The proximalization of the arch anastomosis
This viewpoint article and the detailed surgical techniques are demonstrated in our video (Figure 1). Open surgery for total aortic arch replacement is an established operation (2-4), however it has proven technically demanding due to the narrowness of access to such a deep site as the distal arch. Some recent attempts to simplify open aortic arch replacement have focused on the distal arch anastomosis. The “frozen elephant trunk (FET)” technique makes it easier to introduce a stent graft into the distal portion of the aortic arch. Although an FET may be ideal for some patients with acute complicated type A aortic dissection, it is associated with non-negligible incidence (at least 5%) of spinal cord ischemia when used for atherosclerotic arch aneurysms. Many aortic experts, even FET proponents, have recently been choosing alternatives to FET for chronic atherosclerotic arch aneurysms. An important question now is how best to construct the distal aortic anastomosis with the descending aortic stump. Here we introduce a technical tip, to proximalize the distal aortic anastomosis, in our approach to total aortic arch replacement.

The key pathomorphologic changes in aortic aneurysms are almost always a combination of dilatation of the lumen plus elongation of the aorta and its major branches. An atherosclerotic aneurysm of the aortic arch is often located at or beyond the distal portion of the arch, where the left subclavian artery originates. The chronic dissecting aortic aneurysm also frequently has its largest portion beyond the orifice of the left subclavian artery.
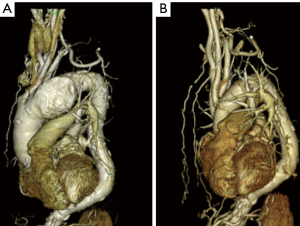
We perform open surgery for the total arch replacement with a view to these structural features. The location of the planned distal aortic anastomosis, beyond the aneurysmal portion, often appears very deep in the preoperative CT scan (Figure 2A). However, after skeletonizing the distal aortic stump, we can usually bring the distal aortic stump forwards, for a comfortably visible construction of the distal aortic anastomosis (Figure 2B).
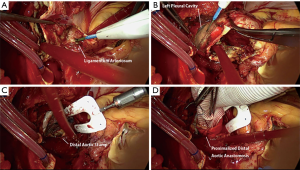
Our procedure is as follows: first, a cardiopulmonary bypass is set up, and the patient is cooled to hypothermic circulatory arrest. Second, after three antegrade cerebral perfusion catheters are introduced, the proximalization of the aortic arch can begin. As a first step, the pulmonary artery is separated into the direction of the left pulmonary artery is freed at the minor curvature of the aortic arch, to find the ligamentum arteriosum, which is then divided (Figure 3A). The left recurrent laryngeal nerve is always identified just distal to it, and must be left untouched. As a second step, at the major curvature of the arch, the parietal pleura of the left chest cavity is opened to reveal the further distal portion of the aorta (Figure 3B). The aortic arch is safely separated from the pleura which includes the left phrenic nerve and the left recurrent laryngeal nerve. The aortic arch is further separated circumferentially from the nearby trachea and esophagus down to a level beyond the arch aneurysm, and it is excised (Figure 3C). A few bronchial arteries are carefully identified and ligated using titanium clips. The key maneuver is the complete circumferential separation, or skeletonization, of at least 2 cm of the distal aortic segment. This leaves the elongated distal aortic portion fully freed or mobilized from the posterior mediastinum. Teflon felt is used to reinforce the distal stump with three sutures of 4-0 Prolene. With gentle traction on these Prolene sutures, the distal anastomosis site is considerably proximalized and construction becomes easier (Figure 3D). This most helpful exposure of the surgical field can be further facilitated with a Terumo ESTECH Surgical Assistant (Terumo Cardiovascular Systems Corporation, Ann Arbor, MI, USA).
We generally use a sealed Dacron graft, Gelweave Four Branch Plexus graft (VASCUTEK Ltd., Inchinnan, UK) for our total arch replacement. We choose a graft size to match the distal aortic stump. The distal aortic anastomosis is then constructed on the proximalized stump with adequate space around the anastomosis, using 3-0 Prolene with SH needles, so as to insert at least 5 or 6 crimps of the graft into the distal native aortic stump. The “elephant trunk” or “FET” technique is not necessary. We apply BioGlue on the anastomosis circumferentially to complete hemostasis. One of the graft branches is then re-perfused to re-check for hemostasis. The perfusion of the lower body is resumed. We initiate systemic rewarming at this point. The rest of the procedure has been previously described (5,6).
In summary, an aortic arch aneurysm is often deeply located, far from the anterior chest wall. Aortic arch replacement is easier with the distal aortic anastomosis considerably proximalized. Since the diseased aorta is almost always pathologically elongated, the mobilization and proximalization of the distal aortic segment makes this operation dramatically simpler. This is a key to performing total aortic arch replacement relatively comfortably and without trouble.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Asai T, Suzuki T, Kinoshita T. The proximalization of the arch anastomosis. Asvide 2018;5:426. Available online: http://www.asvide.com/article/view/24429
- Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg 2000;70:3-8; discussion 8-9. [Crossref] [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Improved results of atherosclerotic arch aneurysm operations with a refined technique. J Thorac Cardiovasc Surg 2001;121:491-9. [Crossref] [PubMed]
- Okita Y, Minatoya K, Tagusari O, et al. Prospective comparative study of brain protection in total aortic arch replacement: deep hypothermic circulatory arrest with retrograde cerebral perfusion or selective antegrade cerebral perfusion. Ann Thorac Surg 2001;72:72-9. [Crossref] [PubMed]
- Suzuki T, Asai T, Nota H, et al. Selective cerebral perfusion with mild hypothermic lower body circulatory arrest is safe for aortic arch surgery. Eur J Cardiothorac Surg 2013;43:e94-8. [Crossref] [PubMed]
- Asai T, Suzuki T, Nota H, et al. Total arch replacement with selective antegrade cerebral perfusion and mild hypothermic circulatory arrest. Ann Cardiothorac Surg 2013;2:235-8. [PubMed]
Cite this article as: Asai T, Suzuki T, Kinoshita T. The proximalization of the arch anastomosis. J Vis Surg 2018;4:83.


