Commissural repositioning in bicuspid aortic valve repair with Valsalva graft
Bicuspid aortic valve (BAV) is the most common congenital cardiac defect, with an estimated prevalence between 0.5% and 2% (1); this pathology is often associated with aortic root and ascending aorta dilation due to structural abnormalities such as decreased fibrillin, elastin fragmentation and apoptosis (1,2). BAV typically consists of two unequal-sized leaflets, with the larger one presenting a central raphe or ridge resulting from the fusion of the commissures (type 1 of Sievers classification) (3). BAV morphologic conformations vary according to the fused commissures, with the most common pattern involving fusion of right and left cusps (2).
In childhood, aortic stenosis can develop due to a small valve orifice size while pure aortic incompetence can be secondary to a prolapsing leaflet (1,4). During adulthood, the abnormal shear stress can lead to valve calcification and/or further aortic root dilation (1,4).
In case of ascending aorta and root dilation, early elective surgery is currently accepted, according to the recent guidelines, in order to reduce the risk of aortic dissection (5,6). In presence of good quality aortic leaflets, a valve sparing operation is a practicable and very attractive option, especially to avoid prosthesis-associated complication (7,8).
In our center, we have quite an extensive experience with this kind of procedures. In the last years, a lot of studies highlighted that commissural orientation <160° in BAV can be considered one of the principal risk factors for recurrent aortic insufficiency (9,10). Basing on this evidence, we started repairing these subtypes of valve aiming, when possible, at the 180°–180° geometric configuration, both in case of isolated valve repair and also when sparing surgery is required. In particular, we tried to obtain this symmetric orientation every time the non-fused cusp occupied at least 160° of the annulus perimeter and of the global cusp surface area. In our center, in presence of BAV with ascending aorta and root dilation, at the current time our systematic approach consists of reimplantation procedure with 180°–180° geometric configuration associated to aortic leaflets repair.
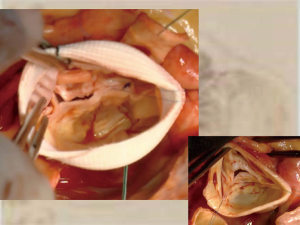
The surgical approach has always been full sternotomy; after cardiopulmonary institution, aortic cross-clamping and diastolic cardiac arrest with Custodiol solution antegrade infusion, we perform a transverse aortotomy above the level of the sinotubular junction to analyze the aortic valve and root in order to choose the adequate repair procedure. To obtain a better valve exposure, we put 4-0 polyester tractional sutures in correspondence of the commissures, paying attention not to distort leaflet due to inadequate traction. After testing the aortic leaflets good quality, fundamental assumption for a sparing surgery, we started the first part of the repair procedure with the native aortic root intact. In most cases, it consists of raphe resection with the aim of improving cusp mobility and of reducing the connection between the raphe and the fused commissure. In presence of fibrotic raphe, shaving can be enough to excise the thickened portion of the leaflet and to restore a normal motion; when a very calcific or fibrotic raphe is hampering the cusp motion, a complete excision followed by direct suture can be necessary; only rarely we need to perform a pericardial patch repair. Shaving can be required also at the level of the free margin. After that, we checked for the presence of any prolapse with the help of both a central stitch passed through the Aranzius nodules and of the Schafers Calliper. If any prolapse is detected, we eventually fix it by means of a plicature performed in the prolapsing portion of the leaflet with the aim of raising the pathological part to obtain a good coaptation height and length. At this moment, the procedure continues with the traditional preparation for the reimplantation procedure, with the dissection of the aortic root as low as possible, detaching and mobilizing the coronary ostia and removing the aortic sinuses. Then we proceed with the placement of the 2-0 braided non-absorbable pledgeted stitches at the proximal suture line at the level of the horizontal plane formed by the base of the interleaflet triangles and the nadir of the leaflets insertion line in the aortic root. These sutures are passed from inside to outside the aorta, with the pledgets internally forming a ring at the level of the virtual basal ring, and then they are reported at the bottom of the vascular graft chosen (Valsalva graft in the majority of the cases, Hemashield in the remaining). The commissural traction sutures are then pulled inside the vascular graft, in order to keep the two commissure well detected and then the basal sutures are tied up. At this point we can start the valve resuspension within the graft: first of all the two commissures are fixed in a 180°–180° symmetric configuration within the neo-root to the new predetermined sinotubular junction (see Figure 1); finally, the scalloped profile of the aortic valve is sutured to the prosthesis with 4-0 polypropylene sutures in the conventional fashion. After completion of the root reimplantation, the valve is re-assessed in order to correct any residual prolapse, generally again with free margin plicature. In the end, the procedure is completed with coronary ostia repositioning in the neo-root and distal anastomosis of the vascular graft.
Intra-operative trans-esophageal echocardiogram is mandatory for the immediate evaluation of the aortic procedure; pre-discharge trans-thoracic echo has always to be performed to check the immediate stability of the surgical result.
We have adopted this kind of procedure for a few years now and at the current time we have performed it in a good number of patients, so we are quite confident with this technique. From our point of view, the advantages offered by this approach are remarkable. First of all, the fact of reproducing a symmetric tridimensional configuration with two balanced opposed leaflets, simplifies considerably the repair procedure since we have to reassess only two surfaces, comparable for dimensions and extension, in order to obtain the same coaptation height and to guarantee an adequate coaptation length, in absence of prolapses and/or retractions. Secondarily, with this kind of configuration we obtain an optimization of the effective orifice area since the removal of the leaflet fibrotic raphe ensures better motility and the 180°–180° situation allows a good valve opening, with no risk of stenosis. Moreover, in all cases we performed, the post-operative aortic gradient always resulted very low, confirming the poor possibility of valve stenosis. Finally, the fact that the new simplified tridimensional configuration is stabilized inside the chosen vascular graft, involving all the components of the aortic root functional unit, should guarantee long term durability of the surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol 2010;55:2789-800. [Crossref] [PubMed]
- Verma S, Siu SC. Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med 2014;370:1920-9. [Crossref] [PubMed]
- Sievers HH, Schmidtke C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg 2007;133:1226-33. [Crossref] [PubMed]
- Bonow RO, Carabello BA, Chatterjee K, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing Committee to Revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol 2006;48:e1-148. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2438-88. [Crossref] [PubMed]
- Falk V, Baumgartner H, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg 2017;52:616-64. [Crossref] [PubMed]
- de Kerchove L, Boodhwani M, Glineur D, et al. Valve sparing-root replacement with the reimplantation technique to increase the durability of bicuspid aortic valve repair. J Thorac Cardiovasc Surg 2011;142:1430-8. [Crossref] [PubMed]
- Bavaria JE, Desai N, Szeto WY, et al. Valve-sparing root reimplantation and leaflet repair in a bicuspid aortic valve: comparison with the 3-cusp David procedure. J Thorac Cardiovasc Surg 2015;149:S22-8. [Crossref] [PubMed]
- Aicher D, Kunihara T, Abou Issa O, et al. Valve configuration determines long-term results after repair of the bicuspid aortic valve. Circulation 2011;123:178-85. [Crossref] [PubMed]
- Fattouch K, Moscarelli M, Castrovinci S, et al. Mid-term results of bicuspid aortic valve repair guided by morphology and function assessment. Interact Cardiovasc Thorac Surg 2017;25:83-8. [Crossref] [PubMed]
Cite this article as: Contino M, Mangini A, Romagnoni C, Antona C. Commissural repositioning in bicuspid aortic valve repair with Valsalva graft. J Vis Surg 2018;4:70.


