Uniportal video-assisted thoracoscopic lobectomy surgery for lung cancer—case report
Introduction
Recently, uniportal video-assisted thoracoscopic surgery (VATS) of lung resection is growing in many thoracic surgery units all over the world (1). Uniportal VATS lobectomy has shown to be associated with less postoperative pain and analgesia requirement, less duration of postoperative intercostal chest tube drainage, and also reported shorter recovery time when compared to multi-port VATS lobectomy (2). Uniportal VATS lobectomy is believed to be safe and feasible technique with good outcome in selected centers (3).
The first uniportal VATS lobectomy with mediastinal lymph nodes dissection was done in 2011 by Dr. Gonzalez-Rivas who is an expert in uniportal VATS (4). Since that time, this new technique has been adopted in many places all over the world. However, in Feb. 2016, uniportal VATS was successfully performed for the first time in our center.
Case presentation
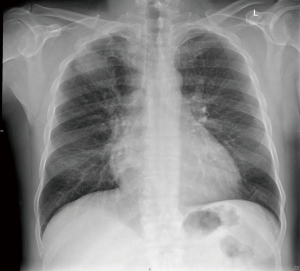
We report a 62-year-old male, presented with shortness of breath and cough. He is diabetic, hypertensive, and is known to suffer from chronic obstructive pulmonary disease (COPD). He is a heavy smoker for more than 40 years. His chest X-ray showed right upper lobe mass (Figure 1).
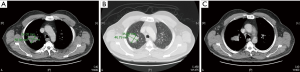
Enhanced chest and abdomen CT scan confirmed a right upper lobar pulmonary mass lesion with small necrotic changes with irregular edges (Figure 2A,B,C). Tru-Cut biopsy confirmed the diagnosis of non-small cell carcinoma, consistent with squamous cell carcinoma, moderately differentiated with prominent necrosis. However, complete staging performed which showed few but less than 1 cm in diameter of mediastinal lymph nodes in the right para-tracheal area, but no distant metastatic lesions found in the abdomen, brain or bones.
Procedure
This patient was assessed preoperatively by anesthesia and cardiology teams. He underwent general anesthesia with one lung ventilation through left side double lumen tube. The pleural cavity approached through a single port by performing a 4–5 cm skin incision in the anterior chest wall at the third intercostal space, right upper lobectomy was done through this incision using Thoracoscopic lobectomy instruments and also a complete mediastinal lymphadenectomy performed of station 3, 4, and station 7 (Figure 3). Patient was extubated immediately after the procedure. He stayed one day overnight in the intensive care unit (ICU), till he was transferred to the ward. Postoperative pain was controlled by minimal dose of analgesia through patient-controlled analgesia (PCA) using morphine. Postoperative course was uneventful without any complications, after few days he was discharged home in a good and a stable condition. He remained very well in regular follow up in the outpatient clinic for the next 18 months.
Results
The macroscopic pathological finding of the specimen consisted of a mass measuring 15 cm × 8 cm × 6 cm. However, the microscopic findings showed a necrotizing and poorly differentiated squamous cell carcinoma of the lung (grade 3). The tumor is unifocal. It extends close to but not beyond the pleural surface of the specimen. The lymph nodes dissection was positive in stations R3, R4. The pathological staging of the neoplasm was: T2aN2M0, which required post-operative adjuvant chemotherapy.
Discussion
Uniportal VATS has become very popular worldwide to treat thoracic surgical diseases, such as benign and malignant lung tumors and pleural pathologies (6). It has been proven to be safe and feasible technique with good outcome, also has shown to be associated with less postoperative morbidity, less duration of postoperative drainage, with less postoperatively analgesia requirement and fast recovery time (3,7). However, uniportal VATS and lung resection has gained recently popularity in some selected thoracic surgery centers for the above reasons (3,4,6,7), in addition, the feasibility of the conversion during the procedure if there are any difficulties or complications encountered such as, bleeding, lymph node invasion or adhesion, the surgeons may convert from uniportal VATS to formal thoracotomy for the patient’s interest, which should not be considered as failure of the procedure (7).
Our case report representing uniportal VATS right upper lobectomy with complete mediastinal lymph nodes dissection, which was done as first case in Saudi Arabia on February 2016. Under general anesthesia with one lung ventilation, the patient had 4–5 cm incision in the anterior chest wall at the right third intercostal space. Post-operative recovery was uneventful, and he continue to be asymptomatic without any distal metastasis on regular follow-up in the outpatient clinics for the next 15 months.
Conclusions
In conclusion, uniportal VATS lobectomy is a minimally invasive surgical technique. It is a feasible and safe technique with an excellent outcome.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Visualized Surgery for the series “Teaching Uniportal VATS”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.03.18). The series “Teaching Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. DGR served as the unpaid Guest Editor of the series and serves as an unpaid associate editor-in-chief of Journal of Visualized Surgery. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu CY, Lin CS, Shih CH, et al. Single-port video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Aragón J, Pérez Méndez I. From open surgery to uniportal VATS: asturias experience. J Thorac Dis 2014;6:S644-9. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Hajjar WM, AlSalman BH, AlNajashi NS, et al. The stages of the thoracoscopic right upper lobectomy with complete mediastinal lymph nodes dissection. Asvide 2019;6:099. Available online: http://www.asvide.com/article/view/30985
- Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013;5:S221-5. [PubMed]
- Shen Y, Liu Y, Feng M, et al. Uniportal video-assisted thoracoscopic lobectomy: Zhongshan experience. J Vis Surg 2015;1:5. [PubMed]
Cite this article as: Hajjar WM, AlSalman BH, AlNajashi NS, Hajjar AW, Al-Nassar SA, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic lobectomy surgery for lung cancer—case report. J Vis Surg 2019;5:36.