and front view of the thorax from above. Figure 7 shows how to take this last picture.
Chest X-ray, CT scan or a chest MRI are not routinely indicated. If the patient presents with an atypical or stiff pectus carinatum, severe pain, or belongs to a family that feels insecure about the diagnosis and proposed management, further investigation may be recommended.
Although uncommon, if cardiopulmonary symptoms are present, pulmonary function tests and an echocardiogram are a must.
Stage 2: initial fitting of the brace and patient training
The FMF is received and assembled. The PC is measured again prior to fitting the brace.
Once the brace is fitted (Figure 8), the PT needs to be adjusted, never higher than 2.5 PSI. If higher, the brace will be loosened by using the different adjustment positions (see Figure 9) and the PT will be measured again until satisfactory values are obtained. Figure 10 shows how the PMD is docked onto the brace and the PT is measured and Figure 11 shows how the compression plate can be moved laterally to both sides, so that it is finally placed and fixed exactly above the pectus carinatum.



The patient is trained so that he/she can put on and take off the brace by him/herself.
The patient is then requested to wear it for 30 min and return to the physician’s office for evaluation of tolerance of the device. If the skin is too sensitive or the patient refers pain or discomfort to breathe, the PT will be reduced, until the device is well tolerated.
Initially, patients will be classified into one of four groups following the treatment guidelines shown in Table 1.
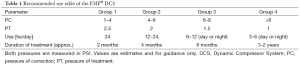
Full table
Group 1 and 2 patients are instructed to wear the FMF® DCS every day, overnight and as much as possible during the day, depending on their activities. They are only allowed to remove the device during sports and while having a shower/bath. We ensure that they understand that the more they wear the device, the faster they will correct the defect.
Patients belonging to group 3 and 4, will begin to wear the system less hours per day, at lower PTs, to indirectly increase the flexibility of the thoracic cage, enhance compliance and prevent skin lesions. We are careful to advise these patients about the complications of overusing the brace and the need to strictly follow medical indications.
The PC and the duration of treatment result very useful in helping patients understand what to expect throughout the treatment stages.
Stage 3: correction phase
The patient has to return for follow up monthly. During each visit, the PT is measured with the brace setting as is, the skin status is evaluated, together with the habits of use of the brace and the practice of complementary activities. The PC is also measured and the brace is adjusted to set a new PT and usage pattern as described in Table 1.
Once the patient’s PC lowers to the PC range of the previous group, he/she is re-classified and time of usage is adjusted accordingly.
The correction phase ends when the interdisciplinary team, patient, and/or family agree that the deformity has been fully repaired.
Stage 4: weaning phase
Once the defect is reverted (PC equal to zero), the FMF® DCS is gradually withdrawn to avoid eventual partial recurrences. Pectus carinatum may return mildly, in approximately 10% of cured patients, particularly if they have been treated before pubertal growth spurts or in case they have cured very rapidly.
During the weaning phase, patients wear the brace as a “retainer” during the day or overnight (they generally prefer the latter), every day for the first month, every 2 days for the second month and every 3–4 days for the next months (range, 2–6 months).
The faster the patient gets cured, the longer the weaning phase should be. PT will remain fixed during the post-correction period. The weaning period is not contemplated in the calculation of the duration of treatment.
Stage 5: follow-up phase
Provisory treatment interruption is indicated when the weaning period ends. Patients are controlled every 6 months until they are 18 years old. In adults, treatment finishes when the defect is corrected. Nonetheless, they are all instructed to return if any partial recurrence is observed so that it can be corrected with a few more months of treatment with the brace.
Role of team members
Physiotherapist
The role of physiotherapy is central to the non-surgical therapy of pectus carinatum. Daily physical therapy exercises can be indicated, to improve elongation, posture, etc. Swimming, playing wind instruments, inflating balloons and other similar respiratory exercises are indicated and encouraged as accessory activities to complement the non-operative treatment, especially to treat the costal flares.
Pediatrician or primary care physician
The role of the pediatrician and the primary care physician is crucial. They are key players for the early detection of this health problem, and timely consultation, referral and treatment.
It is estimated that the optimal timing for non-surgical therapy of pectus carinatum is between 10 and 15 years old, because of greater chest wall malleability, and enough time available to execute the bracing protocols and minimize recurrence.
In our experience, younger patients have a lower PC (major thoracic flexibility) than older patients and better final results are seen in pectus carinatum patients with lower PCs. Unfortunately, it is still frequent to receive referred patients older than this, because the severity of the pectus carinatum or the associated signs or psychological impact have been overlooked or underestimated.
Also, pediatricians and primary care physicians should be well aware that there are some conditions associated to pectus carinatum, being Marfan and Noonan syndrome most common. They should be alert and ready to order a genetic consultation if there are features suggesting a genetic syndrome, to ensure that their patients will receive adequate and timely multi-specialty care.
Tips and tricks
- It is recommended that for adequate measurement of the PC two persons are involved.
One person will be holding the PMD and pressing it onto the most protruding area of the thorax until the thorax seems leveled. The other person will observe the patient’s thorax from the side (profile) and will let the person holding the PMD know when the thorax seems leveled, so that the PC is measured.
- When fitting the brace on the patient, ensure that the space between the sides of the chest and the brace allows one finger to fit. It is very important that enough space is available to allow for lateral expansion of the thorax as remodeling occurs. When enough pressure to correct the pectus carinatum is applied on the chest wall, lateral expansion of the thorax naturally occurs, as can be seen in Figure 12.
- Although Table 1 is a general guideline, treatment can be customized for each patient considering individual tolerance, characteristic of the defect, skin status and age.
- Always check the PT during maximal inspiration. Values of 2.5 PSI or more must be avoided because skin lesions due to pressure necrosis can happen or the patient may not tolerate the device well enough, leading to non-compliance.
Patients with sensitive skin, age lower than 4 years old, stiff chests or reporting pain will have their brace set at PTs ranging from 1 to 2.4 PSI.
- A PT higher than that obtained at the last evaluation, can mean that the patient either has not worn the brace as indicated, or has grown up. This can be clarified by checking the patient’s records of height and weight and by verifying if the brace seems too tight. Be sure to keep these records updated.
- Pay attention to comfort to avoid non-compliance and complications:
- Different compression plates exist, adaptable to distinctive sternal protrusions, independently of their locations, sizes and shapes. Compression pads can also be adhered to the compression plate to cushion the defect, prevent skin lesions, increase PT in girls with breast development, etc.;
- Patients with extremely sensitive skin can experience relief by using a tight cotton shirt below the brace, or by placing a DuoDerm® Extra Thin patch at the site of the defect for protection.
- Since the end of the correction phase is defined as the impression of full resolution of the deformity by the patient, the family and the interdisciplinary team several methods can be used to evaluate this. It is important to discuss which criteria will be used. Some examples are pre and post treatment photographs, a scoring system ranging from 1 to 10, etc.
Conclusions
A summary of the advantages of the FMF® DCS over surgical therapy are listed below:
- It objectively measures the PC and uses it to guide treatment decisions, also allowing for prediction of therapy duration and prognosis.
- It permits in-situ outpatient clinic adjustments, avoiding the need of referrals.
- It not only remodels sternum and cartilaginous ribs permanently, but also results in complete thoracic re-shaping and leaves no visible scars.
- Complications are uncommon (4.6%), mild and easy to resolve: back pain, hematoma and skin ulceration.
- It eliminates the risks of anesthesia and major surgeries, decreasing the complication rate and the activity restrictions associated to implant placing.
- It also avoids hospital admission, surgery and implant costs, significantly reducing the cost of treatment.
- It can help patients who fail bracing to soften the chest wall in preparation for surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: Bruno Strappa is a full time employee at Pampamed S.R.L. Marcelo Martinez-Ferro is also owner of Pampamed S.R.L, an argentine company holding the license for commercialization of the FMF® Dynamic Compressor System. The other authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Steinmann C, Krille S, Mueller A, et al. Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: a control group comparison of psychological characteristics prior to surgical correction. Eur J Cardiothorac Surg 2011;40:1138-45. [PubMed]
- Kravarusic D, Dicken BJ, Dewar R, et al. The Calgary protocol for bracing of pectus carinatum: a preliminary report. J Pediatr Surg 2006;41:923-6. [Crossref] [PubMed]
- Banever GT, Konefal SH, Gettens K, et al. Nonoperative correction of pectus carinatum with orthotic bracing. J Laparoendosc Adv Surg Tech A 2006;16:164-7. [Crossref] [PubMed]
- Frey AS, Garcia VF, Brown RL, et al. Nonoperative management of pectus carinatum. J Pediatr Surg 2006;41:40-5. [Crossref] [PubMed]
- Egan JC, DuBois JJ, Morphy M, et al. Compressive orthotics in the treatment of asymmetric pectus carinatum: a preliminary report with an objective radiographic marker. J Pediatr Surg 2000;35:1183-6. [Crossref] [PubMed]
- Mielke CH, Winter RB. Pectus carinatum successfully treated with bracing. A case report. Int Orthop 1993;17:350-2. [Crossref] [PubMed]
- Stephenson JT, Du Bois J. Compressive orthotic bracing in the treatment of pectus carinatum: the use of radiographic markers to predict success. J Pediatr Surg 2008;43:1776-80. [Crossref] [PubMed]
- Lee SY, Lee SJ, Jeon CW, et al. Effect of the compressive brace in pectus carinatum. Eur J Cardiothorac Surg 2008;34:146-9. [Crossref] [PubMed]
- Martinez-Ferro M, Fraire C, Bernard S. Dynamic compression system for the correction of pectus carinatum. Semin Pediatr Surg 2008;17:194-200. [Crossref] [PubMed]
- Martinez-Ferro M. International innovations in pediatric minimally invasive surgery: the Argentine experience. J Pediatr Surg 2012;47:825-35. [Crossref] [PubMed]
- Martinez-Ferro M. New approaches to pectus and other minimally invasive surgery in Argentina. J Pediatr Surg 2010;45:19-26. [Crossref] [PubMed]
- Lopez M, Patoir A, Varlet F, et al. Preliminary study of efficacy of dynamic compression system in the correction of typical pectus carinatum. Eur J Cardiothorac Surg 2013;44:e316-9. [Crossref] [PubMed]
- Cohee AS, Lin JR, Frantz FW, et al. Staged management of pectus carinatum. J Pediatr Surg 2013;48:315-20. [Crossref] [PubMed]
- Martinez-Ferro M, Bellia Munzon G, Ardigo L, et al. How to measure the pressure of correction (PC). Asvide 2016;3:167. Available online: http://www.asvide.com/articles/916
- Martinez-Ferro M, Bellia Munzon G, Ardigo L, et al. How to take the measurements of the thorax. Asvide 2016;3:168. Available online: http://www.asvide.com/articles/919
- Martinez-Ferro M, Bellia Munzon G, Ardigo L, et al. Fitting the FMF® Dynamic Compressor System. Asvide 2016;3:169. Available online: http://www.asvide.com/articles/924
- Martinez-Ferro M, Bellia Munzon G, Ardigo L, et al. Measurement of the PT. Asvide 2016;3:170. Available online: http://www.asvide.com/articles/925
- Martinez-Ferro M, Bellia Munzon G, Ardigo L, et al. Adjustment of the position of the compression plate. Asvide 2016;3:171. Available online: http://www.asvide.com/articles/926
- Martinez-Ferro M, Bellia Munzon G, Ardigo L, et al. Lateral expansion of the thorax when pectus carinatum is manually corrected. Asvide 2016;3:172. Available online: http://www.asvide.com/articles/927
Cite this article as: Martinez-Ferro M, Bellia Munzon G, Fraire C, Abdenur C, Chinni E, Strappa B, Ardigo L. Non-surgical treatment of pectus carinatum with the FMF® Dynamic Compressor System. J Vis Surg 2016;2:57.





