Nodule marking strategies: cost-benefit
Introduction
The improvement of imaging tests, as well as the advent of lung cancer screening programs (1) have made solitary pulmonary nodules an increasing clinical problem (2).
During investigation some nodules may need tissue sample. However, depending on their size or location, noninvasive diagnostic procedures may not be useful. In this cases, excisional surgical biopsy may be the most appropriate method (2,3).
Video-assisted thoracoscopic surgery (VATS) wedge resection is a well-tolerated minimally invasive procedure. Nevertheless, non-visible or impalpable lesions require an intraoperative localization technique, since they are a limitation for VATS.
Some techniques have been used: intraoperative ultrasonography, hook wire, radiolabeled aggregates, microcoils, liquid agents and navigational bronchoscopy (3). In Brazil, many of these techniques are not available because incorporation of new technologies by health services presents important obstacles.
CT-guided percutaneous barium marking is a simple and low-cost procedure, but is poorly reported in the medical literature (4).
In this article, we describe our experience after standardizing this method in our institution.
Marking techniques
The difficulty of resources in the Brazilian health system restrict our choices.
In Brazil there are two realities: public health system and private health insurances. In the field of public health, the greatest obstacle is the scarce budget. On the other hand, in the private sphere the impediment is the authorizations. In this way, the incorporation of new technologies is a complex issue and hinders our daily practice.
The choice of marking technique should take into account: cost, availability and handling.
Intraoperative ultrasonography and navigational bronchoscopy are expensive technologies that are not part of our reality.
Usually we have 4 methods available: hook wire, radiolabeled aggregates, microcoils and liquid agents (Table 1).
Table 1
| Available marking techniques | Cost | Availability | Handling |
|---|---|---|---|
| Hook wire | High | Limited | Easy |
| Technetium-99 | Low | Unlimited | Tricky |
| Microcoils | High | Limited | Easy |
| Barium | Low | Unlimited | Easy |
| Methylene blue dye | Low | Unlimited | Tricky |
Hook wire is a good technique. It is easy to handle intraoperatively, despite wire dislodgement in up to 10% of cases (3). However, the high cost of the device limits its use.
Technetium-99 is the preferred radiolabeled aggregate (5). It is an easy, available and low-cost method, but it fails as it does not visualize the marking. Gamma probe assess the auditory input adjacent the lesion. In this way, it is an auditory rather than a visual method.
The pros and cons of microcoils resemble those of the hook wire except for the fact that they do not dislodge.
The use of liquid agents has proved to be an important low-cost strategy. Methylene blue dye injection is well reported in the literature. However, we must consider the rapid dye diffusion, which turns the procedure inefficient a few times. On the other hand, barium is inert in lung parenchyma.
Regardless of barium suspension being a low-cost procedure, widely available and easy to handle its use is poorly reported (4). As well as its efficacy, its side effects and complications have not been sufficiently studied.
Our experience
Taking into account the resources available in our environment and their respective effectiveness, we decided to reproduce the barium marking technique (4).
Between January 2013 and May 2018, 41 patients were submitted to the procedure.
All nodules (100%) were adequately located in the intraoperative period. In only 1 case (2.44%) wedge resection was not feasible and a VATS lobectomy was necessary to remove the lesion in its entirety. The marking helped in the location but in the end, it was not effective, because the anatomy was not favorable.
Two patients (4.88%) had complications. One patient complained of cough and another presented with moderate pneumothorax which has not required chest tube.
Patient selection and workup
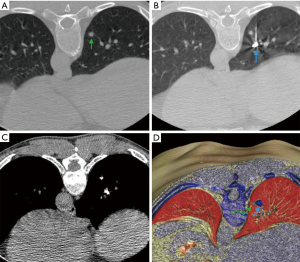
In our service, we use barium marking in patients with presumed impalpable lung nodules which need excisional surgical biopsy (3,6). Our criteria are (Figure 1):
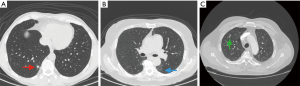
- Lesions less than 1 cm in diameter;
- Subsolid lesions;
- Lesions with a distance greater than 1 cm from the visceral pleura.
All cases are discussed in a multidisciplinary team (pulmonologists, oncologists, thoracic surgeons, radiologists and pathologists).
Pre-operative preparation
- About 4 hours before the surgery patient perform a CT scan;
- Patient are submitted to local anesthesia and CT scan guided percutaneous barium marking;
- Through a 21-gauge Chiba needle 0.2 mL of 140% barium sulfate is injected adjacent to the nodule;
- Control CT scan is done after the puncture to confirm the adequate marking and exclude complications (Figure 2).
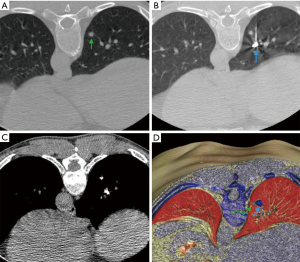 Figure 2 Pre-operative CT-guided barium marking. (A) Small lung nodule in the right lower lobe (green arrow); (B) barium suspension marking (blue arrow) through a 21-gauge Chiba needle; (C) CT (mediastinal window) showing the marking; (D) barium (blue arrow) injected adjacent to the lesion (green arrow).
Figure 2 Pre-operative CT-guided barium marking. (A) Small lung nodule in the right lower lobe (green arrow); (B) barium suspension marking (blue arrow) through a 21-gauge Chiba needle; (C) CT (mediastinal window) showing the marking; (D) barium (blue arrow) injected adjacent to the lesion (green arrow).
Equipment preference card
- Video equipment;
- 30° 10-mm laparoscope;
- 10-mm thoracic port;
- Thoracoscopic grasping clamp;
- Fluoroscopic C-arm;
- Endoscopic stapler;
- Staple cartridge (45 mm-3.5 mm);
- Small wound retractor (2.5–6 cm);
- Specimen retrieval bag.
Procedure
- General anesthesia;
- Selective ventilation;
- Lateral decubitus;
- Intercostal block with ropivacaine 0.75%;
- 10-mm camera port is placed at 8th intercostal space in the anterior axillary line;
- 5-cm long utility incision at 5th intercostal space in the axillary line which will be exposed and protected with wound retractor;
- We approach the pulmonary segment according to the imaging tests. At the first moment, we try indirect palpation of the lesion through a thoracoscopic grasping clamp, as well as the visualization of barium in the pleural surface;
- After deciding the segment, the grasping clamp is positioned simulating the presumed staple line;
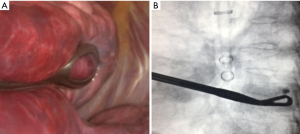
- Intraoperative fluoroscopy reveals if the lesion was correctly located through the marking. This must be in halfway between pleura and the grasping clamp to guarantee complete excision of the nodule (Figure 3);
- If there is doubt that the lesion is in halfway between the grasping clamp and visceral pleura, we can perform transversal rotation movements with the instrument in order to certify adequate positioning. We refer to this as “Barbecue Maneuver” (Figure 4);
 Figure 4 “Barbecue Maneuver”—grasping clamp transversal rotation movements in order to certify adequate positioning (7). Available online: http://www.asvide.com/article/view/27869
Figure 4 “Barbecue Maneuver”—grasping clamp transversal rotation movements in order to certify adequate positioning (7). Available online: http://www.asvide.com/article/view/27869 - The grasping clamp is removed and replaced by the endoscopic stapler;
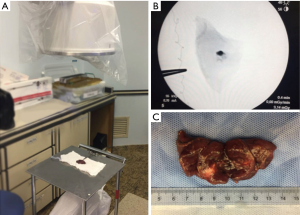
- A wedge resection is performed (Figure 5);
 Figure 5 Wedge resection with intraoperative fluoroscopy (8). Available online: http://www.asvide.com/article/view/27870
Figure 5 Wedge resection with intraoperative fluoroscopy (8). Available online: http://www.asvide.com/article/view/27870 - The specimen is submitted to fluoroscopy. If all the barium marking is in the specimen the excision was satisfactory (Figure 6);
- Frozen section may be performed if intraoperative diagnosis of malignancy demands a major resection;
- 22–24 F chest tube inserted in the camera port.
Role of team members
- Surgeon coordinates and perform the main procedure;
- The 1st assistant handles the camera;
- Surgical instrument technician prepares the surgical instruments and attend surgeon’s requests.
Post-operative management
- Analgesia;
- Early diet reintroduction;
- Early mobilization;
- Control X-ray;
- Chest tube removal if lung fully expanded, absence of air leak and less than 300 mL daily pleural output (9);
- Early hospital discharge.
Tips, tricks and pitfalls
- Discuss all the details of the appointment with the radiologist. Inappropriate marking can lead us away from the injury;
- Fluoroscopy of operative field can help if barium marking complete resection is doubtful;
- In specimen fluoroscopy it is important that there is a space between the staple line and marking. This space can be a first guarantee of safe surgical margin if the marking has been adequate;
- Surgical team must use lead aprons.
Conclusions
Nodules of difficult intraoperative localization will be increasingly frequent. Many marking techniques have been described and new technologies are coming. The choice must be rational taking into account the resources and local reality. In our experience, barium suspension injection proved to be safe, efficient, inexpensive and easy to perform.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ricardo M. Terra and Paula A. Ugalde) for the series “Minimally Invasive Surgery - Robotics and VATS in Brazil” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.10.06). The series “Minimally Invasive Surgery - Robotics and VATS in Brazil” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Keating J, Singhal S. Novel Methods of Intraoperative Localization and Margin Assessment of Pulmonary Nodules. Semin Thorac Cardiovasc Surg 2016;28:127-36. [Crossref] [PubMed]
- Kidane B, Yasufuku K. Advances in Image-Guided Thoracic Surgery. Thorac Surg Clin 2016;26:129-38. [Crossref] [PubMed]
- Lee NK, Park CM, Kang CH, et al. CT-guided percutaneous transthoracic localization of pulmonary nodules prior to video-assisted thoracoscopic surgery using barium suspension. Korean J Radiol 2012;13:694-701. [Crossref] [PubMed]
- Galetta D, Bellomi M, Grana C, et al. Radio-Guided Localization and Resection of Small or Ill-Defined Pulmonary Lesions. Ann Thorac Surg 2015;100:1175-80. [Crossref] [PubMed]
- Bommart S, Bourdin A, Marin G, et al. Impact of preoperative marking coils on surgical and pathologic management of impalpable lung nodules. Ann Thorac Surg 2014;97:414-8. [Crossref] [PubMed]
- Martins FK, Oliveira GA, da Silva TK, et al. “Barbecue Maneuver”—grasping clamp transversal rotation movements in order to certify adequate positioning. Asvide 2018;5:816. Available online: http://www.asvide.com/article/view/27869
- Martins FK, Oliveira GA, da Silva TK, et al. Wedge resection with intraoperative fluoroscopy. Asvide 2018;5:817. Available online: http://www.asvide.com/article/view/27870
- Novoa NM, Jiménez MF, Varela G. When to Remove a Chest Tube. Thorac Surg Clin 2017;27:41-6. [Crossref] [PubMed]
Cite this article as: Martins FK, Oliveira GA, da Silva TKB, Bello RM, Coelho JC, Gelatti A, Lewgoy J, Pasa MB. Nodule marking strategies: cost-benefit. J Vis Surg 2018;4:220.