Advantages of and problems encountered with UICC version 8 TNM staging system for thymic epithelial tumors
Historical thymic epithelial tumor staging system issues
Thymic epithelial tumors, including thymoma, thymic carcinoma, and thymic neuroendocrine carcinoma, are rare neoplasms. Since most clinicians have limited exposure to affected patients, it is important to share experiences among attending physicians in order to develop a standard strategy for diagnosis and treatment of patients, especially consensus establishment of a pathological classification and staging system.
Since the early 2000s, pathological classification of thymic epithelial tumors has been a major topic of discussion and research, because their microscopic appearance varies and oncological behavior is quite different among tumors according to that appearance. Several classification systems have been proposed, resulting in confusion for clinicians regarding nomenclature and difficulty with understanding the significance of pathological diagnosis. Recently, the World Health Organization (WHO) proposed a new system of pathological classification (1), mainly based on the proposals by Bürtzburg’s group, and worldwide consensus was finally obtained after several clinical studies conducted by major institutions throughout the world to confirm its clinical significance (2-5). With the settlement of issues related to pathological classification, the primary interest is now focused on an effective staging system.
Several staging systems have been proposed, mostly by surgeons, among which the Masaoka clinico-pathological classification presented in 1981 (6) has become the most well-known and widely accepted for more than 30 years. Masaoka’s staging system combined and modified Bergh’s (7) and Willkins’ systems (8), with local invasiveness emphasized as the most significant prognostic factor. However, probably because of the small number of cases with lymphatic spread, the significance of nodal involvement was not fully investigated and affected cases are tentatively considered to be stage IVB. In addition, during development of this staging system, understanding of the pathology of thymic epithelia tumors was quite poor and comprehension of thymic carcinoma was not common. Since the 1970s, there has been enormous progress in most fields of medicine, especially imaging technology including CT scanning and MRI, as well as video-assisted thoracoscopic surgery (VATS). Consequently, the Masaoka staging system, established by clinical experience and outcomes prior to 1980, is difficult to adapt to more modern clinical practice.
Another background issue regarding staging of thymic epithelial tumors is the question of whether a single system can be applicable to all related neoplasms, as it has been suggested that thymoma, thymic carcinoma, and thymic neuroendocrine carcinoma should have a staging system that reflects their unique oncological characteristics, or a staging system should be determined exclusively according to tumor extension irrespective of pathology. Unfortunately, there was no international organization available to address these issues prior to 2010.
Global database of thymic epithelial tumors
The International Conference of Thymic Malignancy, held at the National Institutes of Health (NIH) in Bethesda, USA, in 2009, was likely the initial international conference to focus on thymic neoplasms. The next year (2010), the International Thymic Malignancy Interest Group (ITMIG), the first international academic organization specifically related to thymic neoplasms, was formed, and began activities to offer opportunities for establishing a common understanding and promote discussion of thymic tumors among members of the international medical community. Furthermore, members of the group confirmed the necessity of a global database project to establish a new staging system.
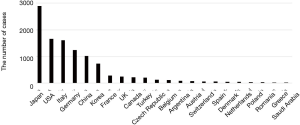
Following the first annual conference held in New York in 2010, ITMIG began a global project to establish a retrospective database of cases. At that time, the European Society of Thoracic Surgeons (ESTS) had already developed their own retrospective database of 1700 patients and provided support for the ITMIG global database project. In addition, the Japanese Association for Research of the Thymus (JART) independently started a retrospective database project of cases in Japan in 2011, which was followed by independent database projects being conducted in South Korea and China. Finally, ITMIG compiled data from 22 countries and in 2014 completed the database of 10,808 patients, comprised of 6,097 (56%) cases registered by ITMIG, 2,897 (27%) by JART, 1,814 (17%) by ESTS (9). Cases registered by each participating country are shown in Figure 1.
Proposal for new staging system
The ITMIG concept of a new staging system included the anatomic extent of disease based on T, N, and M definitions, and also an ability to apply it to all types of thymic epithelial neoplasms. At the same time, another important aim of the new staging system was compatibility with the existing Masaoka classification.
ITMIG and the thymic domain of the Staging and Prognostic Factors Committee (SPFC) of the International Association for Study of Lung Cancer (IASLC) collaboratively analyzed the retrospective database, and finally proposed a new TNM-based staging system. Definitions of TNM are described in Table 1 and those of the stage groupings in Table 2, while the relationship between Masaoka’s system and this new TNM-based staging system is also described in Table 2 (10-12).
Table 1
| T factor |
| T1a: encapsulated or unencapsulated, with or without extension into mediastinal fat |
| T1b: extension into mediastinal pleura |
| T2: extension into pericardium |
| T3: extension into lung, brachiocephalic vein, superior vena cava, chest wall, phrenic nerve, hilar (extrapericardial) pulmonary vessels |
| T4: extension into aorta, arch vessels, main pulmonary artery, myocardium, trachea, esophagus |
| N factor |
| N0: no nodal involvement |
| N1: involvement of anterior (perithymic) nodes |
| N2: involvement of deep intrathoracic or cervical nodes |
| M factor |
| M0: no metastatic pleural, pericardial, or distant sites |
| M1a: separate pleural or pericardial nodule(s) |
| M1b: pulmonary intraparenchymal nodule or distant organ metastasis |
Table 2
| Stage | T | N | M | Masaoka’s classification |
|---|---|---|---|---|
| I | T1 | N0 | M0 | I, II |
| II | T2 | N0 | M0 | III |
| IIIa | T3 | N0 | M0 | III |
| IIIa | T3 | N0 | M0 | III |
| IIIa | T3 | N0 | M0 | III |
| T any | N0, 1 | M1a | IVa, IVb | |
| IVb | T any | N2 | M0, 1a | IVb |
| T any | N any | M1b | IVb |
Value of new TNM-based staging system
The staging system based on TNM proposed by ITMIG and IASLC was finally approved by the Union for International Cancer Control (UICC) and included in version 8 of the UICC TNM staging system, which was an important historical event for clinical practice as well as research regarding thymic epithelial tumors.
Whether a single staging system can be applicable to all types of thymic epithelial tumors which have various characteristics of biological activities and oncological behaviors was point of discussion. If the staging system for thymoma is different from that for thymic carcinoma, the situation will be more confused because stage would not be determined before pathological diagnosis is obtained. To describe the extent of a tumor using the same TNM definition is more convenient and more practical to clinicians in proceeding the clinical practice. Thus, the single definition of TNM category common to all kinds of pathology was established (10).
The definition of the T category strongly reflects the level of invasion to adjacent organs, the same philosophy used for Masaoka staging. Furthermore, T1 is sub-classified into T1a and T1b according to the absence or presence of invasion to the mediastinal pleura, though controversy remains regarding whether discrimination between stage I and stage II in Masaoka’s classification is necessary because of similar long-term survival of affected patients. The N category was also defined, even though solid evidence for determining N factors is lacking. Accumulation of cases with nodal involvement should help to elucidate its significance in terms of long-term survival.
This new TNM-based staging system is expected to contribute to increased global collaborative research because of use of common rules for defining tumor extent, which has been desired for many years.
Future perspectives regarding the TNM-based staging system
Although many problems were solved by development of this staging system based on TNM classification, several clinical questions still remain to be answered. The ITMIG retrospective database mainly consists of records of patients who underwent surgical treatment and is lacking information regarding those who did not undergo an operation. Thus, the definitions of M factor and stage IV require further investigation.
A study conducted using the JART retrospective database suggested the prognostic significance of number of lesions disseminated on the pleura, an issue not analyzed for development of the ITMIG/ISLC global database. Also, research using JART retrospective database showed that invasion to the thoracic wall is an independent adverse prognostic factor among Masaoka stage III disease, suggesting reconsideration on definition of T3 and T4.
Furthermore, tumor size is not included in the definition of T factor in the new staging system, even though several studies have showed findings indicating its prognostic significance. Furthermore, analysis of the global retrospective database did not reveal significance of tumor size, though that might have been the result of poor information contained in the database. There may also be other clinical questions remaining to be answered. Nevertheless, establishment of the ITMIG prospective database project is important, and accumulation of more detailed and correct data including from non-surgical cases will provide greater insight into these issues.
Conclusions
A new TNM-based staging system was established based on a retrospective database created by an international collaboration of a large number of clinicians and researchers. This staging system should promote additional studies of these rare neoplasms throughout the world. On the other hand, information from unresectable cases is lacking. Additional development along with use of the prospective database and staging system are expected to provide answers to important clinical questions, resulting in better patient care.
Acknowledgments
The author is grateful to all the member of the thymic domain of Staging and Prognostic Factor Committee (SPFC) of IASLC for their efforts to establish the TNM-based staging system.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Tommaso Claudio Mineo) for the series “Mediastinal Surgery” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.05.22). The series “Mediastinal Surgery” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Travis WD, Brambilla E, Mueller-Hermelink HK, et al. Pathology and genetics of tumours of the lung, pleura, thymus and heart. World Health Organization Classification of Tumours. Lyon, France: IARC Press; 2004.
- Okumura M, Miyoshi S, Fujii Y, et al. Clinical and functional significance of WHO classification on human thymic epithelial neoplasms. A study of 146 consecutive tumors. Am J Surg Pathol 2001;25:103-10. [Crossref] [PubMed]
- Okumura M, Ohta M, Tateyama H, et al. WHO histologic classification reflects oncological behaviors of human thymoma. A clinical study of 273 patients. Cancer 2002;94:624-32. [Crossref] [PubMed]
- Chen G, Marx A, Chen WH, et al. New WHO histological classification predicts prognosis of thymic epithelial tumors. A clinicopathological study of 200 thymoma cases from China. Cancer 2002;95:420-9. [Crossref] [PubMed]
- Nakagawa K, Asamura H, Matsuno Y, et al. Thymoma: a clinicopathologic study based on the new World Health Organization classification. J Thorac Cardiovasc Surg 2003;126:1134-40. [Crossref] [PubMed]
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [Crossref] [PubMed]
- Bergh NP, Gatzinsky P, Larsson S, et al. Tumors of the thymus and thymic region: I. Clinicopathological studies on thymomas. Ann Thorac Surg 1978;25:91-8. [Crossref] [PubMed]
- Wilkins EW Jr, Castleman B. Thymoma: a continuing survey at the Massachusetts General Hospital. Ann Thorac Surg 1979;28:252-6. [Crossref] [PubMed]
- Detterbeck FC, Asamura H, Crowley J, et al. The IASLC/ITMIG thymic malignancies staging project: development of a stage classification for thymic malignancies. J Thorac Oncol 2013;8:1467-73. [Crossref] [PubMed]
- Detterbeck FC, Stratton K, Giroux D, et al. The IASLC/ITMIG thymic epithelial tumors staging project: proposal for an evidence-based stage classification system for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S65-72. [Crossref] [PubMed]
- Nicholson AG, Detterbeck FC, Marino MStaging and Prognostic Factors Committee, et al. Members of the Advisory Boards; Participating Institutions of the Thymic Domain. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposals for the T Component for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S73-80. [Crossref] [PubMed]
- Kondo K, Van Schil P, Detterbeck FCStaging and Prognostic Factors Committee, et al. Members of the Advisory Boards; Participating Institutions of the Thymic Domain. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposals for the N and M components for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S81-7. [Crossref] [PubMed]
Cite this article as: Okumura M. Advantages of and problems encountered with UICC version 8 TNM staging system for thymic epithelial tumors. J Vis Surg 2018;4:121.