Operative techniques for improving surgical exposure in basic cardiac surgery
Introduction
The obesity epidemic has increased worldwide within the past few decades. In 2015, 107.7 million children and 603.7 million adults were obese comprising 5.0% and 12.0% of the global population, respectively (1). In the United States specifically, the National Health and Nutrition Examination Surveys (NHANES) reported the prevalence of obese adults in 1960 to be 12.8% with more recent data from the Centers for Disease Control reporting obesity prevalence at 37.8% in 2014 (2,3). It has been well-established that overweight [body mass index (BMI) >25–29.9 kg/m2] and obesity (BMI >30 kg/m2) increase the morbidity associated with and patient risk of developing multiple health conditions including hypertension, type 2 diabetes, coronary heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnea and respiratory problems and some cancers (2).
From a surgical perspective, overweight and obesity are linked to various comorbidities that implicate risk in surgical intervention. There is a large amount of evidence that obese patients are at increased risk of surgical site wound infections, urinary tract infections, as well as the development of sepsis in trauma patients and delayed graft function in those undergoing renal transplant (4-6).
Post-sternotomy mediastinitis and deep sternal wound infection are devastating complications of cardiac surgery with studies reporting incidence of 0.7–11.1% following standard sternotomy closure (7). Several studies have reported that BMI >30 kg/m2 increases the odds of developing sternal wound infection; in some studies, it has been demonstrated as the only preoperative risk factor for deep sternal wound infection following coronary artery bypass grafting (CABG) (8-10).
Higher BMI in patients undergoing CABG is positively associated with cardiac mortality at 5-years as well as increased likelihood of intensive care unit (ICU) resource utilization including prolonged length of stay, time on ventilator, ICU readmission, and in-hospital death (11,12). The increased risk of infection following cardiac surgery is likely multifactorial due to inadequate dosage of prophylactic antibiotics, difficulty maintaining sterility of tissue folds, and relative poor perfusion of adipose tissue (8). In the face of an aging population amidst an obesity epidemic, cardiac surgeons can expect to see an increasing number of patients with elevated BMI who will not only pose a challenge to manage medically, but also surgically, especially regarding pre- and postoperative planning (8).
In addition to increased risk of perioperative complications, obesity can adversely impact operative exposure and visualization. Even with a normal body mass index (18.5–24.9), anatomic variations in factors such as mediastinal anteroposterior diameter and cardiac chamber dimensions can lead to suboptimal operative exposure. This article discusses techniques that may not be described in traditional textbooks for obtaining improved exposure in basic cardiac operations such as coronary artery bypass grafting and mitral valve operations, for both obese and non-obese patients and including tips for when experienced surgical assistance is limited or absent.
Preoperative preparation
Patients with generous upper body adiposity may be particularly prone to sternal incision complications. When the patient is positioned supine, adipose tissue can shift, resulting in a mis-estimation of the true midline. While this does not generally cause problems with wound healing, it may result in a less than acceptable cosmetic result to the patient. To avoid this, prior to intubation the midline is marked heavily with a non-permanent pen with the patient sitting upright, in a neutral position.
Positioning
Intraoperative maneuvers to improve exposure may involve tilting the table to the right or left. The surgeon should always be alert to the possibility and risk of positional instability. As much as possible, efforts should be made to secure the patient in a manner that is stable to positioning maneuvers. This is particularly challenging in cardiac surgery, as the legs are often prepped and draped into the field for access to the saphenous veins, precluding securement of the lower body.
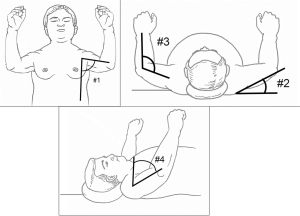
The usual positioning of upper extremities is the tucked position. When patients have a wide lateral thoracic diameter that exceeds the diameter of the bed, the arms may be at risk of falling from the tucked positioned. Use of arm sleds is a solution, but this can increase the distance from the surgeon’s position to the mediastinum, limiting visualization, exposure, and surgeon comfort. Two alternative positioning techniques are available for the upper extremities. First, the arms may be placed in an abducted position on armboards (Figure 1). The second technique is to suspend the arms from upright poles that are secured to the bedrails. This can be done using gauze bandage rolls (Figure 2) or strong silk tape (Figure 3). At our institution, these upright poles are components of a custom-made instrument that supports an instrument tray at the head of the bed. We have used this positioning not only for obese patients but also those with recent hand trauma, hand surgery, or other upper extremity conditions in which development of compartment syndrome may be a concern. No postoperative complications of brachial plexopathy have been observed. Of utmost importance to these alternative positioning techniques is the need to avoid brachial plexopathy (see Role of Team Members).

Procedures
Management of sternotomy and closure
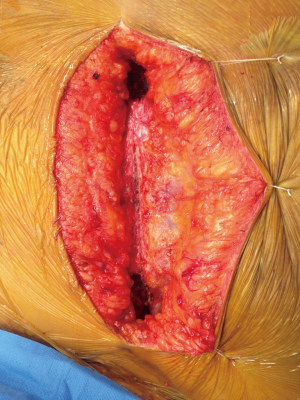
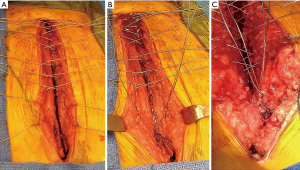
When there is a deep layer of presternal soft tissue, retraction sutures placed through the skin and soft tissue and secured to the lateral chest wall can improve visualization of the sternal bone (Figure 4). This is particularly useful for patients for whom rigid plate fixation is planned. This technique has not resulted in any cosmetic or infectious problems of the chest wall. Caution should be exercised with patients who have mammary implants.
Controversy remains as to the best method of preventing sternal dehiscence in obese patients, and the quality of the sternal bone must also be considered. Obesity may act as a positive predictor of sternal wound infection and dehiscence due to increased weight of soft tissue adding mechanical stress to chest closure. This can prevent union of the sternal halves secondary to increased motion, thus disrupting epithelialization and angiogenesis of soft tissues (9). In patients undergoing median sternotomy followed by wire cerclage closure, obesity (BMI >30 kg/m2) is a known preoperative risk factor for sternal dehiscence and sternal wound infection, most notably, mediastinitis (9,14-16). Molina et al. reported that the incidence of dehiscence rises following wire cerclage as BMI exceeds 30 kg/m2 and can approach 22% as BMI exceeds 49 kg/m2 (17).
The standard closure technique for median sternotomy remains the wire cerclage. Other described methods of closure include the Robiscek technique (18) and rigid plate fixation (19). While Allen et al. reported the method of sternal closure as the only predictor of sternal complications and wound infections, rigid plate fixation has been performed less often than circular wire cerclage due to concerns of drilling near and around the heart, extended operative time, increased expense, and increased time for emergent reentry (7,16). A modification of wire cerclage that redistributes wire tension over a larger area and may reduce the risk of wire fracture is shown in Figure 5.
Dehiscence of the wound is most likely to occur at the inferior portion of the sternotomy incision, where the effect of breasts and abdominal pannus may exert distracting forces. Use of interrupted fascial sutures at the inferior portion, rather than a continuous suture line, is useful in prevention of this complication.
Cannulation
Due to the relatively anterior position of the aorta, exposure of this structure is rarely difficult. The venous structures may be challenging to reach, depending on individual patient anatomy. For example, the right atrial appendage (RAA) may be rotated and in a more posterior position. Retraction of the right ventricle by the surgical assistant may be necessary; however, attention to the hemodynamic effects is critical, and frequent and open communication with the anesthesiologists is paramount to patient safety. Temporary, intermittent cessation of ventilation can aid in exposure. The technique described in Mastery of Cardiac Surgery (20) is safer and easier to perform when an experienced assistance is not available. This involves placing a pursestring on the anterior-most portion of the RAA rather than the lateral wall, thus requiring less manipulation of the heart (Figure 6). A curved clamp is placed at the pursestring suture and the RAA tip excised with scissors. Subsequently, the surgeon is able to control bleeding from the RAA by managing the curved clamp, and the assistant has only to grasp the cut RAA edge and release the clamp to allow insertion of the venous cannula. While not all situations require this technique, consistent use is recommended for operating team familiarity and comfort. We suggest use of a braided suture and placement of the clamp at or above the suture line to avoid inadvertently cutting the pursestring.

Hemodynamic instability may occur during cannulation of the vena cavae due to the required manipulations. Again, temporary cessation of ventilation can assist with exposure, as does retraction of the right pericardium with stay sutures.
Internal mammary harvest
Our retractor of choice for exposure of the internal mammary bed is the Rultract Skyhook system (Rultract Inc., Cleveland, OH, USA). Placement of the retractor arms at the extreme ends of the sternal bone and release of the muscular inferior attachments to the xiphisternum are useful maneuvers. Additional maneuvers for visualization include opening the left pleura widely and drainage of any pleural effusions. The lung can be retracted with a sponge stick, the distal end of which is wedged beneath the hemisternum. This eliminates visual obstruction by the lung without the need for intermittent apnea.
Mitral valve exposure (Figure 7)

Previously described techniques to improve mitral valve exposure include maneuvers that permit the left heart to fall towards the surgeon. These include release of left ventricular adhesions, removal of laparotomy pads behind the left ventricle, and absence of left pericardial retraction sutures. Our preferred method for mitral exposure is the left atriotomy via Waterston’s groove. In over 500 mitral valve surgeries, we have found the need for a trans-septal approach in only one case. The key to excellent visualization with this method is an extended dissection of Waterston’s groove (Figure 7). The limit of dissection is reached when one encounters the fossa ovalis. The atriotomy should be close to this limit. Retraction of the IVC with an umbilical tape retracted at a 45-degree angle, that is, towards the patient’s left hip, also improves exposure by bringing the mitral annulus towards the operative field.
Bleeding from closure of the left atriotomy groove can only be fully assessed after discontinuation of cardiopulmonary bypass, but a full and beating heart may limit visualization of this area. Therefore, a technically sound closure initially is the best method. When an experienced assistant is unavailable to retract the heart, use of the Cosgrove retractor arms in modified positions is useful (Figure 7).
Role of team members
Nursing and surgical technologists
In 2011, the Association of Surgical Technologists developed best practice guidelines for patient positioning (23), which have been summarized as follows:
Surgical position should provide the surgeon optimal visualization and access to the surgical site with minimal physiologic compromise and physical injury to the patient. The surgery team should understand the goals necessary to achieve safe and effective patient positioning; keeping in mind patient comfort, vulnerability, anatomical structures at risk of injury or stress, and access to IV sites and surgical site. Specific patient physiological factors that may affect positioning should be considered during preoperative planning (e.g., age, height, weight, skin integrity, external or internal devices). The surgical department along with the surgical team should have access to surgical equipment (e.g., OR table with appropriate weight recommendations) necessary for optimizing safety and visualization for obese patients.
Special precautions should be considered to avoid pressure ulcer development from surgical positioning. Patients with diabetes, peripheral vascular disease, chronic low blood pressure, increased body temperature, poor nutrition, and those undergoing procedures longer than 3 hours are at increased risk of developing pressure ulcers. Morbidly obese patients should be positioned to achieve maximal patient comfort while also providing adequate surgical site visualization. Skin wrinkling should be smoothed over to avoid vascular compromise and pressure ulcer development. Excessive use of foam or gel positioning devices should be avoided. Special consideration should be given to patients with diabetes or peripheral vascular disease as they are at increased risk of developing ulcers or may have preexisting ulcers.
Surgical team members should be aware of proper technique utilized to position patients as to avoid self-injury. Multiple team members should assist in moving and positioning obese patients. A roller or mechanical lifting device can be utilized for transferring morbidly obese patients from the stretcher to the OR table. Pressure points and bony prominences should be identified and appropriately padded. The patient should be positioned so that no body part extends beyond the OR table or other positioning devices.
When placed in the supine position, patients with cardiorespiratory disease may develop dyspnea, and temporary use of pillows can be beneficial until induction occurs. The most common nerve injuries due to traction or compression include ulnar, brachial plexus, and common peroneal. Care should be taken to appropriately position arms in the anatomical position, abducted no more than 90 degrees with fingers extended. If the procedure requires placement of patient’s arms at the side of the body, it is important to avoid ulnar nerve damage by maintaining slight flexion at elbows, inward facing palms with fingers extended. Draw sheets extending past the elbow should be tucked between the patient and the OR mattress. Ulnar nerve injury occurs secondary to poorly placed arms restraints and table attachments, and poor positioning when placed alongside the patient. Once the patient is properly positioned, surgical team members including the surgeon should assess for optimal safety including proper body alignment, padding, arm placement, and safety strap placement as well as optimal visualization to surgical site before skin prepping occurs.
Anesthesia staff
Patients with obesity present challenges in management to the anesthesia team through both physiologic and anatomic derangements. The first challenge is safely supporting the patient’s respirations via mask ventilation while necessary conditions to establish a definitive airway are achieved. BMI >30, increased neck circumference, and obstructive sleep apnea have all been identified as predictors of difficult mask ventilation combined with difficult laryngoscopy. Thus especially in this patient subset, a variety of supraglottic airways and videolaryngoscopy equipment should be readily available to aid in following the American Society of Anesthesiologists (ASA) difficult airway algorithm (24,25).
Once intubated, patients with obesity pose challenges in mechanical ventilation. Overall these patients have a restrictive lung disease pattern imposed by their chest wall weight as well as decreased functional reserve capacity (FRC). Because of this, their tidal ventilation may dip below the closing volume, leading to collapse of small airways. This causes atelectasis and will severely decrease the tolerance of apneic intervals sometimes needed for optimum exposure. Enhanced vigilance for appropriately applied positive end expiratory pressure is critical to maintain FRC (26).
The anesthesia team must keep several caveats in mind when dealing with the aberrant pharmacokinetics of the obese patient. Obese patients have increased volume of distribution for both lipophilic and water-soluble drugs. The increase in water soluble Vd is not in proportion to total body weight. Obese patients tend also to have higher cardiac outputs and increased renal blood flow and GFR, which alone would both lend themselves to increased clearances. Comorbidities such as hypertension (decreased circulatory blood volume), diabetes mellitus type II (decreased renal function) and fatty liver disease (decreased hepatic metabolism) are other confounding factors. In general, the best approach remains to use a balanced anesthetic that avoids overuse of lipophilic agents.
The pre-incision preparations of the surgeon, surgical technologist, OR nurse, and anesthesiologist come to a common focal point when it comes the positioning of the patient. All should have the goal of patient safety and minimizing iatrogenic injury while gaining optimal surgical exposure in the forefront of their minds. One structure particularly vulnerable to injury is the brachial plexus, due to its fixed origin in the vertebral nerve roots and its route passing in-between structures manipulated during sternal exposure (1st rib and clavicle). Brachial plexus injury during cardiac surgery has a highly variable reported incidence, varying from 1.5–24% percent, with the patients requiring an IMA conduit falling in the higher end of that range. Methods to reduce this injury revolve around appropriate positioning of the patient. The “Hands Up” position is an important tool to balance the risk of brachial plexus injury while still optimizing exposure. The arms being moved away from the patient’s side to the “Hands Up” position is especially a boon for sternal exposure in obese patients as it obviates the need for sleds for arm support. This allows the surgeon a more ergonomic and optimum operating view, decreasing the need for excessive retraction. A series of studies has validated the safety of this position. Vader Salm et al. reviewed 180 patients for post-operative brachial neuropathy and found no difference between arms by side versus arms abducted to 90 degrees (27). Jellish et al. found that “hands up” positioning was associated with less SSEP amplitude decreases but no clinical differences in injury between “hands up” positioning versus arms by side (28). A traditional “Hands Up” approach is described as arms abducted no more than 90 degrees and elbows elevated above the horizontal plane with wedges by the patient’s head. This is often difficult and space-consuming, reducing access to the airway, central lines and TEE probe. Using the same principles, a modified “Hands Up” position can be used by suspending the patient’s arms on an attachment using egg carton foam padding. Several angles need to be considered as illustrated in Figure 8. First, the arms should be abducted less than 90 degrees. Second, the arms should be suspended slightly above the plain of the thoracic outlet. The upper arm should meet at a nonacute angle with forearm. Finally, the humeral head should remain at less than 90 degrees rotation cephalad.
Postoperative management
Obese patients present a general anesthetic challenge due to their various comorbidities and physiologic changes in respiratory homeostasis. The increased risk of the obese patient to develop pneumonia and venous thromboembolism can complicate postoperative management and recovery. Early mobilization, pulmonary toilet, and pain control are key elements and require a multidisciplinary approach including nursing, respiratory, and physiotherapy staff.
For women, routine use of brassieres placed in the operating room and continued into the postoperative period is recommended. Alternatively, an adjustable abdominal binder may be more comfortable for some patients.
Conclusions
Cardiac surgical teams must consider the risks associated with the obese patient population undergoing cardiac surgery procedures and employ techniques pre-, intra-, and postoperatively in a multidisciplinary fashion. Safe and efficacious techniques are paramount to optimal patient outcomes.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained for publication of this case report and any accompanying images.
References
- GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13-27.
- NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Obes Res 1998.51S-209S.
- National Center for Health Statistics. Health, United States, 2016: With chartbook on Long-term trends in health. Hyattsville, MD. 2017.
- Khwaja A, El-Nahas M. Transplantation in the obese: separating myth from reality. Nephrol Dial Transplant 2012;27:3732-5. [Crossref] [PubMed]
- Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg 2009;250:166-72. [Crossref] [PubMed]
- Quante M, Dietrich A, Elkhal A, et al. Obesity-related immune responses and their impact on surgical outcomes. Int J Obes (Lond) 2015;39:877-83. [Crossref] [PubMed]
- Allen KB, Thourani VH, Naka Y, et al. Randomized, multicenter trial comparing sternotomy closure with rigid plate fixation to wire cerclage. J Thorac Cardiovasc Surg 2017;153:888-96.e1. [Crossref] [PubMed]
- Fowler VG Jr, O’Brien SM, Muhlbaier LH, et al. Clinical predictors of major infections after cardiac surgery. Circulation 2005;112:I358-65. [PubMed]
- Fu RH, Weinstein AL, Chang MM, et al. Risk factors of infected sternal wounds versus sterile wound dehiscence. J Surg Res 2016;200:400-7. [Crossref] [PubMed]
- The Parisian Mediastinitis Study Group. Risk factors for deep sternal wound infection after sternotomy: A prospective, multicenter study. J Thorac Cardiovasc Surg 1996;111:1200-7. [Crossref] [PubMed]
- Gurm HS, Whitlow PL, Kip KE, et al. The impact of body mass index on short- and long-term outcomes in patients undergoing coronary revascularization: insights from the bypass angioplasty revascularization investigation (BARI). J Am Coll Cardiol 2002;39:834-40. [Crossref] [PubMed]
- Rosvall BR, Forgie K, MacLeod JB, et al. Impact of obesity on intensive care unit resource utilization after cardiac operations. Ann Thorac Surg 2017;104:2009-15. [Crossref] [PubMed]
- Hui DS, Lizalek JM, Chawa VS, et al. Arm suspension technique using gauze rolls. Asvide 2018;5:415. Available online: http://www.asvide.com/article/view/24405
- Olbrecht VA, Barreiro CJ, Bonde PN, et al. Clinical Outcomes of Noninfectious Sternal Dehiscence After Median Sternotomy. Ann Thorac Surg 2006;82:902-7. [Crossref] [PubMed]
- Katz NM. Pericostal sutures to reinforce sternal closure after cardiac surgery. J Card Surg 1997;12:277-81. [Crossref] [PubMed]
- Song DH, Lohman RF, Renucci JD, et al. Primary sternal plating in high-risk patients prevents mediastinitis. Eur J Cardiothorac Surg 2004;26:367-72. [Crossref] [PubMed]
- Molina JE, Lew RS, Hyland KJ. Postoperative sternal dehiscence in obese patients: Incidence and prevention. Ann Thorac Surg 2004;78:912-7. [Crossref] [PubMed]
- Goh SSC. Post-sternotomy mediastinitis in the modern era. J Card Surg 2017;32:556-66. [Crossref] [PubMed]
- Raman J, Straus D, Song DH. Rigid plate fixation of the sternum. Ann Thorac Surg 2007;84:1056-8. [Crossref] [PubMed]
- Crosby IK, Zacour RK. Cardiopulmonary Bypass. In: Kaiser LR, Kron IL, Spray TL, editors. Mastery of Cardiac Surgery 3rd Edition, Philadelphia: Lippincott Williams & Wilkins, 2013:361-2.
- Hui DS, Lizalek JM, Chawa VS, et al. Techniques for internal mammary artery harvesting exposure. Asvide 2018;5:416. Available online: http://www.asvide.com/article/view/24406
- Hui DS, Lizalek JM, Chawa VS, et al. Techniques for mitral exposure and left atriotomy closure. Asvide 2018;5:417. Available online: http://www.asvide.com/article/view/24407
- AST Education and Professional Standards Committee. AST standards of practice for surgical positioning. AST [Published 1 April 2011, accessed 25 February 2018].
- Kheterpal S, Healy D, Aziz MF, et al. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group. Anesthesiology 2013;119:1360-9. [Crossref] [PubMed]
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology 2013;118:251-70. [Crossref] [PubMed]
- Chacon MM, Cheruku SR, Neuburger PJ, et al. Perioperative care of the obese cardiac surgical patient. J Cardiothorac Vasc Anesth 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Vander Salm TJ, Cereda JM, Cutler BS. Brachial plexus injury after median sternotomy. J Thorac Cardiovasc Surg 1980;80:447-52. [PubMed]
- Jellish WS, Blakeman B, War P, et al. Hands-up positioning during asymmetric sternal retraction for internal mammary artery harvest: a possible method to reduce brachial plexus injury. Anesth Analg 1997;84:260-5. [Crossref] [PubMed]
Cite this article as: Hui DS, Lizalek JM, Chawa VS, Lee R. Operative techniques for improving surgical exposure in basic cardiac surgery. J Vis Surg 2018;4:80.