Refined running suture lower body lift in massive weight loss patients
Introduction
In the past four decades obesity has steadily increased to the extent where more people are obese than underweight in the world (1). The lower body lift is a recognized procedure for the treatment of skin surplus and laxity of Massive Weight Loss (MWL) patients. The circumferential body contouring procedure “belt lipectomy”, was first described by Gonzalez-Ulloa M in 1960 (2) and has since then been modified and improved by several authors (3-7). The procedure is described to be time-consuming, often lasting several hours, and the rate of surgical complications in this patient group is generally high (8,9). With increasing amount of surgical procedures performed and the pressure on cost savings, improvements are being made by surgeons everywhere. We have made some adjustments that have proven to be beneficial to our practice and this study was designed to test the impacts of three different surgical setups for lower body lift with operative time as the primary outcome measure.
Methods
This retrospective study included MWL patients undergoing a circumferential lower body lift procedure including a fleur-de-lis abdominoplasty at Mølholm Private Hospital, Vejle, Denmark in the period February 17th 2015–June 21th 2016. All patients were referred from a public hospital with officially indications for surgery due to skin problems after MWL; a weight loss of more than 15 BMI units and a BMI of less than 30 kg/m2 at the time of surgery and physical problems due to excess skin and fat.
Demographic data, weight loss method, co-morbidity and postoperative complications were registered. The number of consultant plastic surgeons performing the procedure, the suture technique used and the total operative time were also registered.
The same two consultant plastic surgeons operated on all dual-led lower body lifts, and a total of four experienced consultant plastic surgeons performed the single-led lower body lifts. In the one surgeon setting, an experienced scrub nurse also performed suturing.
Excluded from the study, were patients having a lower body lift combined with liposuction and patients having a lower body lift without fleur-de-lis.
Written and oral consent were obtained from all patients in accordance to guidelines from the Danish Patient Safety Authority.
Statistical analysis
Descriptive statistics were calculated using Excel for Mac 2011. Student’s t-test was used to analyse the differences in time for surgery. Data followed a normal distribution and data are presented as means ± SD. A P value of less than 0.05 was considered statistically significant.
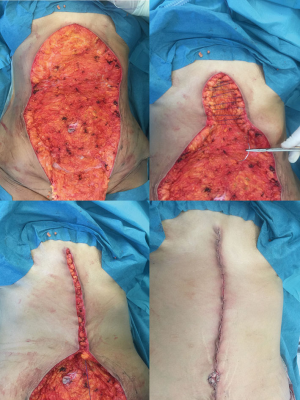
Surgical technique: running suture (Figure 1)
The patient was marked in the standing position prior to surgery. The anterior markings include a vertical and a horizontal excision pattern.
Surgery was commenced with the patient in the prone position. Skin and fat was excised using monopolar cautery down to the level of Scarpa’s fascia.
The defect was sutured in three layers, all in a running fashion using a PDS®0 loop suture, polyglactin (vicryl®) 2-0 and poliglecaprone (monocryl®) 3-0 (Figure 2). The patient was then turned to a supine position and a vertical abdominoplasty with a fleur-de-lis resection pattern was performed, also to the level of Scarpa’s fascia. Again the defect was closed using a PDS®-0 loop suture, polyglactin (vicryl®) 2-0 and poliglecaprone (monocryl®) 3-0.
The umbilicus was sutured using a polyglactin (vicryl®) 3-0 and a nylon (ethilon®) 4-0 suture. Two drains were placed on the abdomen and none at the back or flanks.
Surgical technique: interrupted suture
The technique is identical to the running suture technique with the exception of the two deep layers that were closed by interrupted polyglactin (vicryl®) 2-0 and polyglactin (vicryl®) 3-0 followed by a running poliglecaprone (monocryl®) skin suture.
Drains were removed when the production was less than 50 mL per day. A compression garment was used both day and night for six weeks. All patients were controlled in the outpatient clinic after 14 days and again after three months. Preoperative photographs and three months postoperative results are shown in Figures 3 and 4.
Results
We included a total of 59 patients in the study: 46 women and 13 males. The mean age was 42 (SD =8.9) years. The mean BMI at time of surgery was 26.3 (SD =2.56) kg/m2. The mean weight loss was 20.4 (SD =4.9) BMI units. The majority, 40 patients, had lost weight following a gastric bypass surgery, two patients had a gastric banding surgery and 17 patients had lost weight by means of changing their diet and exercise (Table 1).
Table 1
| Demographics | Total | 1 surgeon | 2 surgeons, running | |
|---|---|---|---|---|
| Interrupted | Running | |||
| No. patients | 59 | 31 | 6 | 22 |
| Age (y, mean, SD) | 42 (8.9) | 43 (8.5) | 41 (12.3) | 42 (9.0) |
| Sex, n (%) | ||||
| Female patients | 46 (78) | 22 | 5 | 19 |
| Male patients | 13 (22) | 9 | 1 | 3 |
| BMI (kg/m2, mean, SD) | 26.3 (2.56) | 26.2 (2.86) | 26.3 (1.67) | 26.5 (2.39) |
| ÄBMI (kg/m2, mean, SD) | 20.4 (4.9) | 21.0 (5.5) | 18.5 (2.8) | 20.0 (4.5) |
| Smoking, n | 3 | 2 | 0 | 1 |
| Diabetes, n | 0 | 0 | 0 | 0 |
| Hypertension, n | 6 | 2 | 1 | 3 |
| Reason for MWL, n (%) | ||||
| Gastric bypass | 40 (68) | 20 | 3 | 17 |
| Gastric banding | 2 (3) | 0 | 0 | 2 |
| Diet and exercise | 17 (29) | 11 | 3 | 3 |
The mean operative time was 148 (SD =56) minutes for all 59 patients. Thirty-one patients were operated by one surgeon using an interrupted suture technique at a mean operative time of 195 (SD =28) minutes, and six patients by one surgeon using the running suture technique at a mean operative time of 131 (SD =36) minutes (P<0.0001). Twenty-two patients were operated on by the dual led team of two surgeons using the running suture technique at a mean operative time of 88 (SD =13) minutes (P<0.0001). All included patients had a hospital stay of only one day and the average drain duration was 1 (range: 1–3) days.
Two patients (3%) were re-operated due to a hematoma within 24 hours, one in the two surgeon running suture group and one in the one-surgeon running suture group.
The most common complications in the one surgeon group were wound dehiscence and superficial skin infection (Table 2). Some patients experienced more than one minor complication at the same time. Only oral antibiotics were prescribed. In the two surgeon running suture group, a total of six superficial infections, four wound dehiscences and one minor haematoma not requiring surgery were seen in six patients (27%).
Table 2
| Variables | Total n=59 | 1 surgeon | 2 surgeons, running (n=22) | |
|---|---|---|---|---|
| Interrupted (n=31) | Running (n=6) | |||
| Operative time, minutes, mean [SD] | 148 [56] | 195 [28] | 131 [36], P<0.0001 | 88 [13], P<0.0001 |
| Tissue removed, g, mean [SD] | 2,234 [955] | 2,123 [746] | 1,773 [860] | 2,516 [1,176] |
| Drainage, days, mean [range] | 1 [1–3] | 1 [1–3] | 1 [1–3] | 1 [1] |
| Hospitalization, mean | 1 | 1 | 1 | 1 |
| Complications (%) | 18 (31) | 9 | 2 | 7 |
| Major (%) | ||||
| Bleeding | 2 (3) | 0 | 1 | 1 |
| Minor (%) | 16 (27) | 9 | 1 | 6 |
| Infection | 12 | 5 | 1 | 6 |
| Wound dehiscence | 11 | 7 | 4 | |
| Minor hematoma | 1 | 1 | ||
Discussion
The lower body lift procedure is considered time consuming due to the large extent of dissection and wound area requiring substantial amount of suturing. The reported total operative time is most often several hours, ranging from 3–6 hours and even longer in the past (3,6,9,11-14) (Table 3). In this study, we present a technique and a setup that reduces the total operative time significantly. A dual-consultant (15) setup using a running suture technique was considerably faster compared to the standard approach with one surgeon using an interrupted suture technique. Comparison of the single-surgeon interrupted suture approach to a single-surgeon running suture technique, the total operative time was reduced, on average by 64 minutes; from 195 to 131 minutes. Adding another surgeon, the procedure was reduced even further to on average 88 minutes (Table 2).
Table 3
| Source | No. surgeons | Duration | Drain duration | Hospital stay |
|---|---|---|---|---|
| Ikander |
Two | 88±13.7 min | 1 day | 1 day |
| Bertheuil |
n/a | 3.8 [2.5–4.7] hours | 3.6 [3–5] days | 3.5 [2–5] days |
| Modarressi |
n/a | 5.2 [3.2–7.3] hours | n/a | 7 [5–25] days |
| Small |
n/a | 6 hours | 7–10 days | 1–2 days |
| Richter |
Two | n/a | Minimum 4 days | 3–6 days |
| Kitzinger |
n/a | 5.2±0.9 hours | 6.7±2.3 days | 9.9±1.6 days |
| Koller |
n/a | 3.8 hours | n/a | n/a |
| Vico |
One | 4.38±1.15 hours | n/a | 7.4±3.6 days |
| Jones |
n/a | 4.2 [3.25–5] hours | 1 | 3.5 [3–6] days |
| Nemerofsky |
One | 4.20 [2.7–7.5] hours | Maximum 5 weeks | 2 days |
| Strauch |
Two | 3–3.5 hours | n/a | 2 days |
| Wallach [2005] | Two | 5–6 hours | 2–3 weeks | Usually one |
| Van Huizum |
Two | 132 [79–210] minutes | 7 days | 8 days |
| Aly |
Two | 5.75 [4.86–6.93] hours | Up to 2 weeks | 1–4 days |
In our experience, the key to a fast and safe closure with a cosmetic pleasing result is the PDS®0 loop suture placed at the level of Scarpa’s fascia. The suture enables fast suturing. The surgeon is able to place up to 10 stiches prior to tightening the suture as shown in the images (Figure 4). The time for adapting the wound edges of the vertical abdominoplasty as seen in the images takes only a couple of minutes. All the tension is placed at the level of Scarpa, which results in tensionless closure of the dermal layers, thus enabling a cosmetic pleasing result. The changes in terms of surgical technique are subtle, however the effect of this change is substantial regarding operative time. The total operative time mentioned in this study does include the perioperative position change of the patient, from prone to supine position. This procedure only takes a few minutes, since all staff members including the surgeons take part.
It is well known that duration of general anaesthesia is correlated with increased rates of postoperative complications like venous thromboembolism, hypothermia, infection and postoperative nausea and vomiting (16-18). Studies have also shown a clear correlation between operating time and muscular fatigue of the surgeon (19).
The shorter operative time found in this study, can therefore have a positive impact on these factors. The complication rate in this patient group is recognized to be higher in general, compared to non-MWL patients and the complication rate in this study was similar to that of previous studies (8,9,11,20). The majority however, are minor complications i.e. minor wound dehiscence and superficial infections as in this report. We experienced two major complications, both being postoperative bleeding requiring reoperation and both occurred in the running suture group. One bleeding was in the beginning of the study period and one was halfway through. However, due to the described level of dissection, the level of Scarpas fascia, which reduces the amount of “dead space” to a minimum, the haematoma was easily detectable due to its superficial location and was evacuated immediately. Both patients were discharged the following day as planned. All but three patients had their drains removed on the first postoperative day and were subsequently discharged, they were discharged as the others with drains, to have them removed at a short follow up visit.
Interestingly, we have not experienced any problems with seroma and this is reflected by this series. We postulate that this is largely due to the extent and level of dissection at the level of the avascular plane of Scarpas fascia, thus preserving the underlying lymphatic vessels and tissue volume, as previously described (5,14,21). All dissection, both at the back and anteriorly were made at this fascial level. This correlates well with a recently published study on Lipo-Body Lift procedure by Bertheuil et al., where the skin resection is performed just beneath the dermis, after completed liposuction and none of their patients developed a seroma (22). This is believed to be due to the limited disruption of the connective tissue structure.
We did not use and have not used any kind of quilting sutures or fibrin glue application in order to reduce seroma formation although this has been suggest to be of benefit (21,23). However, a recent meta-analysis by Nasr et al., present a lack of high quality evidence to support the use of tissue adhesives to prevent seroma formation after abdominoplasty (24).
When we initiated the continuous running suture technique in all three layers we feared the potential risks of a disastrous wound rupture occurring, with major dehiscence, as it all fell apart. Fortunately in all of the 28 running suture patients no such event occurred. Minor superficial wound dehiscence was seen equally frequent in both groups.
There is to date not a clear consensus regarding the length of hospital stay or days of drainage, and many different approaches have been suggested but not compared (4,9,23,25,26).
We have not found any literature references with comparably short operative time, length of hospital stay and drainage (Table 3). The current study has limitations, one being the retrospective design. Another being the fact that two surgeons who used interrupted sutures were not the same two ones using the running suture technique, thus a difference between surgeons must be anticipated when it comes to general operating speed and skills, however, all four surgeons were consultant plastic surgeons, experienced with the procedure, and the difference ought to be negligible in terms of the difference observed.
Conclusions
The lower body lift procedure in MWL patients has mostly, until now, been a time consuming procedure. We have shown that a setup with a dual-led consultant approach using a running suture technique speed up the mean time for a circumferential lower body lift including a fleur-de-is abdominoplasty to 1.5 hours, still providing good results and normal margin of safety. A shorter operative time has several advantages and with increasing demand for post bariatric procedures, the adaptation of a technique that is faster, yet providing a good cosmetic and functional result, is inevitable. The setup, described in the present study, shortens the operative time, the hospital stay and reduces the extent of drainage while maintaining the good results and safety of its predecessors and can therefore be recommended.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.08.19). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- . Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016;387:1377-96. [Crossref] [PubMed]
- Gonzalez-Ulloa M. Belt lipectomy. Br J Plast Surg 1960;13:179-86. [Crossref] [PubMed]
- Aly AS, Cram AE, Chao M, et al. Belt lipectomy for circumferential truncal excess: the University of Iowa experience. Plast Reconstr Surg 2003;111:398-413. [Crossref] [PubMed]
- Richter DF, Stoff A. Circumferential body contouring: the lower body lift. Clin Plast Surg 2014;41:775-88. [Crossref] [PubMed]
- Lockwood T. Lower body lift with superficial fascial system suspension. Plast Reconstr Surg 1993;92:1112-22; discussion 1123-5. [Crossref] [PubMed]
- Nemerofsky RB, Oliak DA, Capella JF. Body lift: an account of 200 consecutive cases in the massive weight loss patient. Plast Reconstr Surg 2006;117:414-30. [Crossref] [PubMed]
- Strauch B, Herman C, Rohde C, et al. Mid-body contouring in the post-bariatric surgery patient. Plast Reconstr Surg 2006;117:2200-11. [Crossref] [PubMed]
- Hasanbegovic E, Sorensen JA. Complications following body contouring surgery after massive weight loss: a meta-analysis. J Plast Reconstr Aesthet Surg 2014;67:295-301. [Crossref] [PubMed]
- Kitzinger HB, Cakl T, Wenger R, et al. Prospective study on complications following a lower body lift after massive weight loss. J Plast Reconstr Aesthet Surg 2013;66:231-8. [Crossref] [PubMed]
- Ikander P, Gad D, Gunnarsson GL, et al. Video showing the refined running suture lower body lift in massive weight loss patients. Asvide 2018;5:741. Available online: http://www.asvide.com/article/view/27062
- Vico PG, De Vooght A, Nokerman B. Circumferential body contouring in bariatric and non-bariatric patient. J Plast Reconstr Aesthet Surg 2010;63:814-9. [Crossref] [PubMed]
- Wallach SG. Abdominal contour surgery for the massive weight loss patient: the fleur-de-lis approach. Aesthet Surg J 2005;25:454-65. [Crossref] [PubMed]
- Jones BM, Toft NJ. Body lifting: indications, technique and complications. J Plast Reconstr Aesthet Surg 2008;61:730-5. [Crossref] [PubMed]
- Koller M, Hintringer T. Circumferential superficial fascia lift of the lower trunk: surgical technique and retrospective review of 50 cases. J Plast Reconstr Aesthet Surg 2012;65:433-7. [Crossref] [PubMed]
- Sharma KS, Nanidis T, Lam DG. The benefits of a dual led consultant approach for microsurgical procedures. J Plast Reconstr Aesthet Surg 2014;67:e129-30. [Crossref] [PubMed]
- Mlodinow AS, Khavanin N, Ver Halen JP, et al. Increased anaesthesia duration increases venous thromboembolism risk in plastic surgery: A 6-year analysis of over 19,000 cases using the NSQIP dataset. J Plast Surg Hand Surg 2015;49:191-7. [Crossref] [PubMed]
- Hardy KL, Davis KE, Constantine RS, et al. The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. Aesthet Surg J 2014;34:614-22. [Crossref] [PubMed]
- Phillips BT, Wang ED, Rodman AJ, et al. Anesthesia duration as a marker for surgical complications in office-based plastic surgery. Ann Plast Surg 2012;69:408-11. [Crossref] [PubMed]
- Slack PS, Coulson CJ, Ma X, et al. The effect of operating time on surgeons' muscular fatigue. Ann R Coll Surg Engl 2008;90:651-7. [Crossref] [PubMed]
- van Huizum MA, Roche NA, Hofer SOP. Circular Belt Lipectomy. Ann Plast Surg 2005;54:459-64. [Crossref] [PubMed]
- Seretis K, Goulis D, Demiri EC, et al. Prevention of Seroma Formation Following Abdominoplasty: A Systematic Review and Meta-Analysis. Aesthet Surg J 2017;37:316-23. [Crossref] [PubMed]
- Bertheuil N, Chaput B, De Runz A, et al. The Lipo-Body Lift: A New Circumferential Body-Contouring Technique Useful after Bariatric Surgery. Plast Reconstr Surg 2017;139:38e-49e. [Crossref] [PubMed]
- Modarressi A, Meia Ruegg E, Bezzola T, et al. Circular abdominoplasty after massive weight loss: Is it a risky procedure? J Plast Reconstr Aesthet Surg 2016;69:1497-505. [Crossref] [PubMed]
- Nasr MW, Jabbour SF, Mhawej RI, et al. Effect of Tissue Adhesives on Seroma Incidence After Abdominoplasty: A Systematic Review and Meta-Analysis. Aesthet Surg J 2016;36:450-8. [Crossref] [PubMed]
- Aly A, Mueller M. Circumferential truncal contouring: the belt lipectomy. Clin Plast Surg 2014;41:765-74. [Crossref] [PubMed]
- Small KH, Constantine R, Eaves FF 3rd, et al. Lessons Learned After 15 Years of Circumferential Bodylift Surgery. Aesthet Surg J 2016;36:681-92. [Crossref] [PubMed]
Cite this article as: Ikander P, Gad D, Gunnarsson GL, Boljanovic S, Sørensen JA, Thomsen JB. Refined running suture lower body lift in massive weight loss patients. J Vis Surg 2018;4:194.