Subcoronal inflatable penile prosthesis under local anesthesia
Introduction
For the past 45 years, infrapubic and penoscrotal incisions have been utilized for inflatable penile prosthesis (IPP) surgery. Both these techniques require general or regional anesthesia. Sporadic reports utilizing these incisions with local anesthesia admitted to considerable patient discomfort and distortion of the surgical fields caused by the injection of considerable volumes of the local. Because IPP is not reimbursed by third parties in South Korea, we wished to obviate the need and the associated cost for an anesthesiologist. With the detailed instructions and participation of known high volume implanters, Robert Valenzuela, Allen Morey and Steven Wilson, we adapted the subcoronal surgical incision to local anesthesia 5 years ago and have successfully utilized the technique on hundreds of Korean men with success.
Anesthetic agents used are 1% lidocaine and 0.75% ropivacaine 1:1 mixture. 25G 1.5-inch needle on 10 cc syringe was employed for injection. LA is achieved stepwise fashion in each section; preoperative and intraoperative stage. This section will describe LA according to surgical steps.
Preoperative LA—pudendal, penile root and direct inguinal block:
- Pudendal block—for initial skin preparation with chlorhexidine-alcohol based solution, patient was placed as frog leg position. After skin preparation, scrotum is push upward by left palm, left index finger was placed above the urethra to protect it and 3rd flinger tip was placed on crus of left corpus cavernosum. While needle was slightly tilted toward ipsilateral nipple, space between index and 3rd fingertip was punctured and when needle in introduced about 5 cc was injected. Same method was done on the contralateral side emptying the 10 cc syringe.
- Penile root block—to reach sub-dartos layer, penile skin was pinched & lifted in full thickness. This was done to prevent accidental vessel puncture and to achieve better anesthetic effect. 2cc was injected each 3, 6, 9 and 12 o’clock side of penile root. (Total volume 8 cc).
- Direct inguinal block—by introducing Rt. index finger through the scrotum, right external (superficial) inguinal ring was located. Right pubic tubercle is a useful land mark since external inguinal ring is located just above it. After locating external inguinal ring, right index finger was retracted slightly. Puncture was done where external inguinal ring was located while needle was tilted inferiorly to hit the pubic bone. After introducing the needle, right index finger is advanced to guide the needle exactly into the inguinal ring. 5 cc was injected on external inguinal ring and 2 cc on layers above the external inguinal ring during the retraction of needle. Total preoperative injection: 25 cc.
Intraoperative LA—scrotal wall anterior to proximal corpora, scrotal septum, proximal corpora where incision will be made, external inguinal ring:
- Scrotal wall anterior to proximal corpora—1–2 cc of injection was done to each side of space anterior to the proximal corpora, manipulation of this area tends to cause pain even with the successful pudendal block.
- Scrotal septum—after developing anterior proximal corporal space, 1–2 cc was injected to scrotal septum while Deavers are retracting Buck’s fascia. Care should be taken not to puncture the urethra.
- Proximal corpora where incision will be made—after placing stay suture where corporal incision will be made, 1–2 cc of intracorporal injection was done to each corpus cavernosum. Note that proximal corporal dilation tends to cause more discomfort than distal dilation. Total intraoperative injected volume: 7 cc.
External inguinal ring—this could be done in case initial direct inguinal block was not successful and patient complains of pain. While retracting the inguinal ring gently with the Deaver, 3–5 cc of additional injection will achieve inguinal anesthesia. If this fails again because of ambiguous anatomy or patient’s abdominal straining, conscious sedation (e.g., Propofol, etomidate etc.) should be employed through the intravenous line. In case of submuscular reservoir placement, etomidate was particularly chosen due to its muscle relaxation effect.
There are other videos available on www.vjpu-issm.info showing deployment of local anesthesia during IPP (1,2).
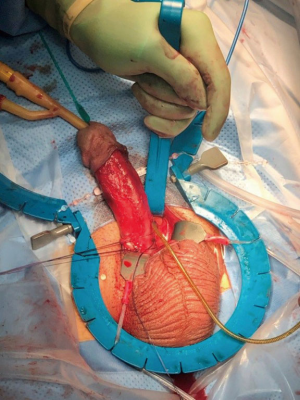
Surgical technique (Figure 1)
0.2 cc of Trimix was injected before the shaving for corporal relaxation, to aid corporal dilatation and for delineation of any penile curvature. After placing 14 Fr Foley catheter, bladder was drained. Circumferential subcoronal skin incision with complete incision of Dartos and gentle degloving is performed. We find the disposable Wilson (Coloplast) or SKW (Boston Scientific) Retractors useful to provide axial support for the penis and thereby lessen frequency of crossover or urethral laceration.
When penoscrotal junction was exposed, Buck’s fascia is pierced deep to anterior corpora with mosquito clamp on each corpora and baby deaver is placed in defect. After placing baby Deaver on each side, Deavers are displaced caudal to expose proximal corpora thereby exposing the septum of the scrotum. The septum is incised for a short distance which will prevent cylinder tubing being visible under the penile or scrotal skin. (tail pipe penis) (Figure 2). This had been a common patient complaint prior to using the Deaver maneuver. Vicryl 2-0 on UR-6 needle was placed as stay sutures in both corpora proximal to the penoscrotal junction. The corpora are incised 1.5 cm between the stay sutures with No. 15 blade. Measurement was done with Furlow inserter and dilation of proximal corpora was done with 12 Brooks dilator.
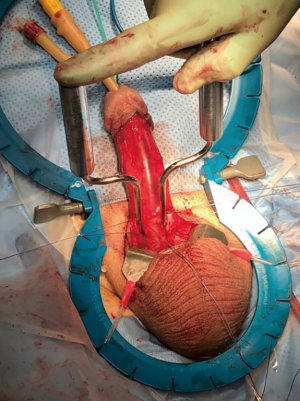
Right external inguinal ring was located with examining finger and retracted with a baby Deaver. Kelly clamp was utilized to pierce Transversalis fascia to make a space for the reservoir. After securing the Retzius space, reservoir was placed and filled (Figure 3). We use a similar technique to place ectopic or high submuscular reservoirs when pelvic anatomy is compromised. It is not our method of choice since it requires additional conscious sedation.
Cylinders were placed and stay sutures were tied to close the corporotomy. Pump was placed in the scrotum posterior to the Dartos layer. 18 Fr. Blake suction drain was placed on contralateral side of prepubic area where reservoir was placed, and skin circumcision incision closed after careful replacement and closure of the Dartos tissue. Compression dressing was applied.
Results
From Jan, 2015 to Dec, 2018, IPP surgery via subcoronal incision under LA was done to 557 Korean men. All cases were first time patients. Mean OR time was 52.54 minutes, mean total volume of injected anesthetic agent was 33.58 mL. Mean subjective patient pain scale during local anesthesia administration was 2.74, during the surgery was 4.24 and on postoperative day 1 was 2.5. Reservoir was placed in space of Retzius (505 cases, 90.6%), submuscular area (50 cases, 8.97%) and Rectus Sheath through counter incision (2 cases, 0.35%). All ectopic reservoir placement cases were supplemented with conscious sedation and 32 of reservoirs placed in Space of Retzius (84 total cases, 15%). Transient systemic symptom of hypotension due to lidocaine injection was noticed among 101 cases (18%) which resolved with oxygen support, fluid infusion and reverse Trendelenburg position. There was no case of conversion to spinal or general anesthesia and 485 patients (87%) said that they will have IPP surgery again under local anesthesia. 137 patients (24.6%) experienced postoperative transient preputial edema which lasted 2 weeks to 6 months. There were 2 cases of distal preputial partial skin necrosis which recovered with conservative treatment without further complication. Infection rate was 0.53% (3 cases). Tubing protrusion was noted in 12 cases and revision was necessary in 2 cases. This complication ceased after employment of the Deaver Maneuver and use of the disposable retractor. 1 case of distal crossover was missed intraoperatively and required revision surgery.
Discussion
Over the past 45 years, surgical techniques for IPP placement have evolved to achieve the optimum postoperative outcome—patient safety and satisfaction. Avoidance of regional or general anesthesia could enhance this goal.
The decision of anesthetic method depends upon preoperative patient consultation with respect to cost and convenience. To our knowledge there is no contraindication to LA with IPP surgery, yet patients for whom cost is no object or who have a desire to be asleep might opt out. On the other hand, patient’s with systemic comorbidities making more extensive anesthesia dangerous might opt into LA.
LA has advantages and disadvantages. The possible advantages could be (I) better postoperative pain control (4); (II) convenience; (III) reduced cost; (IV) enabling operability when patient is a poor candidate of general or spinal anesthesia. Possible disadvantages could be (I) discomfort and memory of the pain during the surgery; (II) possibility of unsuccessful anesthesia; (III) limited duration (1–3 hours); (IV) patient movement during the surgery. Because of these reasons, author strongly suggests LA only be utilized by frequent implanter since patient lucidity and movement can make an occasional surgeon nervous and surgeon speed is advantageous.
Several points must be recognized concerning IPP with LA. First, LA is not completely pain free. Surgeon should discuss this aspect with the patient preoperatively. Conscious sedation can markedly help when patient is uncomfortable or wishes to be “out of it”. It is recognized that in some countries (e.g., USA) conscious sedation requires specially trained medical staff present in the operating room if this sedation is employed. This requirement is not mandatory in Korea. Second, systemic absorption of anesthetic agent may cause side effects. To prevent this, authors try to limit the dosage below 35 cc regardless of patient’s body weight. Even within the safety margin of local anesthetic dosage, usually less than 40 cc of the mixture, patient can experience transient hypotensive symptoms. When this occurs, reverse Trendelenburg position, oxygen mask and fluid infusion should be applied immediately while explaining to the patient to prevent panic which can aggravate the symptom. As a safety measure, aspiration of the syringe should always be done prior to injection of the LA to prevent intravascular administration of anesthetic agent. We prefer staged LA as there are case reports about anaphylactic response toward the local anesthetic agent (5). Third, LA should be reserved for first time implant patients. Pseudo capsule which forms around the implant components tends to be resistant to pudendal and direct inguinal block (6). In case of device infection, we do not employ LA for the removal of the infected device because of theoretical worry about further spreading the infection.
Subcoronal approach is much similar to penoscrotal approach in terms of reservoir and pump placement. However, corporal dilation is similar to infrapubic approach as penile axis is not fixed. Due to this, one should always think about penile alignment to prevent distal crossover. Applying disposable Wilson retractor (Coloplast) or SKW retractor (AMS) could help align penile axis. To achieve meticulous 2-layer skin closure, initial circumferential transection of complete Dartos layer should be done. Most common postoperative patient complaint is painless preputial edema which can last up to 6 months. All cases resolved with conservative treatment.
Author’s initial experience of LA with penoscrotal approach of IPP surgery showed that scrotal dissection became more difficult due to the bloating of anatomical layers after the anesthetic injection. In the subcoronal approach, however, surgical landmarks and planes are not affected by the LA.
Conclusions
Subcoronal approach under local anesthesia is cost effective in patients without third party reimbursement because it eliminates the cost of administration of general or regional anesthesia. While there is mild discomfort during the LA administration and the subsequent surgery, it is usually tolerated by first time implant patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Martin Gross, Jay Simhan and Faysal A. Yafi) for the series “Penile Prosthesis Surgery” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.07.04). The series “Penile Prosthesis Surgery” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Park SH. How to perform an IPP under local anesthesia. VJPU 2018;2:123.
- Park SH. Subcoronal IPP Under Local Anesthesia with Modified Wilson's Deaver Maneuver. VJPU 2016;2:083. Available online: https://www.vjpu-issm.info/videos/peer-reviewed/1-penile-prosthesis-malleable-inflatable-penile-prosthesis-ipp/1-a-first-time-implant/item/98-subcoronal-ipp-under-local-anesthesia-with-modified-wilson-s-deaver-maneuver
- Park SH. Employment of local anesthesia: steps and technique. Asvide 2019;6:212. Available online: http://www.asvide.com/watch/32895
- Tong CMC, Lucas J, Shah A, et al. Novel multi-modal analgesia protocol significantly decreases opioid requirements in inflatable penile prosthesis patients. J Sex Med 2018;15:1187-94. [Crossref] [PubMed]
- Chan TYK. Fatal anaphylactic reactions to lignocaine Forensic Sci int 2016;266:449-52. [Crossref] [PubMed]
- Park SH. How to perform a revision IPP under local anesthesia. VJPU 2018;2:129.
Cite this article as: Park SH. Subcoronal inflatable penile prosthesis under local anesthesia. J Vis Surg 2019;5:65.