Hybrid thoracoabdominal aortic aneurysm repair: is the future here?
Introduction
Despite significant advances in surgical techniques, perioperative adjuncts, and critical care, open thoracoabdominal aortic aneurysm (TAAA) repair remains a surgical challenge. In our series of 3,309 TAAA repairs, we reported an overall operative mortality rate of 8% and a 30-day mortality rate of 5%; key complication rates ranged from 1% to 6% (1). The traditional morbidities associated with open TAAA repair include paraplegia, paraparesis, renal failure necessitating dialysis, stroke, and intestinal ischemia, most of which are related to distal aortic ischemia (2). The risk of postoperative death or complications is increased in the most extensive TAAA repair (Crawford extent II TAAA repair). This repair typically involves replacing the aorta from just distal to the left subclavian artery to the aortic bifurcation. The risk is also increased in certain patient populations, such as older patients and those with congestive heart failure, poor pulmonary function, or renal disease (3-7). Because of the added operative risk in patients with these comorbidities, less invasive techniques have been developed (8-11). These alternative techniques include either a total endovascular approach or a combined open and endovascular “hybrid” approach to TAAA repair. The decision on which approach to use for TAAA repair—conventional open, endovascular, or hybrid—should be based on a clear understanding of the risks of each one as well as the individual needs of the patient.
Unlike with coronary artery bypass graft procedures or abdominal aortic aneurysm repairs (12-14), no well-established risk models specifically address the risk reserved for “high-risk” patients, and the decision is commonly left to the clinician’s discretion (15,16). Algorithms have been developed to assist with decision pathways for hybrid versus open aortic repair in some centers. Benrashid and colleagues (17) identified being frail or over 65 years old or having coronary artery disease, valvular heart disease, congestive heart failure, chronic obstructive pulmonary disease, renal insufficiency, or previous open distal aortic repair as markers for high-risk repair. At our center, we recently reviewed whether female sex or distal aortic reoperation affected postoperative outcomes after TAAA repair and found no significant effect of either variable on early outcomes (18,19). Further research is needed to identify preoperative characteristics that are predictive of increased risk.
Alternative approaches to open TAAA repair
Hybrid TAAA repair
Combined open and endovascular hybrid TAAA repair generally involves 1 or 2 stages. In this approach, the visceral and renal arteries (namely, the celiac axis, superior mesentery, left renal, and right renal arteries) are rerouted by “debranching” the vessels with 8- or 10-mm bypass grafts with aortic reattachment sites above or below the proposed endovascular zone; the repair is followed by endovascular exclusion of the aneurysm, which then covers the vessel origins (20). The hybrid procedure, originally introduced in 1999 by Quinones-Baldrich and colleagues (21), was intended to be an improvement over traditional open TAAA repair because its use avoided aortic cross-clamping, thoracotomy, single-lung ventilation, and prolonged ischemia. In theory, this approach was a better option for patients who were considered poor candidates for open surgical repair.
However, in practice, the early hybrid TAAA experience was fraught with difficulty. The substantial morbidity and mortality after hybrid TAAA (6) repair led many centers to reserve it primarily for inoperable patients (22,23). In 2012, Moulakakis and colleagues (24) published a meta-analysis of outcomes of 528 hybrid TAAA repairs from 14 studies; they found a substantial mortality rate of 14.3% and a complication rate of 7.0% for spinal cord ischemia, 4.5% for mesenteric ischemia, and 7.0% for permanent renal failure (Table 1). Mesenteric ischemia after hybrid TAAA repair is a concern and may range from 17% to 40% (6,23). Chiesa and colleagues (25) reported that severe angulation of the superior mesenteric artery bypass graft is predictive of these ischemic complications.

Full table
Because of these findings, as well as an interest in “staged repair” concepts introduced by Griepp and others (26), newer hybrid techniques have been developed. Contemporary hybrid TAAA repairs often involve first performing a less extensive open TAAA repair (i.e., a Crawford extent III or IV TAAA repair) to reimplant the visceral arteries onto a short section of aortic replacement graft, rather than using a debranching approach with relatively long segments of bypass grafts; the repair is then extended with a stent graft or vice versa, in which at least one endovascular landing zone is a synthetic graft (27). This operation is completed in two stages (separated by days, weeks, or months), which appears to reduce major adverse effects (e.g., renal failure, spinal cord deficit, and operative death) as compared to older methods of hybrid TAAA repair that necessitate debranching the visceral arteries (11,27,28). However, despite these preliminary positive outcomes, staged hybrid repairs are performed at an increased cost—nearly twice that of traditional open TAAA repair (7).
Total endovascular TAAA repair
As advancements in hybrid repair were being made, the development of total endovascular TAAA repair procedures progressed as well, and in recent years, the procedure has been simplified and delivered with high technical success (9). Entirely endovascular approaches to TAAA repair range from the use of bespoke devices with fenestrations or branches to accommodate the visceral arteries (most custom-made devices have a 6-week manufacturing delay) to the use of ad-hoc approaches incorporating a combination of available endovascular devices in an off-label fashion (e.g., parallel, snorkel, telescope, and chimney approaches). Each purely endovascular approach has a sharp learning curve, and early on in their development, many had considerable mortality and morbidity. A remaining concern is the potential for developing a spinal cord deficit after extensive (Crawford extent II) endovascular TAAA repair (29). However, in most contemporary series of endovascular TAAA repairs, few complications are reported (9,10,30,31). Nevertheless, the Achilles’ heel of total endovascular approaches is the relatively frequent need for secondary reintervention (31), which necessitates continued postoperative surveillance. Additionally, it is unclear whether endovascular TAAA repair can be used in all patients, such as those with highly complex anatomy or those with mycotic aneurysm. For example, patients with advanced age, who in theory are the most likely to benefit from this approach, are also more likely to present emergently with aortic rupture, and until very recently, the need for emergent repair prohibited the use of custom-manufactured branched and fenestrated devices. However, Wolosker and colleagues (32) recently reported the successful emergent use of an off-the-shelf branched device to treat a patient with aortic rupture. Table 2 shows the relative advantages and disadvantages of hybrid TAAA repair compared to endovascular TAAA repair.
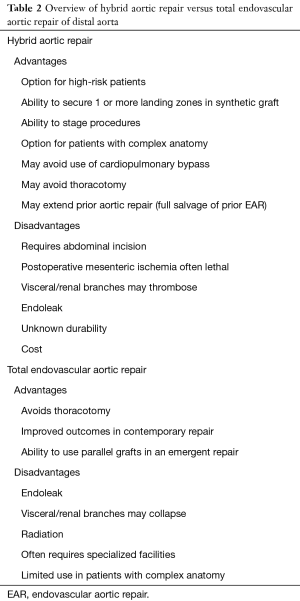
Full table
Open repair after endovascular aortic repair (EAR)
Over the last 2 decades, while complex hybrid and endovascular approaches were being developed and refined, the rates of standard descending thoracic and abdominal EAR increased dramatically, despite related complications and unknown durability associated with this treatment. The decision to perform conventional open TAAA repair after endovascular treatment is not straightforward, and additional endovascular repair is typically performed first in an attempt to address complications. However, the conversion to open repair is often warranted in the case of serious complications, such as fistula, infection of the stent-graft, retrograde type A dissection, device collapse or migration, and some types of endoleak (i.e., types Ia and Ib) or continued aneurysmal expansion (Figure 1) (33,34). As the number of patients treated with EAR increases, the number of patients that will need an open repair after endovascular repair is expected to also increase.
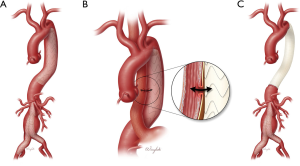
From 1996 through 2017, 159 patients with previous EAR underwent an open or endovascular reintervention at our major quaternary referral aortic center. Of these repairs, 22 (14%) involved the full salvage of the deployed stent-graft, which was incorporated into an adjacent open repair. Partial or complete extraction of the stent graft was performed in 90 patients, and for these patients, the rates of early operative death, permanent stroke, and renal failure were 8%, 1%, and 3%, respectively. However, the postoperative risk increases greatly in patients who undergo highly complex open conversion repairs, such as cases of infection or fistula. Melissano and colleagues (35) reported that the risk of early death may increase to as high as 17% when infection is present. Similarly, repair involving an aortic fistula is challenging and must additionally address the other injured organ or structure. Figure 2 shows a case in which a patient developed an aortoesophageal fistula after endovascular repair and required complete extraction of the stent-graft via open descending thoracic aorta repair and resection of the esophagus.

The risk of late conversion after endovascular repair in patients with genetically triggered aortic disease (GTAD) is of particular interest; this type of repair is nearly universally considered an off-label approach, and results are generally unpredictable (37). In many centers, endovascular repair in patients with GTAD is performed only in cases in which the stent-graft can be landed within a previously placed surgical aortic graft or can be used as a bridge to definitive open repair. In the current era, the use of the endovascular technology has been extended to all types of aortic pathology because of its less invasive nature, ease of use, and lower associated morbidity; therefore, a certain number of associated failures is expected and may necessitate open repair at an experienced aortic center.
Conclusions
Hybrid and total endovascular approaches to TAAA repair are here to stay. These approaches are used most commonly in high-risk patients, such as octogenarians with multiple comorbidities or those who are considered frail. The determination of the best treatment approach for patients with complex aortic disease will likely be made based on the patient’s health as well as the individual clinician’s familiarity with the technology. Hybrid and total endovascular approaches show promising results but are associated with the risk of paraplegia and mesenteric ischemia in the early postoperative period and the risk of multiple reinterventions in the late postoperative period; additionally, a strict imaging surveillance protocol after repair must be followed. Furthermore, many clinicians will likely lack access to this advanced technology, and gaining sufficient experience to become proficient in its application remains problematic. Additionally, the use of hybrid and endovascular TAAA repair in emergency situations is limited, as both of these approaches are better suited to elective repair. Given the variety and difficulty of clinical scenarios combined with the continued development of novel approaches, evaluating these complex endovascular procedures is difficult. Lastly, the number of surgeons who can safely perform traditional open TAAA surgery is decreasing. It is safe to say the future is here and looms large, but challenges remain in deciding on the exact technique, the timing, and the optimal target population for endovascular repair.
Acknowledgements
The authors thank several members of the Surgical Research Core of the Michael E. DeBakey Department of Surgery at Baylor College of Medicine: Susan Y. Green, MPH, and Hiruni S. Amarasekara, MS, for editorial support. We thank Monica Wierzbicki for creating illustrations and figures and the Section of Scientific Publications at the Texas Heart Institute for providing editorial support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Coselli JS, LeMaire SA, Preventza O, et al. Outcomes of 3309 thoracoabdominal aortic aneurysm repairs. J Thorac Cardiovasc Surg 2016;151:1323-37. [Crossref] [PubMed]
- Svensson LG, Crawford ES, Hess KR, et al. Experience with 1509 patients undergoing thoracoabdominal aortic operations. J Vasc Surg 1993;17:357-68; discussion 368-70. [Crossref] [PubMed]
- Aftab M, Songdechakraiwut T, Green SY, et al. Contemporary outcomes of open thoracoabdominal aortic aneurysm repair in octogenarians. J Thorac Cardiovasc Surg 2015;149:S134-41. [Crossref] [PubMed]
- Girardi LN, Ohmes LB, Lau C, et al. Open repair of descending thoracic and thoracoabdominal aortic aneurysms in patients with preoperative renal failure. Eur J Cardiothorac Surg 2017;51:971-7. [Crossref] [PubMed]
- Girardi LN, Lau C, Munjal M, et al. Impact of preoperative pulmonary function on outcomes after open repair of descending and thoracoabdominal aortic aneurysms. J Thorac Cardiovasc Surg 2017;153:S22-9.e2. [Crossref] [PubMed]
- van de Graaf RA, Grune F, Hoeks SE, et al. One-year follow-up after hybrid thoracoabdominal aortic repair. Vasc Endovascular Surg 2017;51:23-7. [Crossref] [PubMed]
- Hawkins RB, Mehaffey JH, Narahari AK, et al. Improved outcomes and value in staged hybrid extent II thoracoabdominal aortic aneurysm repair. J Vasc Surg 2017;66:1357-63. [Crossref] [PubMed]
- Schanzer A, Simons JP, Flahive J, et al. Outcomes of fenestrated and branched endovascular repair of complex abdominal and thoracoabdominal aortic aneurysms. J Vasc Surg 2017;66:687-94. [Crossref] [PubMed]
- Oderich GS, Ribeiro M, Reis de Souza L, et al. Endovascular repair of thoracoabdominal aortic aneurysms using fenestrated and branched endografts. J Thorac Cardiovasc Surg 2017;153:S32-41.e7. [Crossref] [PubMed]
- Eagleton MJ, Follansbee M, Wolski K, et al. Fenestrated and branched endovascular aneurysm repair outcomes for type II and III thoracoabdominal aortic aneurysms. J Vasc Surg 2016;63:930-42. [Crossref] [PubMed]
- Di Bartolomeo R, Murana G, Cefarelli M, et al. Hybrid two-stage repair of thoracoabdominal aortic aneurysm. Multimed Man Cardiothorac Surg 2016;2016. pii: mmw008.
- Grant SW, Hickey GL, Grayson AD, et al. National risk prediction model for elective abdominal aortic aneurysm repair. Br J Surg 2013;100:645-53. [Crossref] [PubMed]
- Shahian DM, O'Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg 2009;88:S2-22. [Crossref] [PubMed]
- Nashef SA, Roques F, Michel P, et al. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 1999;16:9-13. [Crossref] [PubMed]
- Mastracci TM, Greenberg RK, Hernandez AV, et al. Defining high risk in endovascular aneurysm repair. J Vasc Surg 2010;51:1088-95.e1. [Crossref] [PubMed]
- Bub GL, Greenberg RK, Mastracci TM, et al. Perioperative cardiac events in endovascular repair of complex aortic aneurysms and association with preoperative studies. J Vasc Surg 2011;53:21-7.e1-2.
- Benrashid E, Wang H, Andersen ND, et al. Complementary roles of open and hybrid approaches to thoracoabdominal aortic aneurysm repair. J Vasc Surg 2016;64:1228-38. [Crossref] [PubMed]
- Spiliotopoulos K, Price MD, Amarasekara HS, et al. Are outcomes of thoracoabdominal aortic aneurysm repair different in men versus women? A propensity-matched comparison. J Thorac Cardiovasc Surg 2017;154:1203-14.e6. [Crossref] [PubMed]
- Coselli JS, Rosu C, Amarasekara HS, et al. Reoperative surgery on the thoracoabdominal aorta. J Thorac Cardiovasc Surg 2018;155:474-85.e1. [Crossref] [PubMed]
- Coselli JS, Green SY, Preventza O, et al. Combining open and endovascular approaches to complex aneurysms. In: Pearce WH, Matsumura J, Morasch M, et al. editors. Vascular Surgery: Therapeutic Strategies. People’s Medical Publishing House, 2010:529-48.
- Quinones-Baldrich WJ, Panetta TF, Vescera CL, et al. Repair of type IV thoracoabdominal aneurysm with a combined endovascular and surgical approach. J Vasc Surg 1999;30:555-60. [Crossref] [PubMed]
- Greenberg RK, Lu Q, Roselli EE, et al. Contemporary analysis of descending thoracic and thoracoabdominal aneurysm repair: a comparison of endovascular and open techniques. Circulation 2008;118:808-17. [Crossref] [PubMed]
- Rosset E, Ben Ahmed S, Galvaing G, et al. Editor's choice--hybrid treatment of thoracic, thoracoabdominal, and abdominal aortic aneurysms: a multicenter retrospective study. Eur J Vasc Endovasc Surg 2014;47:470-8. [Crossref] [PubMed]
- Moulakakis KG, Mylonas SN, Antonopoulos CN, et al. Combined open and endovascular treatment of thoracoabdominal aortic pathologies: a systematic review and meta-analysis. Ann Cardiothorac Surg 2012;1:267-76. [PubMed]
- Chiesa R, Tshomba Y, Logaldo D, et al. Possible graft-related complications in visceral debranching for hybrid B dissection repair. Ann Cardiothorac Surg 2014;3:393-9. [PubMed]
- Etz CD, Zoli S, Mueller CS, et al. Staged repair significantly reduces paraplegia rate after extensive thoracoabdominal aortic aneurysm repair. J Thorac Cardiovasc Surg 2010;139:1464-72. [Crossref] [PubMed]
- Ghanta RK, Kern JA. Staged hybrid repair for extent II thoracoabdominal aortic aneurysms and dissections. Operative Techniques in Thoracic and Cardiovascular Surgery 2014;19:238-51. [Crossref]
- Canaud L, Gandet T, Ozdemir BA, et al. Staged hybrid repair to reduce the risk of spinal cord ischemia after extensive thoracic aortic aneurysm repair. Ann Thorac Surg 2016;101:e9-11. [Crossref] [PubMed]
- Etz CD, Weigang E, Hartert M, et al. Contemporary spinal cord protection during thoracic and thoracoabdominal aortic surgery and endovascular aortic repair: a position paper of the vascular domain of the European Association for Cardio-Thoracic Surgerydagger. Eur J Cardiothorac Surg 2015;47:943-57. [Crossref] [PubMed]
- Ferrer C, Cao P, De Rango P, et al. A propensity-matched comparison for endovascular and open repair of thoracoabdominal aortic aneurysms. J Vasc Surg 2016;63:1201-7. [Crossref] [PubMed]
- Eagleton MJ, Farivar B, Dias A. Large, single-center databases and the evolution of endovascular therapy for complex aortic aneurysms. Surgery 2017;162:963-73. [Crossref] [PubMed]
- Wolosker N, Fioranelli A, Ferreira M, et al. Endovascular repair of ruptured thoracoabdominal aortic aneurysm with an off-the-shelf endoprosthesis. Ann Vasc Surg 2017;43:312.e1-312.e4. [Crossref] [PubMed]
- Spiliotopoulos K, Preventza O, Green SY, et al. Open descending thoracic or thoracoabdominal aortic approaches for complications of endovascular aortic procedures: 19-year experience. J Thorac Cardiovasc Surg 2018;155:10-8. [Crossref] [PubMed]
- LeMaire SA, Green SY, Kim JH, et al. Thoracic or thoracoabdominal approaches to endovascular device removal and open aortic repair. Ann Thorac Surg 2012;93:726-32;discussion 733. [Crossref] [PubMed]
- Melissano G, Tshomba Y, Mascia D, et al. Late open conversion after TEVAR. J Cardiovasc Surg (Torino) 2016;57:491-7. [PubMed]
- Orozco-Sevilla V, Weldon SA, Coselli JS. Operative video demonstrating a case of stent-graft extraction after open repair. Asvide 2018;5:302. Available online: http://www.asvide.com/article/view/23686
- Quintana E, Bruce C, Sabate Rotes A. Anatomical aortic reconstruction in Marfan disease: dismantling of a hybrid repair. Eur J Cardiothorac Surg 2015;48:507-9. [Crossref] [PubMed]
Cite this article as: Orozco-Sevilla V, Weldon SA, Coselli JS. Hybrid thoracoabdominal aortic aneurysm repair: is the future here? J Vis Surg 2018;4:61.


