An unusual etiology of hyperparathyroidism: robotic-assisted resection of a giant functional intrathymic parathyroid cyst
Introduction
Ectopic parathyroid glands are common, including intrathymic, intrathyroidal, tracheoesophageal groove, retroesophageal, and carotid sheath localization (1). In a recent retrospective review involving 346 patients with ectopic parathyroid adenomas, approximately one-third were intrathymic (1-3). Less common than an ectopic adenoma, however, is the parathyroid cyst (PC) with approximately 300 cases reported (4,5). Of these PCs, first described in the late 19th century, the majority are classified as non-functional (4). Functional PCs are thought to occur secondary to degeneration of parathyroid adenomas (4,6). While non-functional PCs do not necessary require resection, unless there is associated compressive symptomatology, most functional PCs meet criteria for resection, secondary to significant associated symptoms or end organ damage. With the exception of a few especially large PCs (11–14 cm), the majority of PCs range from 1–8 cm (7-11). Classically accessed via cervical anterior approach, sternotomy, or thoracotomy, video-assisted thoracoscopic surgery (VATS) is now the mainstay of therapy for these surgically challenging lesions; however, the recent introduction of robotic surgery offers an alternative approach with distinct advantages (7-10,12-15). The literature includes several reports of robotically resected mediastinal adenomas and cysts; however, to our knowledge, this is the first report of a robotically resected intrathymic functional PC (12-16).
Case presentation
A 61-year-old man was evaluated in endocrine surgery clinic for primary hyperparathyroidism and an asymptomatic nontoxic uninodular goiter. High serum total calcium (STC) levels were first noted six months prior to presentation during routine blood testing. At that time, the STC was markedly elevated at 14.5 mg/dL (normal level 8.4–10.5 mg/dL), with associated parathyroid hormone (PTH) also significantly increased at 570 pg/mL (normal level 10–65 pg/mL). A 24-hour urine calcium level was high normal at 290 mg. The patient reported fatigue, body aches, mild confusion and short-term memory deficits, occasional palpitations, recurrent nephrolithiasis and polyuria. He denied depression, constipation, reflux, abdominal pain, and bone pain. A serum thyroid stimulating hormone level was normal at 2.0 mU/L. Remaining past medical history was non-contributory; however, he took Ergocalciferol for low Vitamin D levels. Aside from paternal thyroid disease, the patient denied family history of endocrinology. The patient had no history of ionizing radiation exposure, but smoked 1/2 packs-per-day for 40 years; however, had quit smoking one week prior to surgery. Associated imaging, including Dual-phase Tc-99m sestamibi SPECT-CT scan (Figure 1) and a neck ultrasound, was negative for parathyroid disease localization (such negative findings are not uncommon, as the localization sensitivity of ultrasound and sestamibi scanning are generally reported to be in the 70–80% range) (3,17). A 4-dimensional computed tomography (4D-CT) scan of the neck and upper chest identified enlarged left upper and right lower parathyroid glands. Given his biochemical, clinical, and radiological findings, the patient underwent bilateral neck exploration with resection of right upper and left lower parathyroid adenomas. A normal left upper parathyroid gland was identified and was left in situ. The right lower parathyroid gland was not identified. Unfortunately, intraoperative blood PTH level testing revealed persistent elevation following two-gland excision, remaining in the 500 pg/mL range, consistent with persistent disease. Additional extensive neck exploration failed to reveal the causative parathyroid tissue. With the possibility of an intrathyroidal right-sided parathyroid adenoma, a right thyroid lobectomy was performed. Nonetheless, blood PTH levels remained unchanged (elevated) following this maneuver and the operation was then stopped, in favor of additional postoperative localization imaging.
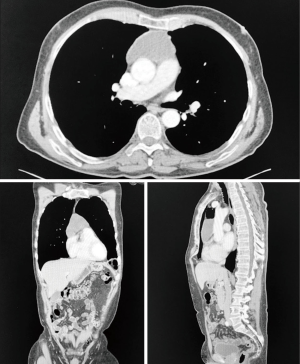
Two weeks postoperatively STC and PTH remained elevated at 14.4 mg/dL and 936 pg/mL, respectively. Six weeks later, additional parathyroid localization imaging using 4D-CT with attenuation correction was performed, with expansion of the imaging field to include the chest, given the possibility of a low lying mediastinal parathyroid adenoma. This study demonstrated a large thymic cyst in the anterior caudal mediastinum (Figure 2). Careful radiological review of this imaging study with senior members of our radiology staff was performed and resulting consensus opinion was that the identified mass was unlikely to represent parathyroid disease given its caudal mediastinal position and the absence of any evident solid component. In light of this diagnostic uncertainty, image-guided aspiration was performed with aspirate PTH level testing. The benefit of a definitive diagnosis was felt to outweigh the very small associated risk of parathyromatosis and, indeed, this testing confirmed the mass’ parathyroid origin, revealing a significantly elevated PTH level of 273,200 pg/mL. The patient subsequently underwent robotic-assisted excision of his mediastinal mass. Following supine patient positioning with the bed tilted to the left-hand side, robotic ports were positioned on either side of the camera port in the right chest, in the 3rd, 5th and 8th intercostal spaces (ICS), respectively. A fourth Air Seal/assist port was placed in the 10th ICS. The cyst was identified and dissected free from both pleural spaces and the pericardium. Intraoperative blood PTH levels dropped from 734 pg/mL preoperatively to 114 pg/mL on completion of the cystectomy, and to 86 pg/mL 10 minutes afterward, consistent with cure by Miami Criteria (18). Postoperatively, STC remained stable but was closely monitored because of concern for hungry bone syndrome, which did not ultimately develop. The patient was discharged on postoperative day 3 with a STC of 12.5 mg/dL. At routine two-month follow-up, STC was normal at 9.2 mg/dL. Final surgical pathology noted a markedly enlarged parathyroid gland (11.0×6.0×0.4 cm, 15 grams) with cystic degeneration (Figure 3).
Discussion
Diagnosis and management of PC is accomplished using physical examination, biochemical testing (STC and PTH levels), localization imaging studies, and occasionally needle aspiration (20). Our patient had a negative ultrasound and sestamibi parathyroid disease localization during initial presentation, with suspicious adenomas detected with preoperative 4D-CT neck reconstruction. The literature describes a significant parathyroid disease localization failure rate with use of sestamibi SPECT-CT scanning, especially for ectopic mediastinal disease, leading the authors to emphasis the utility of the 4D-CT protocol as an important adjunct to increase preoperative localization accuracy (3,17,20). Furthermore, given failure of localization imaging to identify the causative parathyroid disease prior to the initial surgery, complete mediastinal imaging during preoperative workup would have been beneficial; however, our initial management would not have likely changed as a patient presenting with hyperparathyroidism-associated symptoms and concurrent radiologically identified eutopic adenomas carries a strong recommendation for resection per current guidelines (20). Nonetheless, hyperparathyroidism persisted following our initial operation and more extensive imaging identified a thymic cyst. We thus proceeded with fine needle aspiration to establish a diagnosis. Current guidelines recommend against aspiration of PCs due to insufficient evidence supporting the diagnostic value of this testing, with the exception of “unusual, difficult cases of primary hyperparathyroidism (20).” Given the peculiarity of this case, and the uncertain origin of the identified thymic cyst, in the context of persistent hyperparathyroidism, we determined that the diagnostic information gained from aspiration outweighed the small, but potential, risk of mediastinal parathyromatosis. Our decision to proceed with aspiration was reassured by the experience of one of our authors (JD Prescott) as a high volume parathyroid surgeon, with extensive experience in the management of PCs. Once the cyst was determined to be parathyroid in origin, surgical resection became indicated.
While several surgical approaches to mediastinal disease exist, there has been a movement toward minimally invasive approaches, as these techniques are associated with reduced morbidity (9,12-15,21). Similarly, various procedures are performed to remove intrathymic mediastinal cysts, from cystectomy to thymectomy; however, there is no consensus favoring one over the other (7-10,12-15,21). Nevertheless, as robotic technology is increasingly integrated into thoracic surgical practice, we believe this approach offers advantages over conventional VATS for PCs. These advantages include better operative field visualization and finer, more precise dissection capacity, which was especially important in our case with the proximity of vital structures and the small, but real, risk of parathyromatosis associated with intraoperative cyst rupture. Although we chose to pursue diagnostic cyst aspiration, the authors would like to note that venous sampling to confirm functionality of the lesion, and thus establish diagnosis, could also have been attempted in this instance before subjecting the patient to invasive mediastinal exploration (20). Serial intraoperative PTH measurements in unusual cases such as this are extremely helpful in assessing probability of surgical cure, and although several algorithms exist for assessing operative success, we choose to utilize the Miami criteria in our practice (intraoperative PTH drop >50% from highest pre-incision level at 10 minutes after resection) (18). The reported rate of recurrence with use of Miami criteria ranges from 0.4–3% (20). Postoperatively, it is critical to closely monitor and manage STC levels, given the potential for temporary hypocalcemia or even hungry bone syndrome, especially for functional cysts as reported in our patient. Aside from a single report of a mediastinal adenoma resection performed as an outpatient procedure, the length of stay after mediastinal exploration for parathyroid disease ranges from 1–7 days with a median of 3 days for minimally invasive approaches (7,9,10,12,13,15,21).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Roy M, Mazeh H, Chen H, et al. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg 2013;37:102-6. [Crossref] [PubMed]
- Okada M, Tominaga Y, Yamamoto T, et al. Location Frequency of Missed Parathyroid Glands After Parathyroidectomy in Patients with Persistent or Recurrent Secondary Hyperparathyroidism. World J Surg 2016;40:595-9. [Crossref] [PubMed]
- Karipineni F, Sahli Z, Somervell H, et al. Are preoperative sestamibi scans useful for identifying ectopic parathyroid glands in patients with expected multigland parathyroid disease? Surgery 2018;163:35-41. [Crossref] [PubMed]
- Pontikides N, Karras S, Kaprara A, et al. Diagnostic and therapeutic review of cystic parathyroid lesions. Hormones (Athens) 2012;11:410-8. [Crossref] [PubMed]
- Shields TW, Immerman SC. Mediastinal parathyroid cysts revisited. Ann Thorac Surg 1999;67:581-90. [Crossref] [PubMed]
- Khan A, Khan Y, Raza S, et al. Functional parathyroid cyst: a rare cause of malignant hypercalcemia with primary hyperparathyroidism-a case report and review of the literature. Case Rep Med 2012;2012:851941. [Crossref] [PubMed]
- Davoli F, Rena O, Pirondini E, et al. Giant functioning mediastinal parathyroid cyst: an unusual cause of exertional dyspnea and mild dysphagia. Arch Bronconeumol 2013;49:408-9. [PubMed]
- Mikami I, Koizumi K, Shimizu K, et al. Functional mediastinal parathyroid cyst: report of a case. Surg Today 2002;32:351-3. [Crossref] [PubMed]
- Dell'Amore A, Asadi N, Bartalena T, et al. Thoracoscopic resection of a giant mediastinal parathyroid cyst. Gen Thorac Cardiovasc Surg 2014;62:444-50. [Crossref] [PubMed]
- Zhang XU, Yuan JH, Feng LU, et al. Giant non-functional parathyroid cyst: A case report. Oncol Lett 2016;11:2237-40. [Crossref] [PubMed]
- Jarnagin WR, Clark OH. Mediastinal parathyroid cyst causing persistent hyperparathyroidism: case report and review of the literature. Surgery 1998;123:709-11. [Crossref] [PubMed]
- Chan AP, Wan IY, Wong RH, et al. Robot-assisted excision of ectopic mediastinal parathyroid adenoma. Asian Cardiovasc Thorac Ann 2010;18:65-7. [Crossref] [PubMed]
- Ismail M, Maza S, Swierzy M, et al. Resection of ectopic mediastinal parathyroid glands with the da Vinci robotic system. Br J Surg 2010;97:337-43. [Crossref] [PubMed]
- Timmerman GL, Allard B, Lovrien F, et al. Hyperparathyroidism: robotic-assisted thoracoscopic resection of a supernumary anterior mediastinal parathyroid tumor. J Laparoendosc Adv Surg Tech A 2008;18:76-9. [Crossref] [PubMed]
- Ward AF, Lee T, Ogilvie JB, et al. Robot-assisted complete thymectomy for mediastinal ectopic parathyroid adenomas in primary hyperparathyroidism. J Robot Surg 2017;11:163-9. [Crossref] [PubMed]
- Go P, Watson J, Lu Z, et al. Robotic resection of a mediastinal parathyroid cyst. Gen Thorac Cardiovasc Surg 2017;65:52-5. [Crossref] [PubMed]
- Ishibashi M, Nishida H, Hiromatsu Y, et al. Localization of ectopic parathyroid glands using technetium-99m sestamibi imaging: comparison with magnetic resonance and computed tomographic imaging. Eur J Nucl Med 1997;24:197-201. [Crossref] [PubMed]
- Carneiro DM, Solorzano CC, Nader MC, et al. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery 2003;134:973-9. [Crossref] [PubMed]
- Davis TA, Yesantharao P, Ha J, et al. Robotically resected functional intrathymic parathyroid cyst. Asvide 2018;5:451. Available online: http://www.asvide.com/article/view/24565
- Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg 2016;151:959-68. [Crossref] [PubMed]
- Chae AW, Perricone A, Brumund KT, et al. Outpatient video-assisted thoracoscopic surgery (VATS) for ectopic mediastinal parathyroid adenoma: a case report and review of the literature. J Laparoendosc Adv Surg Tech A 2008;18:383-90. [Crossref] [PubMed]
Cite this article as: Davis TA, Yesantharao P, Ha J, Prescott JD, Yang SC. An unusual etiology of hyperparathyroidism: robotic-assisted resection of a giant functional intrathymic parathyroid cyst. J Vis Surg 2018;4:88.



