Bronchial carcinoid in anomalous right upper bronchus: a “patient-tailored” bronchoplasty resection technique
Introduction
Neuroendocrine tumors (NET) are rare neoplasms comprising less than 20% of all lung cancers (1). Among them, primary bronchial carcinoids (BC) represent 0.4% to 3% of resected pulmonary tumors and about 25% of all carcinoids (2). Typical carcinoids (TC) show fewer than two mitoses per 2 mm2 without necrosis, whereas a TC have two to ten mitoses per 2 mm2 and necrosis (1). Although they are indolent, all BC are classified as malignant because they can locally infiltrate and metastasize.
According to the National Comprehensive Cancer Network (NCCN) and the European Neuroendocrine Tumor Society (ENETS) guidelines, resection is the primary treatment for most localized carcinoid tumors, with lung parenchymal-sparing surgery the favoured objective for patients with central airway tumors (3,4).
Sleeve bronchoplasty techniques are complex surgical procedures defined as parenchyma-saving because they allow a radical resection with tumor-free margins while preserving the maximum amount of parenchyma (5). Bronchoplasty is particularly challenging in case of bronchial carcinoid arising from an anomalous bronchial tree and requires careful preoperative evaluation and adequate surgical skills.
We describe a case of typical bronchial carcinoid of an anomalous right upper bronchus with trans-fissural involvement of the middle lobe, requiring a “patient-tailored” bronchoplasty technique.
Case presentation
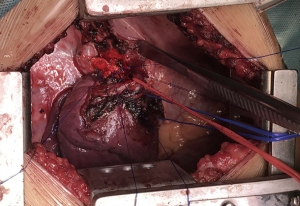
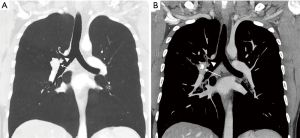
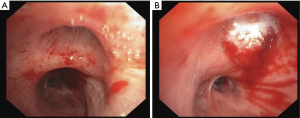
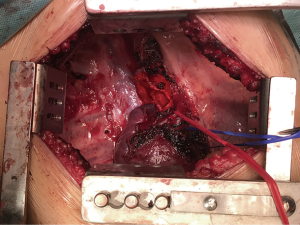
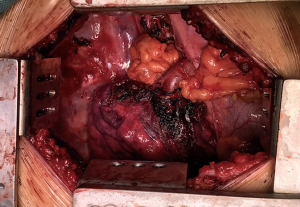
A 35-year-old man was referred to our department with a diagnosis of endobronchial lesion occluding the right upper bronchus. Computed tomography (CT) (Figure 1) and flexible bronchoscopy (FB) (Figure 2A) disclosed a bronchial anomaly consisting in a dorsal bronchial segment of the right upper bronchus arising alone directly from the right main bronchus and connected to the true right upper bronchus by an anomalous intrabronchial carina. The origin of the true right upper bronchus was obstructed by a polypoid lesion while the aberrant dorsal segment and carina were not involved (Figure 2B). A trans-fissural involvement of the middle lobe was described. Bronchoscopic biopsy disclosed a well-differentiated TC with one mitosis per 2 mm2, absence of necrosis and a Ki67 =3%. Positron emission tomography and whole-body CT scan did not disclose any other lesion. A right upper bronchoplasty bilobectomy was planned (Figure 3). After performing a standard middle lobectomy and closing the aberrant dorsal bronchial segment with a stapler, a bronchial wedge resection of the origin of the true right upper bronchus was performed, preserving the uninvolved pars membranacea of the bronchus intermedius, with free margins at frozen section examination (Figure 4). Airway reconstruction was obtained by suturing with tension–free interrupted stitches between the uninvolved anomalous carina and the bronchus intermedius, above the middle lobe bronchial stump (Figure 5) after extensive subcarinal and paratracheal lymphadenectomy—following azygos vein section—to ensure maximal mobilization of the right tracheobronchial angle. A wide pericardial fat flap was then mobilized and interposed between the anterior aspect of the anastomosis and the posterior wall of the intermediary pulmonary artery to prevent bronchovascular fistula and to cover the bronchial stumps (Figure 6). No major complications occurred in the postoperative period and no clinical problem was recorded at the 30-day follow-up.
Discussion
Since the first bronchial sleeve resection performed by Price Thomas (7), bronchoplasty procedures have gradually gained popularity among thoracic surgeons and are now performed with a wide range of indications, including carcinoids, benign diseases and traumatic lesions (8). Bronchoplasty is mainly indicated for tumors arising at the origin of a lobar bronchus, precluding simple lobectomy but not infiltrating so far as to require pneumonectomy (8).
In the reported case, the anomalous segmentation of the right upper lobe represented a further challenge for radical resection of the carcinoid tumor guaranteeing adequate tumor-free margins while preserving the maximum amount of healthy lung tissue.
A complete sleeve resection from above the healthy aberrant bronchus to the distal part of the bronchus intermedius would probably have resulted in a tension anastomosis because of the considerable amount of bronchial wall resected, potentially culminating in bronchial disruption or significant bronchial size mismatch. For this reason, we planned to close the aberrant bronchus separately and use the uninvolved anomalous carina to insert safe interrupted stitches. At the end of the procedure, the surgical field showed two separate bronchial stumps (anomalous segmental dorsal bronchus and standard middle lobe bronchus) with in between the anastomosis reconstructing the airway.
Two technical aspects of this procedure are of paramount importance. Firstly, an extended lymphadenectomy needs to be accomplished, the R2-R4 stations, not only for oncologic reasons but to ensure maximal mobilization of the right tracheobronchial angle. For this reason, the azygos vein is transected and the region maximally exposed. Secondly, a wide pericardial fat flap is mobilized to protect the stumps and the anastomosis and to separate the bronchial suture from the posterior aspect of the lining artery above. A pericardial fat flap was used not only because it is easy and fast to harvest, but mainly for its reparative properties due to the presence of adipose-derived stem cells (9).
Acknowledgements
The authors thank Anne Prudence Collins for editing the English text.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from both patients for publication of this report and any associated images and videos.
References
- Ramirez RA, Beyer DT, Diebold AE, et al. Prognostic Factors in Typical and Atypical Pulmonary Carcinoids. Ochsner J 2017;17:335-40. [PubMed]
- Detterbeck FC. Management of carcinoid tumors. Ann Thorac Surg 2010;89:998-1005. [Crossref] [PubMed]
- National Comprehensive Cancer Network (NCCN) guideline: Neuroendocrine Tumors, Version 3. 2017 – June 13, 2017. Available online: https://www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf
- Caplin ME, Baudin E, Ferolla P, et al. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol 2015;26:1604-20. [Crossref] [PubMed]
- Erginel B, Ozkan B, Gun Soysal F, et al. Sleeve resection for bronchial carcinoid tumour in two children under six years old. World J Surg Oncol 2016;14:108. [Crossref] [PubMed]
- Petrella F, Mariolo AV, Guarize J, et al. Right upper bronchoplasty bilobectomy. Asvide 2018;5:418. Available online: http:http://www.asvide.com/article/view/24408
- Thomas CP. Conservative resection of the bronchial tree. J R Coll Surg Edinb 1956;1:169-86. [PubMed]
- Venuta F, Rendina EA. Bronchial Sleeve Resections in: ESTS Textbook of Thoracic Surgery Volume 1 Chapter 55.5. Medycyna praktyczna Cracow, 2014:913-21.
- Petrella F, Spaggiari L, Acocella F, et al. Airway fistula closure after stem-cell infusion. N Engl J Med 2015;372:96-7. [Crossref] [PubMed]
Cite this article as: Petrella F, Mariolo AV, Guarize J, Donghi S, Girelli L, Rizzo S, Spaggiari L. Bronchial carcinoid in anomalous right upper bronchus: a “patient-tailored” bronchoplasty resection technique. J Vis Surg 2018;4:81.