Video-assisted thoracic surgery right upper lobe bronchial sleeve resection
Introduction
Lung cancer is the most commonly diagnosed cancer as well as the leading cause of cancer death in males worldwide (1). Surgery for patients with non-small cell lung cancer (NSCLC) involving proximal bronchi can be challenging. Pneumonectomy is associated with high rates of complications, especially for patients with compromised pulmonary function. Sleeve lobectomy was introduced as an alternative to pneumonectomy (2). As a result, noninvolved lung parenchyma can be preserved for improving quality of life postoperatively. In 1952, Allison performed the first successful right upper lobe sleeve lobectomy for a patient with bronchogenic carcinoma (3). With the development of video-assisted thoracic surgery (VATS), locally advanced lung cancer, has been adapted for thoracoscopic lung resection and has obtained worldwide acceptance (4-10). However, a thoracoscopic approach is most commonly used for peripheral lesions (11,12). Central lung cancer was still considered a contraindication of thoracoscopic surgery. Thoracoscopic bronchial sleeve resection has only been reported in limited studies (13-16). This report describes a minimally invasive technique for VATS right upper lobe bronchial sleeve resection.
Methods
Clinical summary
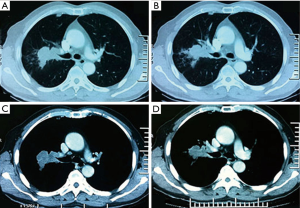
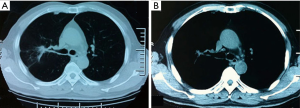
A 66 years old man was admitted for coughing for 2 months. He had smoked for 30 years, 20 packs a day. Chest computed tomography (CT) revealed a 2.5 cm × 4.5 cm mass in the right upper lobe (Figure 1). Bronchoscopy demonstrated the tumor obstructing the right upper lobe bronchus and involved the right main bronchus and bronchus intermedius. Pathology was squamous cell carcinoma. He received two cycles of neoadjuvant chemotherapy (gemcitabine 2.0 g day 1, 8 + cisplain 40 mg day 1–3). The lesion’s size reduced to 2.5 cm × 1.0 cm (Figure 2). There were no positive past medical history and co-morbidities. His pulmonary function result was forced expiratory volume in 1 second (FEV1): 1.91 L (64.7% predicted), forced vital capacity (FVC): 4.36 L.
Pre-operative assessment
Pneumonectomy is associated with high rates of complications, especially for patients with compromised pulmonary function (2). Sleeve lobectomy was an alternative to pneumonectomy. This patient’s lesion was located in the right upper lobe and was selected to be candidate for VATS sleeve resection. Preoperative workup included clinical history, physical examination, chest CT scan with intravenous contrast no more than 1 month before resection, pulmonary function test, blood gas analysis, cardiac evaluation, bronchoscopy and basic examinations as usual. Abdominal B-ultrasound, cerebral magnetic resonance imaging (MRI) and isotopic bone scanning were examinations to exclude metastatic disease. Fluorodeoxyglucose-position emission tomography (FDG-PET) was employed to exclude N2 disease.
Anaesthesia and positioning
This patient received general anesthesia with double-lumen endotracheal intubation and left lung ventilation. Left lateral decubitus position was chosen. His arms extended to 90° and the elbows flexed to 90°. And the operative table was flexed to maximize the intercostal space.
Technique
The first 1.5 cm incision was selected in the eighth intercostal space in the midaxillary line, and was used for the camera (30 degree 10 mm high definition video thoracoscope). A 4 cm long incision was made in the 3rd intercostal space in the preaxillary line (Figure 3). A third 1.5 cm incision was performed in the 9th intercostal space in the postaxillary line for assistant (Figure 4).

First, pulmonary ligament and the entire right hilum were mobilized with combination of sharp and blunt dissection. Second, pulmonary vein is the most forward hilar structure, sometimes immediately prior pulmonary trunk. The right upper lobe vein was transected with a vascular stapler (ETHICON 45 mm white stapler). Third, truncus and posterior ascending pulmonary artery were then divided and transected with a vascular stapler. Injury of the adjacent structures like azygos vein, phrenic and recurrent laryngeal nerves must be avoided during this step. Fourth, major and minor fissures were stapled by 60 mm green linear stapler.
Following clearance of the mediastinal lymph nodes of level 7, 4R and 2R, the bronchial sleeve resection and reconstruction began. Excision of these lymph nodes will facilitate exposure of the bronchus. The distal right main bronchus and bronchus intermedius were fully mobilized to ensure adequate surgical exposure. Traction sutures were routinely placed on the lateral walls and to reduce tension. Attention was then turned to bronchial anastomosis. The key point is to retract the two rings gently and allow the bronchus intermedius to the right main bronchus. Interrupted sutures were chosen for bronchial anastomosis. Bronchial membrane was sutured first, and then circumference end-to-end anastomoses were carried out using 3-0 absorbable sutures. The specimen was removed with a bag, and the two side of the bronchial resection margin were confirmed negative by frozen pathology. Afterwards, level 4R, 2R, and 3A were cleared. Bronchial anastomosis was confirmed without air leakage by water test. Finally, a 32F chest tube was placed 1.5 cm incision (8th intercostal space in the midaxillary line). Final pathology revealed T3N0M0 stage IIA squamous carcinoma.
Results
Post-operative management
Chest X-ray showed right middle and lower lobe reexpanded. Analgesia, antibiotics are used for three days postoperatively. There were no complications and the patient was discharged 8 days postoperatively.
Conclusions
The 3rd intercostal space of the anterior axillary line was suggested for right upper lobe bronchial sleeve resection. This incision can reduce the distance and angle between the anastomosis to the incision, providing convenient conditions for easy anastomosis. And avoid the operator fatigue for keeping the posture for a long time. Clearance of the mediastinal lymph nodes before cutting the bronchus was helpful for satisfied explosion of the right main bronchus, the upper lobe bronchus and bronchus intermedius. And this would avoid pulling bronchial anastomosis for mediastinal lymph nodes clearance. Interrupted suture was safe and effective for VATS bronchial anastomosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee. Written informed consent was obtained from the patient. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [PubMed]
- Wain JC. Bronchoplastic Resections. In: Kaiser LR, editor. Mastery of Cardiothoracic Surgery. Philadelphia: Lippincott-Raven, 1998:68-76.
- Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. [PubMed]
- Nakanishi R, Yamashita T, Muranaka K, et al. Thoracoscopic carinal resection and reconstruction in a patient with mucoepidermoid carcinoma. J Thorac Cardiovasc Surg 2013;145:1134-5. [PubMed]
- Xu X, Chen H, Yin W, et al. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg Innov 2014;21:481-6. [PubMed]
- Jiao W, Zhu D, Cheng Z, et al. Thoracoscopic tracheal resection and reconstruction for adenoid cystic carcinoma. Ann Thorac Surg 2015;99:e15-7. [PubMed]
- Zhao G, Dong C, Yang M, et al. Totally thoracoscopic tracheoplasty for a squamous cell carcinoma of the mediastinal trachea. Ann Thorac Surg 2014;98:1109-11. [PubMed]
- Nakanishi K, Kuruma T. Video-assisted thoracic tracheoplasty for adenoid cystic carcinoma of the mediastinal trachea. Surgery 2005;137:250-2. [PubMed]
- Zhang R, Xia W, Yu Z, et al. Complete video-assisted thoracic surgery right upper lobe sleeve resection. J Thorac Dis 2013;5 Suppl 3:S331-2. [PubMed]
- Yang R, Shao F, Cao H, et al. Bronchial anastomosis using complete continuous suture in video-assisted thoracic surgery sleeve lobectomy. J Thorac Dis 2013;5 Suppl 3:S321-2. [PubMed]
- Swanson SJ, Herndon JE 2nd, D'Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802--a prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [PubMed]
- Kim K, Kim HK, Park JS, et al. Video-assisted thoracic surgery lobectomy: single institutional experience with 704 cases. Ann Thorac Surg 2010;89:S2118-22. [PubMed]
- Nakanishi K. Video-assisted thoracic surgery lobectomy with bronchoplasty for lung cancer: initial experience and techniques. Ann Thorac Surg 2007;84:191-5. [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [PubMed]
- Kamiyoshihara M, Nagashima T, Igai H, et al. Video-assisted thoracic lobectomy with bronchoplasty for lung cancer, with special reference to methodology. Interact Cardiovasc Thorac Surg 2011;12:534-8. [PubMed]
- Schmid T, Augustin F, Kainz G, et al. Hybrid video-assisted thoracic surgery-robotic minimally invasive right upper lobe sleeve lobectomy. Ann Thorac Surg 2011;91:1961-5. [PubMed]
- Ma Q, Liu D. Video-assisted thoracic surgery (VATS) right upper lobe bronchial sleeve resection. Asvide 2016;3:028. Available online: http://www.asvide.com/articles/779
Cite this article as: Ma Q, Liu D. Video-assisted thoracic surgery right upper lobe bronchial sleeve resection. J Vis Surg 2016;2:18.