Nonintubated uniportal video-assisted thoracic surgery course—live surgery
“Uniportal video-assisted thoracic surgery (VATS) course—live surgery” was held on 23rd of November 2015 in Lithuania, The Hospital of Lithuanian University of Health Sciences Kaunas Clinics. It was organised by the Department of Cardiothoracic and Vascular Surgery together with The Lithuanian Society of Cardiothoracic Surgeons. This international event has attracted many thoracic surgeons, doctors anesthesiologists-reanimatologists, operative theatre nurses and other medical specialists from Lithuania, Latvia, Estonia and Poland. The special guests of the conference were worldwide famous Spanish thoracic surgeon Dr. Diego Gonzalez-Rivas and his colleague doctor anesthesiologist Dr. Humberto Aymerich Cano.
Dr. Diego Gonzalez-Rivas is a highly skilled thoracic surgeon and world leading expert in uniportal VATS. He has performed the first uniportal VATS lobectomy on 29th of July, 2010. Since then, this innovative technique has been adopted in many countries of Europe, Asia, North and South America. Although general anesthesia with intubation and one lung ventilation was traditionally considered to be necessary for major thoracoscopic pulmonary resections, the first nonintubated VATS for lobectomy was initially described in 2007. Avoidance of general anesthesia results in a faster recovery, immediate return to daily life activities and minimizes the adverse effects of tracheal intubation and general anesthesia.
Dr. Diego Gonzalez-Rivas has presented some reports concerning the recent advances in the uniportal VATS and the thoracoscopic surgery technique performed for a nonintubated patient. The anesthetic protocol for a non-intubated VATS was also presented by doctor anesthesiologist Dr. Humberto Aymerich Cano. The attendees of the conference had a unique possibility not only to know about this minimally invasive surgery technique, but also to see the surgeries performed live.
Cases
We have performed two uniportal VATS lobectomies for a nonintubated patient. This kind of surgical procedures in our institution were performed for a first time.
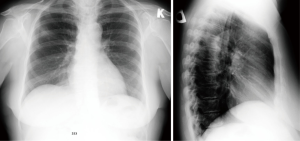
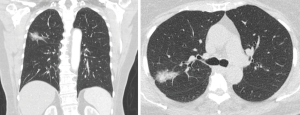
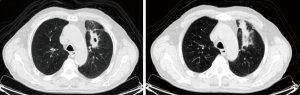
The first case was a 70 year old female, who was diagnosed with non-small cell lung cancer in the right upper lobe. She has complained of a dry cough for about 3 weeks. Chest X-ray showed a shadow in the right lung S2 area (Figure 1). Chest CT (Figures 2,3) and PET-CT scan has confirmed ~1.6 cm × 2.8 cm tumor in the right lung S2 zone, mediastinal lymph nodes: right paratracheal ~0.6 cm, right bronchopulmonary calcified up to 1.0 cm; FDG negative. Fibrobronchoscopy showed no endobronchial changes and transbronchial biopsy (TBB) has confirmed lepidic adenocarcinoma diagnosis. This patient is non-smoker, had no oncological anamnesis and has some comorbidities: arterial hypertension, type 2 diabetes, obesity [body mass index (BMI) 31.2 kg/m2] and benign non-toxic multinodular thyroid enlargement deviating trachea to the left. Nonintubated uniportal VATS right upper lobectomy and mediastinal lymphadenectomy was performed (Figure 4).
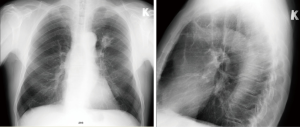
The second case was a 68-year-old male. He was diagnosed with non-small cell lung cancer in the left upper lobe. The patient is a smoker for about 45 years, he smokes 10–20 cigarettes per day, has arterial hypertension, BMI is normal (24.5 kg/m2). More than a year before he was diagnosed with colon cancer, right hemicolectomy was performed and histopathology confirmed adenocarcinoma, stage IIIB, he got adjuvant treatment. The patient has complained of a fatigue and dry cough. The chest X-ray showed ~4 cm × 3 cm tumor in the left lung S1-2 area (Figure 5). Chest CT (Figures 6,7) and PET-CT scan showed ~4.1 cm × 2.6 cm × 2.4 cm FDG positive tumour in the left lung S1-2 zone and tumorous infiltration extending to the front till the parietal pleura; small mediastinal lymph nodes with minimal FDG consumption. TBB has confirmed infiltrative squamous cell carcinoma diagnosis. This patient had nonintubated VATS left upper lobectomy and mediastinal lymphadenectomy (Figure 8).


Surgical technique
The patient was positioned in the lateral decubitus position. The oxygen was administered via face mask. Intravenous sedation was achieved by using propofol and remifentanil. The skin and intercostal space were infiltrated with levobupivacaine. A single 3 cm skin incision was made in the 5th intercostal space. The surgeon and assistant were positioned in the front of the patient. The 30˚ high definition thoracoscope, specially designed curved thoracoscopic instruments, endostaplers and vascular clips were used. The camera was placed in the posterior part of the incision and the instruments were placed below the camera. Vagus nerve blockade with local anesthetic was used to reduce cough reflex. The patient was breathing spontaneously, but the collapse of the ipsilateral lung was really good and the movements of the diaphragm were minimal. Lobectomy and mediastinal lymphadenectomy was performed. The lung was extracted in a protective bag. A single chest tube was inserted through the same incision and placed posteriorly at the end of the procedure.
Results
The vital signs of the patients were stable during the surgery. After returning to supine position the patients were already awake and were transferred to the intensive care unit for a full recovery. The patients were allowed to drink and eat after 2 hours and were sent back to the thoracic surgery department ward. Both patients have recovered after the surgery fast and easy. Postoperative pain was minimal. Chest tube was removed after 2 days and the patients were discharged to a rehabilitation centre.
Conclusions
These successful examples demonstrate a minimally invasive surgical technique—uniportal VATS lobectomy for a nonintubated patient. It is important to mention that the procedures were performed by a team of experienced anesthesiologist and a highly skilled single port VATS surgeon.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Karalevičiūtė R, Gonzalez-Rivas D. Chest CT scan video shows ~1.6 cm × 2.8 cm tumor in the right lung S2 zone. Asvide 2016;3:018. Available online: http://www.asvide.com/articles/769
- Karalevičiūtė R, Gonzalez-Rivas D. Nonintubated uniportal VATS right upper lobectomy and mediastinal lymphadenectomy was performed. Asvide 2016;3:019. Available online: http://www.asvide.com/articles/770
- Karalevičiūtė R, Gonzalez-Rivas D. Chest CT scan video shows ~4.1 cm × 2.6 cm × 2.4 cm tumor in the left lung S1-2 zone and tumorous infiltration extending to the front till the parietal pleura. Asvide 2016;3:020. Available online: http://www.asvide.com/articles/771
- Karalevičiūtė R, Gonzalez-Rivas D. Nonintubated VATS left upper lobectomy and mediastinal lymphadenectomy was performed. Asvide 2016;3:021. Available online: http://www.asvide.com/articles/772
Cite this article as: Karalevičiūtė R, Gonzalez-Rivas D. Nonintubated uniportal video-assisted thoracic surgery course—live surgery. J Vis Surg 2016;2:15.