
Distal sternectomy for post-sternotomy chronic osteomyelitis
Introduction
Sternal chronic osteomyelitis following median sternotomy is a severe complication of open cardiac surgery, presenting as purulent draining sinus tracts in patients with a closed sternal wound (1). Its incidence ranges from 1% to 5% but its mortality rate may rise up to 80%, depending on the severity of the infection (2). Fistulas may occur usually after some weeks, months or even years following sternotomy and this is one of the reasons that underestimate their real incidence (3). First-line treatments are repeated curettages, conservative debridements and aggressive antibiotic therapy; moreover, the application of negative pressure to wound can accelerate the wound-healing process and promote granulation tissue formation, by using the vacuum-assisted closure device (VAC) (4).
However, these methods present a high failure rate and the eradication of the infection may require partial or total sternectomy followed by a chest reconstruction and muscle flaps (5). This procedure, however, is associated with a high morbidity and mortality rate; an adequate reconstruction of the sternum and stabilization of the whole chest wall is of paramount importance, in particular when prolonged post-operative mechanical ventilation is needed. Synthetic rigid prosthetic materials are contraindicated because of the infected surgical field and muscular reconstruction can be accomplished by using pectoralis major muscle flaps, rectus abdominis, latissimus dorsi or transposed omentum (6).
Case presentation
A 57-year-old male patient was admitted at our department for a post-sternotomy sterno-cutaneous fistula (Figure 1).
He has been submitted seven months earlier to emergency surgery for cardiac perforation during an epicardial transcatheter ablation of ventricular tachycardia, complicated by multifactorial shock and Staphylococcus Epidermidis sepsis.
Despite surgical toilette, removal of underlying sternal wires, treatment by VAC and appropriate antibiotic therapy, the wound did not show any healing.
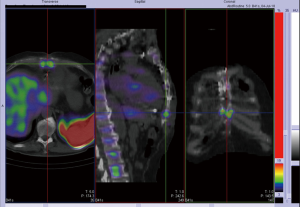
In vitro-labeled leukocyte imaging revealed a chronic osteomyelitis of the distal third of the sternum (Figure 2).
The patient underwent distal sternectomy and resection of all infected costal cartilages for complete eradication of the infection; thoraco-abdominal wall integrity was restored by an absorbable polyglactin mesh (Vicryl meshTM) fixed by absorbable interrupted stitches to the surrounding healthy cartilaginous and soft tissue structures, to prevent laparocele or visceral herniation (Figure 3).

Post-operative course did not disclose any major complications.
Discussion
Post-operative infection of sternal wound significantly increases the morbidity and mortality associated with cardiothoracic surgery (8). Major risk factors for developing deep sternal wound infections are diabetes mellitus, intensive care unit (ICU) stay longer than 5 days, need for re-do sternotomy, higher body mass index and the use of the internal mammary vessels for coronary artery bypass grafts (9). The main tasks for successful treatment of chronic osteomyelitis are removing the infected bone and the steel wires because of the presence of biofilms in the foreign materials as well as an adequate antibiotic therapy; however, recalcitrant infections may require sternectomy and resection of all infected costal cartilages for complete eradication of the infection.
Being performed after one or several previous cardiac procedures, in infected surgical fields with subsequently complex chest wall reconstructions, this type of sternal resection can be technically demanding, often requiring multidisciplinary approach involving cardiac, thoracic and plastic surgeons.
Preoperative sinograms may show communication among cartilaginous-cutaneous tracts or between these tracts and the mediastinum as well as computed tomography (CT) scan may contain information about the location or presence of bypass grafts and prosthetic material; it is extremely important to exactly know the type of procedures received by the patient and previous operative reports may offer useful data. In vitro-labeled leukocyte imaging is the nuclear medicine test of choice for diagnosing complicating osteomyelitis. Leukocytes accumulate in bone marrow as well as in infection. Performing complementary bone marrow imaging with 99mTc-sulfur colloid facilitates the differentiation between osteomyelitis and normal marrow and improves test overall accuracy (10). Reconstruction techniques after total or partial sternectomy for osteomyelitis have been described since the early 1970s and 1980s like transposing pedicled omentum to the mediastinum, pectoralis major rotation flaps and pectoralis myocutaneous advancement flaps (6).
As our patients was previously submitted to median laparotomy with initial laparocele, after distal sternectomy we fixed an absorbable polyglactin mesh (Vicryl meshTM) by absorbable interrupted stitches to the surrounding healthy cartilaginous and soft tissue structures, to prevent laparocele or visceral herniation. We avoided rigid non-absorbable prostheses because of the infected field and to avoid significant limitation of thoraco-abdominal flexion.
In conclusion, distal sternectomy may be advocated as rescue treatment for post sternotomy recalcitrant osteomyelitis; if needed, absorbable soft mesh can be considered for thoraco-abdominal reconstruction and stabilization.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.09.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tocco MP, Ballardini M, Masala M, et al. Post-sternotomy chronic osteomyelitis: is sternal resection always necessary?. Eur J Cardiothorac Surg 2013;43:715-21. [Crossref] [PubMed]
- Ottino G, De Paulis R, Pansini S, et al. Major sternal wound infection after open-heart surgery: a multivariate analysis of risk factors in 2,579 consecutive operative procedures. Ann Thorac Surg 1987;44:173-9. [Crossref] [PubMed]
- Steingrímsson S, Gustafsson R, Gudbjartsson T, et al. Sternocutaneous fistulas after cardiac surgery: incidence and late outcome during a ten-year follow-up. Ann Thorac Surg 2009;88:1910-5. [Crossref] [PubMed]
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg 1997;38:563-76; discussion 577. [Crossref] [PubMed]
- El Oakley RM, Wright JE. Postoperative mediastinitis: classification and management. Ann Thorac Surg 1996;61:1030-6. [Crossref] [PubMed]
- Johnson P, Frederiksen JW, Sanders JH, et al. Management of chronic sternal osteomyelitis. Ann Thorac Surg 1985;40:69-72. [Crossref] [PubMed]
- Petrella F, Arlati F, Mariolo AV, et al. Distal sternectomy for post-sternotomy chronic osteomyelitis. Asvide 2018;5:745. Available online: http://www.asvide.com/article/view/27130
- Scholl L, Chang E, Reitz B, et al. Sternal osteomyelitis: use of vacuum-assisted closure device as an adjunct to definitive closure with sternectomy and muscle flap reconstruction. J Card Surg 2004;19:453-61. [Crossref] [PubMed]
- Gummert JF, Barten MJ, Hans C, et al. Mediastinitis and cardiac surgery--an updated risk factor analysis in 10,373 consecutive adult patients. Thorac Cardiovasc Surg 2002;50:87-91. [Crossref] [PubMed]
- Palestro CJ. Radionuclide imaging of osteomyelitis. Semin Nucl Med 2015;45:32-46. [Crossref] [PubMed]
Cite this article as: Petrella F, Arlati F, Mariolo AV, Gennari M, Pirola S, Polvani G, Spaggiari L. Distal sternectomy for post-sternotomy chronic osteomyelitis. J Vis Surg 2018;4:195.



