Uniportal video-assisted thoracic surgery treatment of intra-operative complications
Introduction
The first principle in addressing intra-operative complications, in surgery and particularly in uniportal video assisted thoracic surgery, is prevention.
Hence, prevention is supported by understanding the anatomic challenges of the individual case, study pre-operative images, discuss each patient in a multi-disciplinary team meeting, select appropriately and plan carefully each case which merits a uniportal approach.
Nevertheless, complications are still part of the operation; the surgeon should be prepared to identify them early and treat them adequately.
The authors aim to analyse the following factors as shown in Table 1, to help the reader to avoid and treat intraoperative complications.
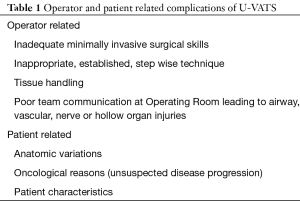
Full table
Operator related factors influencing complications
Minimally invasive and uniportal approach skills
Every surgeon needs to recognise own limitations, more than strengths. A skillful traditional 3–4 port VATS surgeon is not necessarily equally capable in uniportal approach.
Education in uniportal VATS surgery should encompass:
- A team learning approach including Anaesthetist, assistants and scrub nurses;
- Attendance at an accredited uniportal video-assisted thoracic surgery (U-VATS) Institution with good experience followed by;
- Production of standard Operating Procedures and Protocols at Home Institution;
- Provision of appropriate equipment and;
- Proctorship to safeguard a comfortable learning curve (1).
U-VATS technique
Access through a single incision renders the technique unique in multitasking. Most surgeons are able to handle more than one instrument on a single hand.
- It is not uncommon that U-VATS requires the surgeon to address 3–4 instruments simultaneously (2).
- Frequently the 0 or 30-degree camera (in U-VATS lobectomy, segmentectomy and pneumonectomy) is on the “roof” of the incision.
- A suture around the camera, in a loop fashion, anchored at the posterior aspect of the skin incision maintains a stable position of the camera and helps the assistant.
- It should be noted that often it is difficult to assist a lengthy U-VATS major lung resection, as the position of the camera requires hyperextension of the assistant’s shoulder and forearm holding the camera in an anti-gravitational direction.
Tissue manipulation
Contrary to the multi-port VATS operations, U-VATS does not allow multiple angulations of the different endoscopic instruments. All instruments are pointing towards the anatomical structures from a similar direction in a way that often vessels or airways might not be presented at a favourable, familiar angle to the instruments.
- On these occasions the operator needs to present the anatomical structure to the instrument, by retracting and manipulating lung tissue.
- Reckless and excessive manipulation of the lung, does lead to microtrauma of the parenchyma. Apart from the risk of an annoying postoperative air leak (3), more importantly the injury of the lung tissue can affect the lymphatic and venous drainage; acute lung injury or adult respiratory distress syndrome have been reported (4);
- Injury to the distal bronchioles is contributing to postoperative atelectasis.
- Dedicated U-VATS instruments (elongated with various angulations) have been developed particularly for the above-mentioned reasons. The elegance of gentle tissue manipulation cannot be emphasized enough to prevent complications.
Appropriate pre-operative planning of each case
- Correct studying and interpretation of pre-operative imaging is mandatory.
- A dedicated discussion with a thoracic radiologist is a routine practice in our institution.
- A contrast CT scan remains the gold-standard imaging to identify the vessels and airways in need of attention, their relationship and any anatomical variations necessitating the presence of all appropriate equipment, skill mix and team preparation.
- An inviting operating field at U-VATS is of paramount importance and such can only be presented by an appropriate Thoracic Anaesthetist. His presence in U-VATS is not desirable but mandatory.
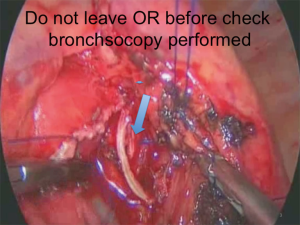
Management of intraoperative airway complications
Airway injuries at VATS are very unusual but once they occur the consequences can be disastrous and lead to unacceptable and high morbidity. Injuries range from simple perforations as a result of extensive manipulation, tissue or instrument failure at stapling line with stump leaks to stapling and transection of the wrong bronchus (Figures 1,2).

The authors have provided a comprehensive table to manage airway injuries (Table 2).

Full table
In the unfortunate event of transection of the wrong bronchus, early identification and re-establishment of the anatomy is of paramount importance.
In general:
- Air leaks should be addressed to avoid prolonged hospital stay and risks of pleural infection with all catastrophic sequel for patients and Health Care Systems.
- Tissue is always favourable in buttressing airway injuries rather than commercially available sealants and ‘plugs’.
- The authors would also encourage any surgeon in doubt, to convert to a multi portal VATS or open thoracotomy in case of concern. What matters most is the successful outcome and not the obsession to complete with one port.
- There is enough evidence in the medical literature to suggest that a primary repair, with or without a flap reduces significantly the incidence of bronchopleural fistula and empyema, compared to a delayed repair, once an intrapleural infection has been established.
Management of intraoperative bleeding
This remains the main concern shared by all surgical fraternity.
Pulmonary artery bleeding (Figures 3,4)


General comments:
- The pulmonary artery (PA) and its branches, unless the patient has established pulmonary hypertension, are part of a low-pressure system. The PA-related bleedings can be controlled by applied gentle pressure.
- The classic “swab on a stick” (small gauze wrapped in a Rampley sponge holding forceps) is adequate to control most PA bleeds. This should be available and ready for use in all procedures. We advise constant gentle pressure for at least 5 consecutive minutes, prior to re-evaluation of the injury. During this period a full team brief is established with a plan. Long vascular clamps, vascular tapes and fine sutures should be available as well as haemostatic patches.
- The first main task is to assess the injury by asking the following questions:
- Type of injury, i.e., minor bleed on a vessel, moderate wall dissection with haematoma formation, full large thickness split of a PA branch or main shaft.
- Extent of injury and topography, i.e., small branch, lobar branch, main PA.
- Extent of prior dissection and ability to get proximal and distal control as well as encircle safely the vessel.
A suggested algorithm for management of PA bleeds is shown in Table 3.
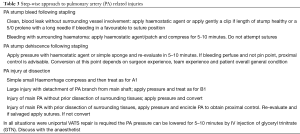
Full table
Pulmonary veins (PV)
The PV and their tributaries, can tolerate more handling compared to their artery counterparts.
General comments:
- The same principles of repair apply as in the previous paragraph with arterial bleeds.
- It’s advisable to allow adequate vein stump when stapling the pulmonary veins (photo). In this manner any bleeds can be addressed with proximal control and sutures.
- PV bleeding close to pericardium raises concern as the left atrium is in close proximity and has a thin muscular wall.
- If such situation is suspected the pericardium should be opened without disturbing the stapling line and proximal control applied before any attempt to suture is commenced.
Other uncommon intra operative bleeding
- The subclavian vessels can be traumatised not only in operations of the superior sulcus, but in bullectomies or lung volume reduction surgery (LVRS) because of frequent presence of vascular adhesions to the area. It may become challenging to visualise the area of bleeding with the uniportal approach. Compression is the first step, but large tears can only be managed with conversion and appropriate vascular control. In desperate situations ligation of the vessel might prove life-saving.
- Blood flow to the upper limb can be re-established with vertebral or carotid to distal subclavian by-pass and in some environments the assistance of the vascular team will be necessary.
- The internal thoracic vein and artery might be injured during dissection of an anterior lesion or detachment of an adherent lung area. In case of injury compression followed by simple ligation of the vessels with sutures is enough to arrest the bleed.
- Caution should be applied in cases of a U-VATS approach where the patient has received a prior CABG with internal mammary artery dissection and anastomosis. Quite often the lung is adherent in the grove between the anterior chest wall and the pericardium. A bleed can be avoided if an extremely adherent lung gets detached by the use of staplers. The retained lung tissue on the chest wall has enough vascular supply and will not necrose. Adventurous dissection in this area can cause a serious bleed. In this situation conversion will be necessary and on the balance of probabilities, if the arterial graft is lost the patient will require assistance from a Cardiac Surgeon to address the internal mammary artery conduit injury.
- Intra operative bleeds from an azygos vein injury are managed easily either by simple suturing or stapling of the vessel.
- Similar bleeds from the superior vena cava should be addressed with initial pressure. Small injuries can be sutured, although bigger injuries will require control with a vascular clamp. Please note that in the presence of a central line:
- The vascular clamp might not arrest the bleeding completely and
- Special care should be taken to avoid incorporating the central line within the repaired injury by the suture line.
Management of intraoperative diaphragmatic injuries
Diaphragmatic perforations can result from an inadequately paralysed patient or inappropriate port incision placement in cases of pleural sepsis was the diaphragm can be in an unusually high position.
It is advised in such pathology to perform an intra-operative ultrasound scan of the chest which marks the correct position of the diaphragm.
Diaphragmatic injuries can be simply repaired with sutures and no conversion is necessary. The surgeon should always take care to avoid abdominal organ injury during repair.
Management of intraoperative esophageal injuries
The oesophagus can be potentially injured in both pleural cavities. The most frequent injuries occur during dissection of the sub carinal nodes.
It is recommended that diathermy should be used with caution in the vicinity of the esophageal lumen. Any minor bleeding can be attended with simple packing for a few minutes and conscious use of haemostatic agents.
In cases were identification of the esophagus is challenging an oesophageal bougie or nasogastric tube should be inserted to facilitate recognition.
Esophageal perforations need primary repair, preferably with 2 layers of sutures and an adjoining viable tissue flap to prevent subsequent leak and pleural sepsis.
Management of intraoperative thoracic duct injuries
The thoracic duct can be traumatised while sampling stations R9 and 8. Prevention is of paramount importance as such injuries become evident during the post-operative period.
Our recommendation is aggressive management with fat free diet and if the leak continues ligation of the duct without delay.
Patient related factors influencing complications
Extra care should be paid by the surgeon to identify those patient-related factors which can lead to intraoperative complications.
Anatomical variations
There are several recognised anatomical variations of the hilar anatomy (7). Such, dictate surgical approach and require pre-operative identification and understanding. We cannot emphasize enough the need to obtain appropriate imaging studies, discuss them with a dedicated radiologist and have these available in the operating room for consultation.
Disease progression
International guidelines dictate that no patient with lung cancer should undergo an operation with CT images older than 4 weeks from the date of surgery (8). The importance of a recent CT is multifaceted as (I) it provides accurate staging; (II) allows appropriate surgical planning, type of access and position of uniportal incision; and (III) guides the surgeon safely around the hilar structures preventing complications
Patient characteristics
These provide important pivot points to prepare and prevent intra operative complications.
- The chest wall contour dictates the position and size of the uniportal incision in combination with the intended procedure in a severely kyphotic or scoliotic patient.
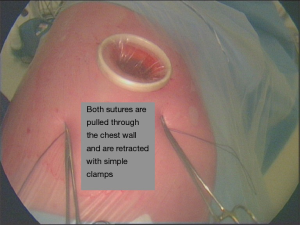
- The access and instrument selection is influenced by the presence of a severely emphysematous lung with minimum deflation or a severely obese patient with high hemi diaphragm and generous hilar fat. Loss of the operating field can be compensated by traction sutures to the diaphragm in order to increase the volume of the pleural cavity (Figures 5,6).
- Similar concerns apply to a patient with significant pulmonary hypertension where a full hilar dissection is necessary.

Discussion
U-VATS approach brings new challenges. We feel the need to repeat that the uniportal surgery is not a variation of the multi-portal one. It requires specific skills, instruments and team mentality to succeed; equally it will present its own patient related challenges.
Nowadays, the VATS approach is dominating. In our institution, Leeds Teaching Hospitals, we have reported VATS lobectomies compared to open approach up to 100% in certain months, while our average is well above 75%. Within the European Society of Thoracic Surgeons (ESTS) database (10) of approximately 40,000 lobectomies, in the last 5 years the VATS percentage in lobectomies alone is 31.9; this same percentage was only 5.3, just 5 years earlier.
In other words, it required a decade for the dedicated thoracic surgeon to change the surgical practice and increase to six-fold the percentage of VATS lobectomies.
At present, the ESTS Silverbook has no data on whether the VATS approach includes the uniportal procedure.
Undoubtedly, the uniportal approach needs time before it increases to large percentages at an international level. The involved surgeons ought to share their experience.
Conclusions
We presented several factors that can help and improve the understanding and safety of the U-VATS procedure. The differentiation of the contributing factors in operator and patient-related can help to have a better insight on the new adaptations that are required in the future.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: All participants gave informed consent before taking part in this study.
References
- Bedetti B, Bertolaccini L, Solli P, et al. Learning curve and established phase for uniportal VATS lobectomies: the Papworth experience. J Thorac Dis 2017;9:138-42. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Tsunezuka Y, Shimizu Y, Tanaka N, et al. Video-assisted thoracoscopic lobectomy for lung cancer patients with severe incomplete fissures or emphysema; intralobar no-touch access technique (INTACT). Kyobu Geka 2007;60:202-6. [PubMed]
- Jin Z, Chun Suen K, Ma D. Perioperative "remote" acute lung injury: recent update. J Biomed Res 2017;31:197-212. [PubMed]
- Tentzeris V, Papagiannopoulos K. Main bronchus stapling line leak and suturing. Asvide 2018;5:397. Available online: http://www.asvide.com/article/view/24314
- Tentzeris V, Papagiannopoulos K. Left pa dissection following manipulation. Asvide 2018;5:398. Available online: http://www.asvide.com/article/view/24315
- Bergman RA, Afifi AK, Miyauchi R. Introduction to the Series. Illustrated Encyclopedia of Human Anatomic Variation. Available online: www.anatomyatlases.org
- Lim E, Baldwin D, Beckles M, et al. Guidelines on the radical management of patients with lung cancer. Thorax 2010;65 Suppl 3:iii1-27. [Crossref] [PubMed]
- Tentzeris V, Papagiannopoulos K. Diaphragmatic retraction. Asvide 2018;5:399. Available online: http://www.asvide.com/article/view/24316
- ESTS Silverbook, Database annual report 2017, 31. Available online: http://www.ests.org/collaboration/database_reports.aspx
Cite this article as: Tentzeris V, Papagiannopoulos K. Uniportal video-assisted thoracic surgery treatment of intra-operative complications. J Vis Surg 2018;4:74.


