
A novel procedure of thoracoscopic 4L lymph node dissection: 4L posterior first technique
Introduction
The left lower paratracheal (4L) lymph nodes are important components of the lymphatic pathway of the left lung (1-3). Several recent retrospective studies found that 4L lymph node dissection was associated with favorable survival outcomes in patients with left-sided lung cancer (4,5). However, surgeons do not always dissect 4L lymph nodes because dissecting these nodes increases the possibility of left recurrent nerve damage. Station 4L lymph node dissection is more difficult than lymphadenectomy of other stations because of the different anatomic configurations of the aortic arch, pulmonary artery, and left recurrent laryngeal nerve.
We developed a novel procedure of thoracoscopic 4L lymph node dissection, which involves the dissection of the posterior side of 4L lymph nodes followed by that of the hilar structure. This 4L posterior first technique enables en bloc retraction of nodal packet with lung, pulmonary artery, and vagus and left recurrent nerves; this retraction provides an excellent surgical view. This novel method of thoracoscopic 4L lymph node dissection reduces the amount of blood loss during hilar and mediastinal lymph node dissection because it involves the division of bronchial arteries that arise from the aortic root as an initial step.
This study aimed to describe the novel procedure of thoracoscopic 4L lymph node dissection using the confronting upside-down monitor setting and to determine the surgical outcomes.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocols followed for data collection and analysis were approved and the requirement for obtaining informed consent from each patient was waived by the Institutional Review Board (approval number: 2019-1209).
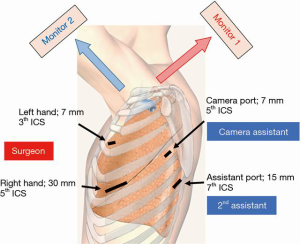
Confronting upside-down monitor setting
A thoracoscopic lobectomy with lymph node dissection is performed using four ports (7, 7, 15, and 30 mm) with confronting upside-down monitor setting (Figure 1) (6,7). Two monitors are installed on the cranial side of the patient, and one of the monitors is placed upside down. The surgeon stands on the right side of the patient regardless of the operation side (in a left-sided operation, ventral side). The camera and secondary assistants stand on the left side of the patient. During a left-sided surgery, the secondary assistant focuses on providing the surgeon with a better view of the surgical site by placing two instruments using a 15-mm port in the seventh intercostal space. The camera assistant places a 7-mm port in the fifth intercostal space and can visualize all structures in the chest cavity with a 30-degree scope. A 30-mm utility incision is made in the fifth intercostal space, and a 7-mm port is inserted in the third intercostal space for the operator’s right hand. In this setting, the surgeon can use both hands freely and perform a sharp dissection using traditional Metzenbaum scissors.
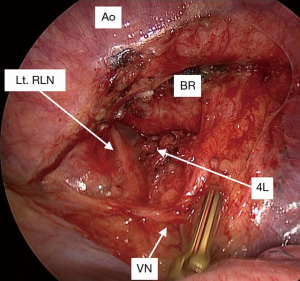
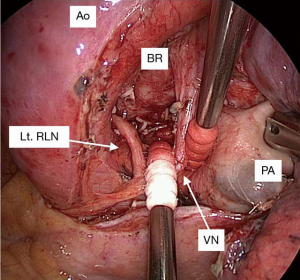
4L posterior first technique
In this 4L posterior first technique, the posterior side of the 4L lymph nodes is dissected first. At the start of the operation, the assistant surgeon retracts the lung anteriorly. The pleura of the dorsal side of the hilum is divided, and the bronchial arteries arising from the aorta are clipped and divided with a surgical energy device. The left main bronchus is dissected cranially using scissors. The vagus nerve is exposed, and the left recurrent nerve is dissected distally. The dissection of the posterior side of the nodal packet including 4L lymph nodes and the surrounding structures, such as the left main bronchus, aortic arch, and vagus and left recurrent nerves, is completed before touching the hilar structures (Figure 2). Further, lobectomy and mediastinal lymph node dissection are performed in a conventional manner (Figure 3). Lobe-specific systematic lymph node dissection is usually performed (8). Subcarinal lymph node dissection is omitted in patients with lung cancer localized in the left upper segment, whereas complete mediastinal lymph node dissection including stations 4L, 5, 6, 7, 8, and 9 is performed in those with lung cancer in the left lower lobe (Video 1). It is easy to perform 4L lymph node dissection because the left recurrent nerve has already been dissected and we just have to dissect the anterior part of 4L.
Data collection and statistical analysis
The operative and clinical records of the patients who underwent thoracoscopic 4L lymph node dissection between 2016 and 2018 were retrospectively analyzed. The stations of lymph nodes were defined according to the lymph node map proposed in 2009 by the International Association for the Study of Lung Cancer (10). A comparison between the novel method group and the conventional method group matching the surgical procedure and main operator was performed. The surgical procedure was limited to thoracoscopic left upper lobectomy with lobe-specific mediastinal lymph node dissection omitting subcarinal lymphadenectomy. The patients with lung cancer invading the chest wall or broad pleural adhesions were excluded. In this study, one of the four experienced general thoracic surgeons (M Mun, M Nakao, Y Matsuura, and J Ichinose) performed the operation. The main operators were divided as follows: the senior surgeon (M Mun) and the junior surgeons (M Nakao, Y Matsuura, and J Ichinose), and the ratio of the senior to the junior surgeons was matched (1:2) in both of the conventional method group and the novel method group. The matched comparison was analyzed using IBM SPSS Statistics version 25 software (SPSS Inc., Chicago, IL, USA). Variables were compared using the Student’s t-test or Fisher’s exact test. P<0.05 was defined as statistically significant.
Results
From January 2016 to November 2018, 99 consecutive patients with primary lung cancer of the left upper lobe underwent thoracoscopic left upper lobectomy and systematic lymph node dissection. In 21 patients, 4L lymphadenectomy was omitted because of oncological reasons or patients’ comorbidities. Forty (51%) of 78 patients underwent thoracoscopic 4L lymphadenectomy using the novel method: 4L posterior first approach. The operation time was 200±41 min, whereas the volume of blood loss was 27±28 mL. The length of postoperative hospital stay was 6±3 days. No 90-day and in-hospital mortality were reported, and none of the patients were converted to thoracotomy.
To evaluate the utility of the novel method, 37 patients from the novel method group and 27 from the conventional method group matching the surgical procedure and main operator were compared (Table 1). Results showed that the operation time was shorter (194±33 vs. 218±41 min, P=0.01) and the amount of blood loss was relatively smaller (22±21 vs. 33±21 mL, P=0.06) in the novel method group. Transient recurrent nerve paralysis was noted in one patient from the conventional method group (3.7%) and in no one from the novel method group (0%).
Table 1
| Variable | Novel method group | Conventional method group | P |
|---|---|---|---|
| Number of cases | 37 | 27 | |
| Operation time (min) | 194±33 | 218±41 | 0.01 |
| Amount of bleeding (mL) | 22±21 | 33±21 | 0.06 |
| Recurrent nerve paralysis | 0 (%) | 1 (3.7%) | 0.87 |
Discussion
In our initial experience, our 4L posterior first technique was a useful procedure, which shortened the operation time and reduced the amount of bleeding in thoracoscopic left upper lobectomy with systematic mediastinal node dissection.
This approach has two advantages. First, it provides an excellent surgical view of the left recurrent nerve. In this method, the 4L lymph nodes are initially dissected prior to the dissection of hilar structures. This technique enables en bloc retraction of the lung with nodal packet, pulmonary artery, and vagus and left recurrent nerves. The assistant surgeon retracts the lung using only a single instrument. The most difficult and important part of 4L lymph node dissection is the sufficient exposure of the left recurrent nerve. The en bloc retraction allows the application of adequate tension to the left recurrent nerve and makes it easier to dissect the recurrent nerve to the distal side. Although some surgeons do not expose the left recurrent nerve for fear of nerve damage including nerve palsy, we believe that sufficient exposure of the left recurrent nerve is essential to the satisfactory removal of 4L lymph nodes and avoidance of recurrent nerve injury.
Second, this method reduces the amount of bleeding during lymph node dissection, because the bronchial arteries arising from the aortic root are initially divided. In the conventional method, the distal part of the bronchial arteries is divided to perform hilar lymph node dissection; further, the proximal part of the bronchial arteries are divided again to perform mediastinal lymph node dissection. Performing the division twice may cause unnecessary bleeding.
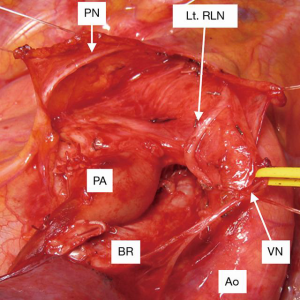
However, the novel method described in this study has been performed earlier. Our predecessors, Dr. Ken Nakagawa and Dr. Sakae Okumura, had performed 4L lymphadenectomy via thoracotomy using the same technique, i.e., initially dissecting the posterior side of 4L (Figure 4). Traditional surgical techniques developed over a long period of time and through experience with open surgery have a precious value also in minimally invasive procedure, such as thoracoscopic surgery and robot-assisted thoracic surgery.
In conclusion, our 4L posterior first technique provides an excellent surgical view during 4L lymphadenectomy by en bloc retraction and reduces the amount of bleeding during lymph node dissection by dividing the bronchial arteries first. This novel procedure enables the surgeon to perform thoracoscopic 4L lymph node dissection more easily and accurately.
Acknowledgments
Presented at the 36th Annual Conference of Japanese Association for Chest Surgery, Osaka, Japan, May 16–17, 2019. The authors sincerely thank Dr. Ken Nakagawa and Dr. Sakae Okumura for teaching them the techniques of performing precise lymphadenectomy.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Meinoshin Okumura) for the series “Dedicated to the 36th Annual Conference of Japanese Association for Chest Surgery (JACS)” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs.2019.11.12/coif). The series “Dedicated to the 36th Annual Conference of Japanese Association for Chest Surgery (JACS)" was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocols followed for data collection and analysis were approved and the requirement for obtaining informed consent from each patient was waived by the Institutional Review Board (approval number: 2019-1209).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hata E, Troidl H, Hasegawa T. In-vivo-Untersuchungen der Lymphdrainage des Bronchialsystems beim Menschen mit der Lympho-Szintigraphie-eine neue diagnostische Technik. Behandlung des Bronchialkarzinoms 1st ed Stuttgart: Georg Thieme Verlag 1981:27-34.
- Nohl-Oser HC. An investigation of the anatomy of the lymphatic drainage of the lungs as shown by the lymphatic spread of bronchial carcinoma. Ann R Coll Surg Engl 1972;51:157-76. [PubMed]
- Riquet M, Arame A, Foucault C, et al. Prognostic classifications of lymph node involvement in lung cancer and current International Association for the Study of Lung Cancer descriptive classification in zones. Interact Cardiovasc Thorac Surg 2010;11:260-4. [Crossref] [PubMed]
- Zhao K, Wei S, Mei J, et al. Survival Benefit of Left Lower Paratracheal (4L) Lymph Node Dissection for Patients with Left-Sided Non-small Cell Lung Cancer: Once Neglected But of Great Importance. Ann Surg Oncol 2019;26:2044-52. [Crossref] [PubMed]
- Wang YN, Yao S, Wang CL, et al. Clinical Significance of 4L Lymph Node Dissection in Left Lung Cancer. J Clin Oncol 2018;36:2935-42. [Crossref] [PubMed]
- Mun M, Nakao M, Matsuura Y, et al. Video-assisted thoracoscopic surgery lobectomy for non-small cell lung cancer. Gen Thorac Cardiovasc Surg 2018;66:626-31. [Crossref] [PubMed]
- Mun M, Ichinose J, Matsuura Y, et al. Video-assisted thoracoscopic surgery lobectomy via confronting upside-down monitor setting. J Vis Surg 2017;3:129. [Crossref] [PubMed]
- Ichinose J, Kohno T, Fujimori S, et al. Locoregional control of thoracoscopic lobectomy with selective lymphadenectomy for lung cancer. Ann Thorac Surg 2010;90:235-9. [Crossref] [PubMed]
- Ichinose J, Matsuura Y, Nakao M, et al. How thoracoscopic left lower lobectomy with systematic mediastinal lymph node dissection is performed using 4K video-thoracoscopy. Asvide 2020;7:025. Available online: http://www.asvide.com/watch/33042
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
Cite this article as: Ichinose J, Matsuura Y, Nakao M, Mun M. A novel procedure of thoracoscopic 4L lymph node dissection: 4L posterior first technique. J Vis Surg 2020;6:11.


