
Resection of a large thymoma of 15 cm without thoracotomy nor sternotomy
Introduction
Thymoma is a rare malignancy most often characterized by biological slow growth. Surgical complete resection remains the gold standard allowing excellent long-term survival with reported disease-free survival up to 90% at 10-year depending on stage and WHO classification. Historically, median sternotomy is the preferred approach that provides full exposure and access to surrounding mediastinal structures and pericardial fat which may potentially be involved by the tumour. Video-assisted thoracoscopic surgery (VATS) has evolved in parallel with instrumentation and experience of surgeon with advanced cases for treatment of early non-small cell cancer. Minimal invasive approach is nowadays the preferred approach for small (less than 5 cm), well encapsulated, non-invasive thymoma in experienced centers. However, despite these progresses, there is still no consensus on the optimal approach for thymectomy, particularly on the laterality of the approach (right/left, bilateral, uniportal or subxiphoid). Currently the approach is mainly dictated by the experience of the surgeon and the localization of the thymic lesion. In addition, in case of large tumour, larger access by sternotomy or thoracotomy may be necessary for safe dissection of surrounding major vascular structures and for easier extraction of the specimen at the end of the procedure. We present the case of a patient who underwent bilateral thoracoscopy and subxiphoid extraction of a large 15 cm thymoma without thoracotomy nor sternotomy.
Case presentation
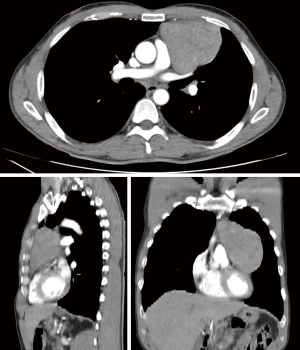
A 51-year-old male was referred with an incidental finding of a large anterior mediastinal mass. Chest CT-scan showed a well encapsulated thymic lesion of 10 cm × 15 cm extending on the left pleural cavity close to the left phrenic nerve without invasion of adjacent structures (Figure 1). The trans-thoracic Tru-Cut biopsy diagnosed an AB thymoma. Due to the size of the lesion and its left location, the decision was taken to start the operation on the right side by thoracoscopy for safe dissection of thyrothymic horns and innominate vein. The patient was positioned in supine position with both arms below the chest and gently separated from the chest wall. The entire sternum was maintained in the operative field to have access in case of urgent conversion to sternotomy. The general anesthesia was managed with a double lumen tube. We used a three-port technique with three trocars (one of 10 mm and two of 5 mm) positioned along the inferior border of the pectoralis muscle. The optic port was located in the midclavicular line in the 5th intercostals space with the carbon dioxide insufflation. The surgeon and the assistant were located on the side of the operative field and the scrub nurse on the opposite side.
The equipment consisted in a thoracoscope 10 mm 30° in order to optimize the visualization of the pleural cavity and the entire mediastinum. We used for dissection classical straight laparoscopic forceps and an energy device for dissection and coagulation (Sonicision; Medtronic®). Succion device was also used for aspiration and blunt dissection. Carbon dioxide was insufflated with continuous flow and a moderate pressure up to 8–10 mmHg.
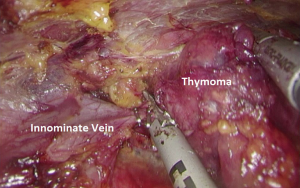
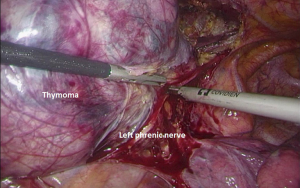
The procedure started on the right side distant to the tumor to first dissect and control the superior horns off the innominate vein. Then the retro-sternal plane was opened and the thymic gland mobilized inferiorly to dissect the superior horns (Figure 2). Tumor was released from the pericardium on the right side. Then, the left thoracoscopy allowed safe dissection of the left phrenic nerve (Figure 3). A subxiphoid incision was added with resection of the xyphoid appendix. The specimen was finally placed in a retrieval bag and removed. Histological examination confirmed the complete resection of 15 cm × 9 cm AB thymoma Masaoka stage I. Postoperative course was uneventful and the patient was discharged on day 2. After 9 months, the patient presented no recurrence and recover normal functional status (Figure 4).

Discussion
During the last decade, mediastinal surgery has benefited from the growing experience in minimally invasive approaches for lung cancer. The potential advantages of VATS over classical sternotomy are numerous including less morbidity, smaller incisions, shorter hospitalization and rapid return to daily activities (2-4). Nevertheless, concerns remained for thymoma, regarding the risk of local dissemination of the tumor due to manipulation and capsular disruption during the dissection. Post-operative outcomes for VATS thymectomy have been reported favorably in comparison with open sternotomy in term of bleeding, length of drainage and hospitalization with comparative long-term oncological results (2). VATS approach is nowadays largely proposed for small (<5 cm) well encapsulated non-invasive thymoma in many experienced centers.
Laterality of the procedure is generally selected based on the location of the thymoma. In our case, we decided to start first by the right approach for safer initial dissection of the thyrothymic horns and innominate vein which was considered risky by left due to the size of the tumour. On the right side, the innominate vein is easy to find as you can follow the vena cava. Once, the tumour was freed from innominate vein and distant of the right phrenic nerve, left approach was continued to finish dissection of the left phrenic nerve which could be preserved. The subxiphoid incision is becoming popular for different thoracic surgical procedures with significant reported decreased post-operative pain in comparison with sternotomy or thoracotomy due to the absence of chest wall paresthesia (5,6). We decided to remove the specimen through this subxiphoid incision of 6cm with concurrent xyphoid appendix resection to enlarge the incision and extract the specimen. Interestingly, post-operative pain was well tolerated by patient.
In conclusion, large non-invasive thymoma can be managed occasionally by bilateral thoracoscopy to control and dissect safely both innominate vein and phrenic nerves. In case of large tumor, surgical specimen can be extracted without thoracotomy nor sternotomy through a small subxiphoid incision.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.08.16). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abdelnour-Berchtold E, Forster C, Perentes JY, et al. Thymectomy by bilateral thoracoscopy and subxiphoid approach. Asvide 2018;5:736. Available online: http://www.asvide.com/article/view/26962
- Ye B, Tantai JC, Ge XX, et al. Surgical techniques for early-stage thymoma: video-assisted thoracoscopic thymectomy versus transsternal thymectomy. J Thorac Cardiovasc Surg 2014;147:1599-603. [Crossref] [PubMed]
- Jurado J, Javidfar J, Newmark A, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg 2012;94:974-81; discussion 981-2. [Crossref] [PubMed]
- Zahid I, Sharif S, Routledge T, et al. Video-assisted thoracoscopic surgery or transsternal thymectomy in the treatment of myasthenia gravis? Interact Cardiovasc Thorac Surg 2011;12:40-6. [Crossref] [PubMed]
- Karunanantham J, Fok M, Ali JM, et al. Subxiphoid single incision thoracoscopic surgery approach for thymectomy: a case report. J Vis Surg 2017;3:147. [Crossref] [PubMed]
- Chen H, Xu G, Zheng W, et al. Video-assisted thoracoscopic extended thymectomy using the subxiphoid approach. J Vis Surg 2016;2:157. [Crossref] [PubMed]
Cite this article as: Abdelnour-Berchtold E, Forster C, Perentes JY, Gonzalez M. Resection of a large thymoma of 15 cm without thoracotomy nor sternotomy. J Vis Surg 2018;4:191.


