
Video-assisted thoracoscopic surgery (VATS) resection of a right paratracheal ectopic thyroid: a case report
Introduction
An ectopic thyroid gland is defined as thyroid tissue that is not located anterolaterally to the second to fourth tracheal cartilages (1). Anatomically, an ectopic thyroid can be anywhere along the course of the embryologic migration of the thyroid gland, from the foramen cecum to the pre-tracheal position.
Ectopic intrathoracic thyroid goiter is a rare entity accounting for less than 1% of all ectopic thyroid cases (1). Conversely, intrathoracic thyroid goiters represent 5.8% of all mediastinal masses (2), and should be considered as a differential diagnosis for a mediastinal mass.
Up to 40% of intrathoracic thyroid goiters are asymptomatic and diagnosed incidentally (2). Clinical manifestations are usually due to compressive symptoms on the trachea or esophagus, causing dyspnea, cough, or dysphagia (3). Less frequently observed are compressive effects on the neurovascular structures in the chest, with rare cases of superior vena cava syndrome having been reported previously (2). Even if asymptomatic, they should be surgically resected due to the risk of malignancy and to avoid the potential effects of the mass on the trachea, esophagus and vena cava (1).
At present, the surgical approach for an intrathoracic goiter is dependent upon its blood supply and location. Mediastinal goiters can be divided into primary and secondary goiters (4). Primary mediastinal goiters, such as in the case presented here, derive their blood supply from intrathoracic vessels, thus extra-cervical incisions are often required for the resection of these masses (4). In contrast, the more common secondary form represents large cervical thyroid goiters that have extended into the superior mediastinum (4). These, like most thyroid goiters, derive their blood supply from thyroid vessels in the neck and are usually resected via a cervical approach, unless there are specific indications for extra-cervical incisions, such as extension into the posterior mediastinum (4).
There are a variety of extra-cervical approaches to remove intrathoracic goiters, such as median sternotomy, posterolateral thoracotomy and more recently, video-assisted thoracoscopic surgery (VATS). This case report describes our technique of employing VATS in the resection of a right paratracheal ectopic thyroid.
Patient selection and workup
A 62-year-old female who initially presented with neck pain was referred for surgical removal of a mediastinal mass in the right paratracheal region. She was otherwise well with no known comorbidities or significant past medical history. Physical examination was unremarkable.
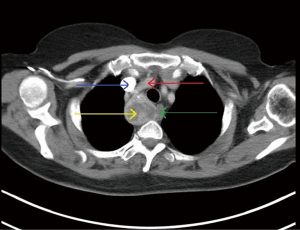
Magnetic resonance imaging (MRI) of the cervical spine did not show significant cervical spine abnormality, but there was a solid-enhancing right-sided mediastinal mass with mild mass effect on the upper thoracic trachea and esophagus. Computed tomography (CT) scans of the thorax demonstrated a 4.1 cm × 3.8 cm × 5.4 cm heterogeneously enhancing mass in the right paratracheal region, which displayed foci of calcification and central regions of necrosis (Figure 1). There was displacement of the esophagus with mild compression. Based on these findings, the differential diagnosis included a necrotic lymph node, a bronchogenic cyst, or a neurogenic tumour.
Equipment preference card
Alexis soft tissue wound retractor (Applied Medical, Rancho Santa Margarita, California, USA), 30-degree 10 mm camera (Olympus, Tokyo, Japan), Yankauer suction catheter, EL314 endoscopic clip applier (Ethicon, Cincinnati, Ohio, USA), Harmonic blade hook tip (Ethicon) and Harmonic scalpel (Ethicon).
Procedure
Under general anesthesia, the patient was placed in a left lateral decubitus position with left single lung ventilation achieved by a double-lumen endotracheal tube.
Three incisions were employed. The camera port, into which the 30-degree 10 mm endoscope was introduced, was a 1 cm incision made in the right seventh intercostal space at the mid-axillary line. A 3 cm utility incision was made in the right fourth intercostal space at the anterior axillary line. The third incision was a 1 cm incision in the right sixth intercostal space just below the tip of the scapula (Figure 2).

The mass was located in the right paratracheal region between the trachea, which was mildly displaced by the mass, and the superior vena cava. It was also located close to the apex of the chest, abutting the right subclavian artery which was just superior to the mass.
The parietal pleura was incised around the mass circumferentially with the Harmonic blade hook tip. Subsequently, a combination of blunt dissection with a Yankauer suction catheter and sharp dissection with the Harmonic blade hook tip was used to separate it from the vital structures closely related to the mass. The Harmonic blade hook tip provided hemostasis while avoiding the use of electrocautery, which may result in thermal injury to the surrounding trachea, esophagus, vagus nerve, subclavian artery and superior vena cava.
Once the mass was mobilized from the surrounding structures, the vascular pedicle was identified and controlled by endoscopic clipping, followed by division with a Harmonic scalpel. The mass was subsequently removed in an endoscopic bagging device (Figure 3).

For drainage, a 24-Fench chest tube was positioned posteriorly at the apex of the chest.
Postoperative management
The chest tube was initially placed at −20 cm water suction for the immediate postoperative period, but suction was turned off on postoperative day 1. The chest tube was removed on postoperative day 2, and the patient was discharged on the same day.
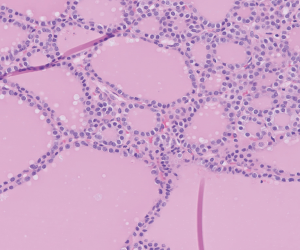
On gross examination, the thinly encapsulated mass had a reddish soft appearance with haemorrhage, colloid-like and more solid pale tan areas. Microscopic examination confirmed ectopic thyroid tissue with small and larger thyroid follicles lined by follicular cells with round granular without nuclear grooves or pseudoinclusions (Figure 4). Parathyroid tissue is also noted adjacent to the large thyroid nodule. The patient was asymptomatic preoperatively, and is still euthyroid postoperatively.
Tricks and pitfalls
The preoperative CT scan was reviewed thoroughly prior to the procedure, and the relations of the mass to surrounding structures were identified. Subsequently, these structures were carefully protected intraoperatively to avoid injury to them (Figure 5).

Beginning the dissection at the inferior aspect of the mass may aid subsequent dissection of the mass, since the weight of the mass will pull it away from its superior attachments.
Discussion
The majority of intrathoracic goiters are removed via a trans-cervical approach. Cho and colleagues recommended a trans-cervical approach even for goiters extending into the aortic arch based on their experience of 70 patients with substernal (secondary mediastinal) goiters (8). Their finding that a large majority of substernal goiters can be safely removed with a conventional trans-cervical approach has been confirmed by several other groups (9-11).
However, in patients with a primary mediastinal goiter, the intrathoracic goiter may be simply inaccessible by the trans-cervical approach (12,13). Ehrenhaft and Buckwalter recommended a sternotomy for anterior mediastinal goiters, and a right lateral thoracotomy for posterior mediastinal goiters (14). Others have even advocated a transclavicular approach, with resection of the middle third of the clavicle and extraperiosteal disarticulation (15).
In contrast, VATS resection of mediastinal goiters is an excellent alternative to thoracotomy or sternotomy and their associated morbidity. VATS was introduced in the 1990s and quickly became widely used for the diagnosis and treatment of a variety of intrathoracic diseases, including mediastinal lesions. It is now generally regarded as the gold standard in management for most general thoracic surgical problems, from pleurodesis procedures for pneumothorax to major pulmonary resections for lung cancer. Compared to an operation requiring a sternotomy or thoracotomy, it is associated with decreased postoperative pain, reduced length of hospital stay and fewer postoperative complications (16).
Despite the benefits of VATS, some surgeons may feel uncomfortable with this approach to access the upper mediastinum, as it is a delicate area with many important structures that are at risk of being injured if one is unfamiliar with the relevant anatomical relationships (12). This risk is further exacerbated by the loss of depth perception with the 2-dimensional view afforded by the camera and the intensification of hand tremor by using thoracoscopic instruments (12). However, with proper planning, appropriate instrumentation and sufficient training, VATS resection of mediastinal masses can be performed safely, as demonstrated in this case.
In summary, an intrathoracic goiter is a rare manifestation of ectopic thyroid tissue outside the neck, and can occasionally present as a mediastinal mass with a wide range of differential diagnoses. When surgical resection is contemplated, we believe that VATS is an excellent approach that has several benefits compared to a traditional open procedure.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.06.01). BHO reports non-financial support from Johnson & Johnson, non-financial support from Medtronic, non-financial support from Broncus, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roh E, Hong ES, Ahn HY, et al. A case of mediastinal ectopic thyroid presenting with a paratracheal mass. Korean J Intern Med 2013;28:361-4. [Crossref] [PubMed]
- Di Crescenzo V, Vitale M, Valvano L, et al. Surgical management of cervico-mediastinal goiters: Our experience and review of the literature. Int J Surg 2016;28:S47-53. [Crossref] [PubMed]
- Grondin SC, Buenaventura P, Luketich JD. Thoracoscopic resection of an ectopic intrathoracic goiter. Ann Thorac Surg 2001;71:1697-8. [Crossref] [PubMed]
- Pilavaki M, Kostopoulos G, Asimaki A, et al. Imaging of ectopic intrathoracic multinodular goiter with pathologic correlation: a case report. Cases J 2009;2:8554. [Crossref] [PubMed]
- Tay WL, Hwang JS, Ong BH. Incisions. Asvide 2018;5:592. Available online: http://www.asvide.com/article/view/25576
- Tay WL, Hwang JS, Ong BH. Removal of mass. Asvide 2018;5:593. Available online: http://www.asvide.com/article/view/25577
- Tay WL, Hwang JS, Ong BH. Preoperative CT images. Asvide 2018;5:594. Available online: http://www.asvide.com/article/view/25578
- Cho HT, Cohen JP, Som ML. Management of substernal and intrathoracic goiters. Otolaryngol Head Neck Surg 1986;94:282-7. [Crossref] [PubMed]
- Judd ES, Beahrs OH, Bowes DE. A consideration of the proper surgical approach for substernal goiter. Surg Gynecol Obstet 1960;110:90-8. [PubMed]
- Gourin A, Garzon AA, Karlson KE. The cervicomediastinal approach to intrathoracic goiter. Surgery 1971;69:651-4. [PubMed]
- Erbil Y, Bozbora A, Barbaros U, et al. Surgical management of substernal goiters: clinical experience of 170 cases. Surg Today 2004;34:732-6. [Crossref] [PubMed]
- Bodner J, Fish J, Lottersberger AC, et al. Robotic resection of an ectopic goiter in the mediastinum. Surg Laparosc Endosc Percutan Tech 2005;15:249-51. [Crossref] [PubMed]
- Podgaetz E, Gharagozloo F, Najam F, et al. A novel robot-assisted technique for excision of a posterior mediastinal thyroid goiter: a combined cervico-mediastinal approach. Innovations (Phila) 2009;4:225-8. [Crossref] [PubMed]
- Ehrenhaft JL, Buckwalter JA. Mediastinal tumors of thyroid origin. AMA Arch Surg 1955;71:347-56. [Crossref] [PubMed]
- D'Alia C, Tonante A, Lo Schiavo MG, et al. Transclavicular access as an adjunct to standard cervical incision in the treatment of mediastinal goitre. Chir Ital 2002;54:576-80. [PubMed]
- Reddy RV. The advantages of VATS: a systematic review. Thorax 2005;60:238. [Crossref]
Cite this article as: Tay WL, Hwang JSG, Ong BH. Video-assisted thoracoscopic surgery (VATS) resection of a right paratracheal ectopic thyroid: a case report. J Vis Surg 2018;4:125.


