
Thoracoscopic anatomical S10 segmentectomy: a posterior approach
Introduction
The indications for performing a thoracoscopic segmentectomy have been growing owing to significant advancements in surgical techniques. However, this procedure is usually limited to anatomically simple and easy procedures such as left upper division, lingular (S4+5), and S6 segmentectomies. Intersegmental dissection is not procedurally difficult during such segmentectomies because the dissection can be performed along a single intersegmental plane with the use of stapling devices. Anatomical resection of the dorsal area of the basal segment of the lower lobe is difficult because of the deep-seated vessels and bronchi in the parenchyma in this anatomical location and the presence of multiple dissection surfaces.
We describe the video-assisted thoracic surgery procedure for an anatomical right S10 segmentectomy based on simulation of the surgical margin and bronchovascular branching using three-dimensional computed tomography (3D-CT) reconstruction (1,2).
Case presentation
A 67-year-old woman who underwent distal pancreatectomy for pancreatic cancer was referred to our department. Chest CT showed a solid lung nodule that was observed to have increased in size up to 8 mm in the S10 area and an aberrant segment called the sub-superior segment (S*) between S6 and S10. Thoracoscopic wedge resection was performed followed by S10 segmentectomy because frozen section examination of this nodule confirmed the diagnosis of an adenocarcinoma; however, metastasis or primary lung cancer could not be conclusively diagnosed. The operative time was 135 min, and the estimated blood loss could not be measured. Air leakage was not observed, and the chest tube was removed on postoperative day 1.
Procedure
The arteriovenous branching pattern was identified based on accurate assessment of 1-mm slice axial images and 3D reconstruction of multidetector CT data. Bronchial anatomy was not difficult to determine because bronchi are known to run alongside the pulmonary artery. General anesthesia was administered using a double-lumen endotracheal tube. The patient was placed in a lateral position with the left upper extremity fixed onto the hand shelf. The surgeon stood posterior to the patient.
A 20-mm soft silicone port with a smoke suction channel (used by the assistant) was placed in the 4th intercostal space along the left anterior axillary line. The 30° 10-mm rigid scope was placed in the 8th intercostal space along the right mid-axillary line. Subsequently, 5- and 12-mm flexible ports for the surgeon were placed in the 6th and 8th intercostal space, respectively, along the left posterior axillary line.
Initially, the inferior pulmonary vein was dissected and each branch was identified, and the lung parenchyma was incised along the inferior basal vein that runs between S10 and S7. After re-confirming the course of the superior and sub-superior veins (V6 and V*), the lung parenchyma was incised along V* that was observed to run between S* and S10. The hilum of S10 was exposed posteriorly, and the posterior basal bronchus (B10) and the posterior basal artery (A10) were isolated. B10 was looped using a monofilament polypropylene suture, and an extracorporeal slip knot was created following which A10 was divided after ligation. The anesthetist was instructed to ventilate the bilateral lungs using pure oxygen. During ventilation, the end of the suture was pulled, and the knot slipped to reach the bronchus without a knot pusher such that segmental air within S10 was observed to be trapped. Unilateral ventilation was resumed, and B10 was divided using a stapler. As further dissection of hilar parenchyma was continued, venous tributaries draining the segments (intra-segmental veins) were divided, and the inflation-deflation lines between segments became apparent. The lung parenchyma was incised along the inflation-deflation lines and eventually the peripheral lung tissue was divided using staplers. Fibrin glue was sprayed at the site of the remnant cut surface, and the edges of S* and S10 were approximated using a loop-tie (Figure 1). The operative time was 135 min, and the estimated blood loss could not be measured. Air leakage was not observed, and the chest tube was removed on postoperative day 1.
Comments
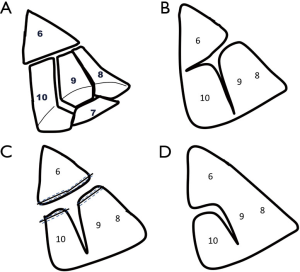
We emphasize the importance of 3D simulation using multidetector CT for accurate interpretation of individual segmental anatomy to perform a safe, effective and meticulous anatomical segmentectomy under total thoracoscopic visualization. Following the introduction of this method, we have observed that a greater number of difficult segmentectomies can now be performed (1,2). Anatomical resection of the dorsal area of the basal segment of the lower lobe is difficult because of the deep-seated arrangement of vessels and bronchi in the parenchyma and the presence of multiple dissection surfaces (Figure 2A). The usual surgical approach for this segment involves access from the interlobar fissure, dividing the lung parenchyma between the superior segment (S6) and the anterior basal segment (S8) to expose the deep-seated target pulmonary artery (A10, A9+10) and bronchus (B10, B9+10), particularly when open procedures are performed (Figure 2B) (4). Our initial series of total thoracoscopic lung segmentectomies included only 1 S9+10 segmental resection among 30 segmentectomies performed 10 years ago—the operation was performed via the interlobar fissure at that time (1). Another option may be a method splitting superior and basal segments using staplers and then dissecting the intersegmental plane between S9 and S10 (Figure 2C). During the course of our practice, we encountered a patient with an incomplete fissure in whom this approach was technically difficult because passage through the interlobar components was not easy and this led to the development of the posterior approach for S9+10 segmentectomies performed with accurate anatomical evaluation guided by 3D-CT surgical simulation (5). We used this new approach for thoracoscopic S10 segmentectomies (6), and to date, we have performed 28 S10 or S9+10 segmentectomies using this method (Figure 2D).
This method requires a thorough understanding of the anatomy particularly the veins running between the superior and basal segments. Usually, the superior vein receives 3 subsegmental tributaries: V6a, V6b and V6c. V6a drains S6, whereas V6b and V6c run their course between the superior and basal segments. A parenchymal incision made along these intersegmental veins using an ultrasonically activated device or bipolar tissue sealing and dividing system leads to the bronchus B10 or B9+10 posteriorly and facilitates the management of the target bronchus and the neighboring artery. Thus, V6 is the landmark to identify the intersegmental plane between the superior and basal segments (6). However, our patient showed an additional S* that required accurate identification of the relevant vein associated with that segment. In this patient, we dissected the lung along the intersegmental vein (sub-superior vein) from the posterior aspect. When the fissure is complete and the pulmonary artery can be managed easily the artery (A10) may be managed through the interlobar space.
Additionally, in this patient, we incised the parenchyma along the inferior basal vein between S10 and S7. However, the anatomy of intersegmental veins between S10 and S7 shows wide variations between patients; therefore, intersegmental dissection must be performed using an individualized approach based on accurate CT-guided understanding of the anatomy. Various methods have been reported to identify the segmental border. Creation of an inflation-deflation line provides an accurate understanding of the anatomy and division of the intersegmental plane because the line of demarcation does not disappear once it has been created and can be easily visualized (7-9).
This approach is beneficial in patients presenting with incomplete lobulation and in whom the hilar components are not easily accessible via the interlobar fissure. Additionally, this approach can avoid parenchymal division between the superior (S6) and anterior and lateral basal segments (S8, S9) even when the major fissure is well developed and the hilum is easily accessible. However, this approach might not enable hilar lymph node dissection. Thus, we propose that this technique is indicated for early-stage lung cancer and pulmonary metastasis in patients not requiring lymph node dissection (6).
In conclusion, a thoracoscopic anatomical S10 segmentectomy can be optimally performed via a posterior approach after gaining a thorough understanding of the intersegmental veins and the creation of an inflation-deflation line to serve as an intersegmental border. This procedure can eliminate the need for additional parenchymal division from the major fissure.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alessandro Brunelli) for the series “Uncommon Segmentectomies” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.06.15). The series “Uncommon Segmentectomies” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Oizumi H, Kanauchi N, Kato H, et al. Total thoracoscopic pulmonary segmentectomy. Eur J Cardiothorac Surg 2009;36:374-7; discussion 377. [Crossref] [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Oizumi H, Kato H, Suzuki J, et al. 3D-CT angiography and surgical procedure. Asvide 2018;5:615. Available online: http://www.asvide.com/article/view/25828
- Nomori H, Okada M. Illustrated anatomical segmentectomy for lung cancer. Springer, 2012:92-113.
- Oizumi H, Kato H, Fukaya F, et al. A posterior approach for lateral posterior basal bisegmentectomy of the lower lobes. J Jpn Assoc Chest Surg 2011;25:235-7. [Crossref]
- Endoh M, Oizumi H, Kato H, et al. Posterior approach to thoracoscopic pulmonary segmentectomy of the dorsal basal segment: A single-institute retrospective review. J Thorac Cardiovasc Surg 2017;154:1432-9. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. [Crossref] [PubMed]
- Endoh M, Oizumi H, Kato H, et al. How to demarcate intersegmental plane with resected-segments inflation method using the slip knot technique in thoracoscopic anatomic segmentectomy. J Vis Surg 2017;3:100. [Crossref] [PubMed]
Cite this article as: Oizumi H, Kato H, Suzuki J, Hamada A, Nakahashi K, Takamori S, Sadahiro M. Thoracoscopic anatomical S10 segmentectomy: a posterior approach. J Vis Surg 2018;4:142.


