
A novel intra-operative navigation system for resection of small lung nodules by video-assisted thoracoscopic surgery (VATS) using three-dimensional image construction in real time and on site with a tablet computer
Introduction
Improved accuracy of imaging modalities, such as computed tomography (CT), is needed for resection of small lung nodules that are otherwise difficult to detect. In such cases, qualitative diagnosis is difficult because of the small size of the tumor; thus, a pathological diagnosis is usually made intraoperatively. If performed appropriately, partial lung resection leads to complete cure of adenocarcinoma in situ and minimally invasive adenocarcinoma. Therefore, in order to ensure an adequate resection margin, it is necessary to accurately identify the tumor site, which is difficult to do during partial lung resection. In addition, identification of the tumor site leads to maximum preservation of the vessels and bronchi in the remaining lung to avoid reduced respiratory function.
While thoracoscopic surgery is advantageous in terms of being less invasive and achieving better cosmesis, several problems, such as the difference between the surgical view and monitor image because of the narrow two-dimension (2D) view of a monitor versus an ordinary 2D-CT image, must be addressed.
Recently, several studies have reported the usefulness of identifying the tumor site using such as virtual-assisted lung mapping (VAL-MAP); however, most methods are often invasive and complicated (1-5). Therefore, a simple intraoperative navigation system that can be accessed in the operating room (OR) is required to reduce the invasiveness of the surgery while maintaining curability.
Here, we describe a novel intraoperative navigation system using a software (Amin Inc., Tokyo, Japan) that can easily obtain an image desired by the surgeon and can be controlled using a tablet computer (TC) (6). We evaluated the utility of the proposed intraoperative navigation system with that of conventional visual inspection and palpation.
Patient selection and workup
In total, 53 patients with suspected malignant tumors underwent partial lung resection via video-assisted thoracoscopic surgery (VATS) between July 2017 and April 2018 at the Department of Surgery, Division of Thoracic Surgery, Jikei University School of Medicine, Tokyo, Japan. Of these 53 patients, three were selected for this study because their tumor position was in the vicinity of the visceral pleura. In addition, 1-mm slice enhanced CT examinations of all three cases were performed for comparison with the virtual images created using the proposed three-dimensional (3D) image system. For all three cases, the American Society of Anesthesiologists physical status was class 1 or 2, which was judged as sufficient for the patients to endure the procedure in accordance with preoperative criteria of our hospital. Ground glass opacity was observed in two cases, whereas a thin-wall cavitary lesion was observed in the third.
Intraoperative imaging of the tumor via thoracoscopy was confirmed by visual inspection and palpation. The monitor angle and direction were traced using the TC, and an appropriate 3D image was created on site by the digital imaging assistant. The image was fed back in real time to the surgeon who was able to easily compare between the monitor and the 3D views. The resected specimen was diagnosed by pathological examination. No tumor cells were observed at the excised end. One case was complicated with prolonged air leakage.
Preoperative preparation
The tumor volume and mass and the lung surface and vessels were created using axial data [Digital Imaging and Communications in Medicine (DICOM)] obtained via 1-mm slice enhanced CT using a workstation dedicated for the creation of 3D images (Ziostation 2; Ziosoft, Inc., Belmont, CA, USA).
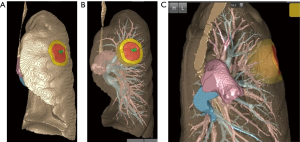
Further, we made two highlighted concentric spheres of 150 and 200 mm from the outer edge of the tumor, respectively. The highlighted concentric spheres between 150 and 200 mm were considered as virtual resection lines (Figure 1).
Because of the high volume, it is difficult to handle data using a general-purpose computer in the OR. The 3D viewing software developed by Amine Inc. recognizes only the shape displayed and does not include the CT value. In addition, the amount of data is compressed from gigabytes to megabytes, which makes data easily controllable and sufficient enough to enlarge, reduce, and/or rotate the 3D image, and delete the volume or render it transparent even on a general-purpose TC. Surgical simulation was performed before surgery, and the image was confirmed by the surgeon, assistant, and digital imaging assistant using the TC. The role of the digital imaging assistant was to operate the TC in the OR.
Equipment preference card and procedure
All surgeries were performed under general anesthesia and differential pulmonary ventilation with the patient in the lateral position. An epidural catheter was inserted for postoperative pain relief. Partial lung resection was performed using a 3-port VATS with a 10-mm 30-degree thoracoscope and a “Forest River” (Midorija Sugiura, Nakano, Tokyo, Japan) instrument invented by Dr. Morikawa.
The digital imaging assistant instantaneously visualized the 3D image as desired by the operator while orally interacting with the surgeon in real time via a Leap Motion® hand gesture tracking system (Leap Motion, Inc., San Francisco, CA, USA) and a telephone headset to enlarge, reduce, rotate, make transparent, or delete the image. The surgeon comprehensively took in to consideration both the image obtained from this system and the thoracoscopic image and subsequently identified the tumor and simulated the resection line (Figure 2). Following partial lung resection using an endoscopic stapler, the specimen was retrieved in a bag and a 20-Fr chest tube was inserted and the wound was closed.

Role of the team members
A surgeon, two surgical assistants, a scrub nurse, a circulating nurse, and an anesthesiologist participated in each surgery. Apart from the usual surgical preparations, a digital imaging assistant operated the TC in the OR. The digital imaging assistant wore a telephone headset and operated the Leap Motion® hand gesture tracking system. The telephone headset follows the digital imaging assistant’s voice commands to enlarge, reduce, rotate, make transparent, delete, or display an image. The Leap Motion® system digitally senses the imaging assistant’s hand motion from the telephone headset (Figure 3).

Postoperative management
The postoperative management regimen was the same as that for standard thoracoscopic partial lung resection. Our protocol for removing the chest tube ensures that there is no air leakage from the chest tube and no problem with X-ray image diagnosis. All patients were discharged three to four days after the surgery.
Tips, tricks, and pitfalls
The proposed navigation system is based on the 1-mm slice enhanced chest CT and requires no other examination. Therefore, preoperative inspection is less invasive than the other marking methods. Moreover, matching images using the TC is both easy and quick, which is a remarkable point of this novel intraoperative navigation system. This system allows the surgeon to easily compare the monitor and 3D views to smoothly conduct surgical procedures.
Conclusions
The proposed navigation system allows for a less invasive procedure because it requires only preoperative CT before surgery and also because of the use of a TC in the OR.
Acknowledgments
We wish to thank Nemoto Kyorindo Co., Ltd. and Amin Co., Ltd. for analyzing 3D images and supplying a 3D tablet computer and 3D viewing program.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.07.06). TM serves as an unpaid editorial board member of Journal of Visualized Surgery from Dec 2017 to Nov 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Individual informed consent was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yutaka Y, Sato T, Zhang J, et al. Localizing small lung lesions in video-assisted thoracoscopic surgery via radiofrequency identification marking. Surg Endosc 2017;31:3353-62. [Crossref] [PubMed]
- Iguchi T, Hiraki T, Matsui Y, et al. Preoperative short hookwire placement for small pulmonary lesions: evaluation of technical success and risk factors for initial placement failure. Eur Radiol 2018;28:2194-202. [Crossref] [PubMed]
- Sato M, Omasa M, Chen F, et al. Use of virtual assisted lung mapping (VAL-MAP), a bronchoscopic multispot dye-marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J Thorac Cardiovasc Surg 2014;147:1813-9. [Crossref] [PubMed]
- Chen YR, Yeow KM, Lee JY, et al. CT-guided hook wire localization of subpleural lung lesions for video-assisted thoracoscopic surgery (VATS). J Formos Med Assoc 2007;106:911-8. [Crossref] [PubMed]
- Yamanashi K, Tokuno J, Sumitomo R, et al. A case of thoracoscopic wedge lung resection of small-sized ground-glass nodules using virtual-assisted lung mapping. Jpn J Lung Canc 2015;55:206-11. [Crossref]
- Volonté F, Robert JH, Ratib O, et al. A lung segmentectomy performed with 3D reconstruction images available on the operating table with an iPad. Interact Cardiovasc Thorac Surg 2011;12:1066-8. [Crossref] [PubMed]
- Noda Y, Matsudaira H, Asano H, et al. Monitor image obtained via a thoracoscope compared with the tablet computer (TC) image in the same view in the operating room. Asvide 2018;5:629. Available online: http://www.asvide.com/article/view/25937
- Noda Y, Matsudaira H, Asano H, et al. The digital imaging assistant is wearing the telephone headset, which is operated using the Leap Motion® system. Asvide 2018;5:630. Available online: http://www.asvide.com/article/view/25938
Cite this article as: Noda Y, Matsudaira H, Asano H, Odaka M, Yamashita M, Mori S, Shibasaki T, Kato D, Tsukamoto Y, Morikawa T, Ohki T. A novel intra-operative navigation system for resection of small lung nodules by video-assisted thoracoscopic surgery (VATS) using three-dimensional image construction in real time and on site with a tablet computer. J Vis Surg 2018;4:150.


