
Single-incision laparoscopic parastomal hernia repair employing fascial defect closure and sandwich technique
Introduction
Parastomal hernia (PSH) is a common and frequent complication following permanent stoma creation and is currently a distressing issue for patients (1). The surgical approaches for PSH include local repair by suture, relocation, and mesh-based techniques. The keyhole technique and the Sugarbaker technique were launched as laparoscopic surgeries spread among various diseases (2,3). However, these procedures could not reduce the recurrence rate of PSH dramatically; therefore, the sandwich technique was invented to reduce the recurrence rate with acceptable morbidity (4,5).
On the other hand, laparoscopic intraperitoneal onlay mesh (IPOM) repair along with fascial defect closure, also referred to as IPOM-Plus, is often performed for patients with a ventral or incisional hernia (6). The surgical outcomes of IPOM-Plus seemed to be favorable including recurrence rate and incidence of postoperative complications (7).
Conventional laparoscopic PSH repair usually requires 3 to 5 ports. To minimize the wound and abdominal-wall damage, single-incision laparoscopic surgery (SILS) was developed for use in various abdominal surgeries (8). Potential benefits of SILS include better cosmesis, mesh introduction into the abdominal cavity, patient satisfaction, less post-operative pain, and quicker recovery (8).
From these backgrounds, we hereby present the first case of a patient undergoing single-incision laparoscopic PSH repair employing IPOM-Plus and the sandwich technique.
Patient demographics
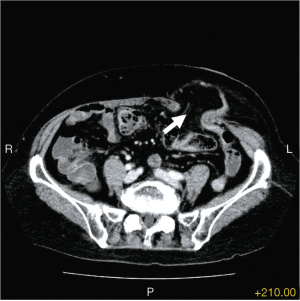
The patient was a 76-year-old woman who received laparoscopic abdominoperineal resection one year ago for treatment of advanced rectal cancer. She sequentially received adjuvant chemotherapy for 6 months including follow-ups at our clinic. However, she noticed the reducible non-tender mass around the sigmoid colostomy about two months ago. A contrast computed tomography (CT) revealed a PSH 5 cm in size as well as an omentum entering the hernia orifice (Figure 1). She agreed to undergo laparoscopic PSH repair.
Pre-operative preparation
Contrast CT is necessary for clarifying the detailed location and diameter of the PSH for planning laparoscopic PSH repair. A barium enema examination from stoma is also useful to confirm the length of the remnant colon. From these results, we usually decide to perform laparoscopic PSH repair. Neither mechanical nor antibiotic bowel preparation is required for this operation.
Equipment and consumables
Here is a list of all equipment and consumables used during the procedure: high definition laparoscopic video system (VISERA ELITE, Olympus®, Tokyo, Japan), 5-mm flexible laparoscope (ENDOEYE FLEX, Olympus®, Tokyo, Japan), routine laparoscopic instruments including atraumatic graspers, scissors, and needle holder, laparosonic coagulating shears (HARMONIC ACE® +7, Ethicon, Tokyo, Japan), 2-0 polypropylene thread (PROLENE®, Ethicon, Tokyo, Japan), 15 cm × 15 cm keyhole type parastomal mesh (PARIETEXTM, Medtronic Japan, Tokyo, Japan), 15 cm × 15 cm Sugarbaker type parastomal mesh (PARIETEXTM, Medtronic Japan, Tokyo, Japan), and mesh fixation device (AbsorbaTackTM, Medtronic Japan, Tokyo, Japan).
Procedure
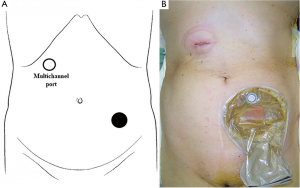
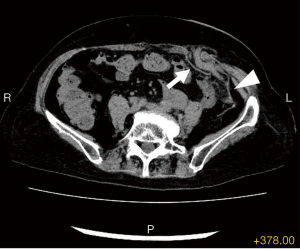
The patient was placed in supine position after the induction of general anesthesia. A multichannel port was placed at the right hypochondriac region (Figure 2), because most of the permanent colostomy was located at the left hypogastric region. Pneumoperitoneum was implemented at a pressure of 6–10 mmHg, and hernia content was extracted from the PSH. Laparoscopic adhesiolysis between the remnant descending colon and the retroperitoneum was performed with preservation of both the ureter and gonadal vessels, and we performed fascial defect closure by intracorporeal suturing using 2-0 PROLENE® (Figure 3). Then, the keyhole type parastomal mesh was introduced into the abdominal cavity and placed around the colostomy, fixed by AbsorbaTackTM (Figure 4). Next, the remnant descending colon was sewn onto the keyhole mesh for the purpose of immobilizing the remnant descending colon. For the final Sugarbaker procedure, Sugarbaker type parastomal mesh was implanted for PSH, which contains a coated portion in the area of the lateralized intestinal portion to prevent mesh migration (Figure 5). Mesh fixation was also carried out by AbsorbaTackTM using the double-crown technique. The total operating time was 132 minutes, and the total blood loss was 3 mL.



Post-operative management
The patient resumed a liquid diet 6 hours after operation and restarted her usual diet on the post-operative day 1; she was discharged from the hospital on the post-operative day 3. Follow-up CT revealed that the meshes appropriately covered the PSH without recurrence (Figure 6).
Tips, tricks, and pitfalls
- Pre-operative contrast CT scan and barium enema examination is required to make operative strategies. These examinations provide us with important information, such as the location and diameter of the PSH, hernia content and intra-abdominal adhesion, coexistence of other incisional hernias, the length of the remnant colon, etc.
- Tacking to the nearest edge of the mesh is sometimes difficult due to the arrangement of the port-site being too near the PSH; therefore, a multichannel port should be placed at the farthest possible location from the PSH.
- During laparoscopic adhesiolysis between the remnant descending colon and the retroperitoneum, we have to pay attention to the location of the ureter and gonadal vessels. We should also certainly avoid damaging any mesenteric vessels.
- Fascial defect closure, also referred to as IPOM-Plus, should be performed by using a non-absorbable thick thread to prevent the dehiscence of the hernia orifice. An interrupted suture is better than a running suture for the same reason. The pneumoperitoneum pressure should be decreased to 6 mmHg to relieve the tension of the abdominal wall when we tie the knots of the IPOM-Plus.
- The most important phase of the keyhole technique is closing the slit of the mesh; the most efficient type of closure should not be too tight or too loose. When we close the slit of the mesh, we first close the inner part of the slit because we have to adjust the tightening of the keyhole.
- Immobility of the remnant descending colon makes it much easier to perform the Sugarbaker technique. We employed intracorporeal suturing between the descending colon and the keyhole mesh or abdominal wall; however, any additional techniques, such as temporal hanging, are also useful depending on the preference of the surgeon.
- Mesh fixation is usually performed in a double-crown technique when performing laparoscopic ventral hernia repairs. However, there are a couple possibilities for concern that arise when performing the sandwich technique. One concern is the duplication of tackers, and another is the thickness of the meshes due to an overlapping technique; moreover, we are not required to persist in performing the double-crown technique.
- We have some concerns about migrations and adhesion between the mesh and the intestine, including the remnant descending colon; therefore, warping or bending of meshes should be appropriately expanded and altered by additional sutures.
Discussion
The occurrence of PSH is a common and unavoidable complication following stoma creation (1). In addition, factors such as obesity, diabetes mellitus, chronic obstructive pulmonary disease, old age, steroid use, and malnutrition play a large role in the development of PSH (12). However, laparoscopic approach has been applied to the repair of PSH, considering that it is minimally invasive and may possibly allow for a more precise repair due to its allowance of a better view of the abdominal wall.
As for the application of the IPOM-Plus technique, the surgical outcomes for ventral or incisional hernias seemed to be favorable, including recurrence rate. Suwa et al. reported that the overall recurrence rate of IPOM-Plus was 0–7.7% with a median follow-up period of 10.5–50.4 months (7). From these backgrounds, employing IPOM-Plus technique for laparoscopic PSH repair has not been routinely performed. Wiessner et al. have recently reported the employment of IPOM-Plus in laparoscopic PSH repair via multiple port approach (13).
Currently, the most cited laparoscopic PSH repairs are the keyhole and Sugarbaker techniques. Berger et al. initially described his experience with the sandwich technique, consisting of a combination of the keyhole and Sugarbaker techniques (4,5). The sandwich technique dramatically reduced the recurrence rate of PSH with acceptable morbidity; therefore, guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society) claims that the sandwich technique can be considered a safe alternative to either the keyhole or Sugarbaker technique (14). However, the sandwich technique costs twice as much as the keyhole or Sugarbaker technique. Given these current circumstances, further investigation regarding long-term recurrence rate and economic benefit of required medical supplies are warranted to prove the true superiority of the sandwich technique over others.
We usually employ the SILS approach in various surgeries, and the usual resulting benefits of SILS are fewer scars, less abdominal wall damage, and greater cosmetic satisfaction (8). However, the SILS procedure is not a naturally ergonomic technique because the traditional laparoscopic principle of triangulation is lost; therefore, SILS requires a longer operative time compared to the conventional laparoscopic procedure (8). In laparoscopic PSH repair, the SILS approach has the advantage of introducing the meshes into the abdominal cavity more easily than the conventional laparoscopic approach because meshes for PSH repairs are too large to introduce from a 12-mm trocar.
In conclusion, we have presented a first-case patient who underwent single-incision laparoscopic PSH repair through employment of IPOM-Plus and the sandwich technique. For various types of ventral hernia, employing the IPOM-Plus technique may potentially reduce recurrence rate (7). In addition, the sandwich technique has been proven to reduce the recurrence rate of PSH (4,5). Currently, the laparoscopic sandwich technique coupled with IPOM-Plus is the best conceivable combination for laparoscopic PSH repair, promising the lowest recurrence rate (14). Furthermore, SILS approach reduces operation-related scars and abdominal muscle damage without affecting the safety or quality of the operation; nevertheless, operating time does tend to be longer. We believe this procedure provides a promising outcome for patients suffering from PSH; therefore, more research is necessary in order to thoroughly assess the efficacy and feasibility of this procedure.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hotouras A, Murphy J, Thaha M, et al. The persistent challenge of parastomal herniation: a review of the literature and future developments. Colorectal Dis 2013;15:e202-14. [Crossref] [PubMed]
- Hansson BM, de Hingh IH, Bleichrodt RP. Laparoscopic parastomal hernia repair is feasible and safe: early results of a prospective clinical study including 55 consecutive patients. Surg Endosc 2007;21:989-93. [Crossref] [PubMed]
- Sugarbaker PH. Peritoneal approach to prosthetic mesh repair of paraostomy hernias. Ann Surg 1985;201:344-6. [Crossref] [PubMed]
- Berger D, Bientzle M. Laparoscopic repair of parastomal hernias: a single surgeon's experience in 66 patients. Dis Colon Rectum 2007;50:1668-73. [Crossref] [PubMed]
- Berger D, Bientzle M. Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair! A prospective, observational study with 344 patients. Hernia 2009;13:167-72. [Crossref] [PubMed]
- Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc 2014;28:2-29. [Crossref] [PubMed]
- Suwa K, Okamoto T, Yanaga K. Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today 2016;46:764-73. [Crossref] [PubMed]
- Umemura A, Suto T, Nakamura S, et al. Comparison of Single-Incision Laparoscopic Cholecystectomy versus Needlescopic Cholecystectomy: A Single Institutional Randomized Clinical Trial. Dig Surg 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Umemura A, Suto T, Fujuwara H, et al. Procedure of IPOM-Plus technique is shown. Asvide 2018;5:770. Available online: http://www.asvide.com/article/view/27356
- Umemura A, Suto T, Fujuwara H, et al. The keyhole technique was performed via SILS approach. Asvide 2018;5:771. Available online: http://www.asvide.com/article/view/27357
- Umemura A, Suto T, Fujuwara H, et al. The Sugarbaker technique was also performed via SILS approach. Asvide 2018;5:772. Available online: http://www.asvide.com/article/view/27358
- DeAsis FJ, Lapin B, Gitelis ME, et al. Current state of laparoscopic parastomal hernia repair: A meta-analysis. World J Gastroenterol 2015;21:8670-7. [Crossref] [PubMed]
- Wiessner R, Vorwerk T, Gehring A. Laparoscopic repair for parastomal hernia with ongoing barbed suture followed by sandwich-technique: 'Sandwich-plus-technique'. J Minim Access Surg. 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])-Part III. Surg Endosc 2014;28:380-404. [Crossref] [PubMed]
Cite this article as: Umemura A, Suto T, Fujuwara H, Nakamura S, Nitta H, Takahara T, Hasegawa Y, Sasaki A. Single-incision laparoscopic parastomal hernia repair employing fascial defect closure and sandwich technique. J Vis Surg 2018;4:202.


