Laparoscopic repair of multiple incisional hernias in a single midline incision by double composite mesh
Introduction
Laparoscopic repair for abdominal incisional hernia with anti-adhesion mesh has been widely adopted nowadays. Data from USA in 2013 revealed that about 20–27% of repairs for ventral and abdominal incisional hernias were performed laparoscopically (1,2). In meta-analysis, there is no difference in recurrence between laparoscopic and open repair for ventral and incisional hernias, but laparoscopic repair has the merit of reducing surgical site infective complication when compared with open repair (1.6% vs. 10.1%) (3). The major operative steps of laparoscopic repair of ventral incisional hernia include ports positioning, adequate adhesiolysis, defect closure and mesh fixation (4). On the other side, in view of the clinical heterogenicity in location, quantity and size of abdominal incisional hernia, the repair strategy can be very challenging in some cases. In this article, we present a case with multiple hernias (swiss-cheese lesions) in one long midline incision repaired with double anti-adhesion mesh by IPOM technique.
Patient demographics
The patient is a 67-year-old lady who had open myomectomy 20 years ago for myoma of uterus. Reducible non-tender mass was found by patient over upper end of previous abdominal incision about 1 year ago. The mass enlarged gradually without pain. On physical examination, the midline scar was 25 cm in length extended from 10 cm above umbilicus to the suprapubic area. A reducible incisional hernia with size of 5 cm was found on the upper part of the incision. Besides, our patient had history of hypertension which was well controlled by medication.
Pre-operative preparation
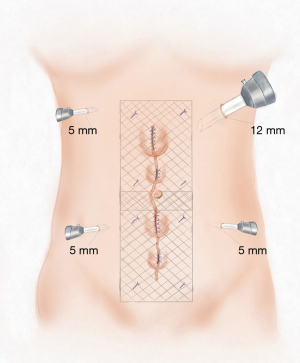
Contrast CT scan was performed for better delineation of defects and planning of laparoscopic repair. Multiple defects (a total of 4) were found from 8.5 cm above the umbilicus to 10.5 cm below which ranging from 1.7 to 3 cm ( Figure 1) . In view of multiple defects scattered over the long midline incision, there is no single mesh which is commercially available in the market that can cover all the defects with enough circumferential overlapping (5 cm) in both longitudinal and transverse directions. Therefore, we decided to repair the defects with two 15×10 cm anti-adhesive meshes (Figure 2).

Equipments and consumables
High definition laparoscopic video system (EVIS EXERA III, CV190, OLYMPUS®), laparoscopic high flow insufflation unit (UHI-4, OLYMPUS®), routine laparoscopic instruments including atraumatic graspers, needle holder, scissors. Ultrasonic dissector (Harmonic Ace, Johnson & Johnson™, 2/0 polyprophylene suture (PROLENE®, Johnson & Johnson™), titanium tackers (PROTACK®, Medtronics™), two 15×10 cm composite meshes (PARIETEX COMPOSITE®, Medtronics™), and port site closure device (ENDO CLOSE™, Medtronics™).
Procedure
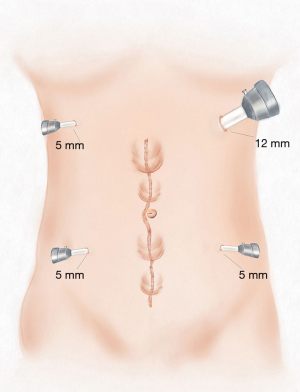
The patient was positioned supine after induction of general anesthesia. Operative site was disinfected with chlorohexidine and alcohol solution. A 12 mm trocar and three 5 mm trocars were placed over both sides abdominal wall by open approach and laparoscopic guidance (Figure 3). The trocars on same side were about 10 cm apart and all the trocars were 10 cm apart to the previous midline incision. Pneumoperitoneum was created by carbon dioxide at pressure of 12 mmHg and the diagnostic laparoscopy was performed via 12 mm trocar. There was adhesion of greater omentum and small intestine to previous midline incision. Adhesiolysis was performed by ultrasound dissector and sharp cut by laparoscopic scissors without monopolar energy. The 4 defects were delineated and hernia content was reduced with combination of external manual pressure and laparoscopic reduction with graspers. The defect over lower end was just on the dome of bladder therefore it was mobilized to facilitate mesh placement and anchorage (trans-abdominal partial extra-peritoneal technique, TAPE) (5). The 4 defects were measured by intra-corporal ruler over peritoneal side. The edge of the defects was also marked at the skin level by medical use marker pen. Subsequently the proposed mesh coverage site was marked at skin level as reference for trans-abdominal suture retrieval and fixation. The defects were then closed by polypropylene sutures with help of port site closure device in interrupted manner. Composite meshes were placed into abdominal cavity via the 12 mm trocar and fixed by trans-abdominal sutures at 4 edges of the meshes and titanium tacks in double crowning manner with 1–1.5 cm apart from each other. The two meshes overlapped in middle of the midline wound. Haemostasis and no intra-peritoneal iatrogenic injury were confirmed before the end of procedure (Figure 4).
Post-operative progress
The patient resumed liquid diet 6 hours post operation. Non-parental painkiller (diclofenac sodium) was administrated orally per 12 hours. The patient was discharged on day 2 post operation. Pain score was 0 at 3 weeks’ time. No recurrence, chronic pain or chronic discomfort was reported at 19-month post operation.
Tips, tricks and pitfalls
- For multiple abdominal incisional hernias, surgical repair is more difficult than that of single ones. CT scan prior to surgery is helpful to delineate the quantity, location, and size of the defects. The strategy of repair and meshes must be anticipated and prepared pre-operatively. When a single mesh cannot achieve adequate coverage of the hernia defects, multiple meshes can be used to ensure adequacy of repair;
- Undesirable trocar positioning reduces ease of laparoscopic manipulation, therefore trocars should be placed at least 10 cm away from the anticipated operative area. A 12 mm trocar is mandatory for intra-peritoneal placement of mesh;
- Operative surgeon and assistants may need to change positions to ensure adequacy of repair, coverage of defects and fixation of the meshes. Laparoscopy and operating instruments may need to change access trocars to facilitate laparoscopic manipulation, and camera should be in-line with the operative instruments to avoid operate under mirror images;
- Adhesiolysis is a risky step that should be performed meticulously if the bowel is adhered to the operating area. Once enterotomy is created and peritoneal cavity is contaminated, it will result in an intricate dilemma of whether mesh should be used for the repair. Ultrasound dissector is good for dissecting omentum and fat tissue adhesions due to its excellent hemostatic effect, but it can cause collateral injury to surrounding bowel by its high temperature active blade. Sharp cutting by laparoscopic scissors is advised for adhesiolysis of bowel adhesions. Hybrid dissection of adhesion by creating a small wound and adhesiolysis under hand-assisted with direct vision can be considered if severe adhesion is encountered. The wound is then closed afterward and laparoscopic repair is continued;
- When tying the knots of the suture for defect closure by trans-abdominal sutures, the pneumoperitoneum pressure should be reduced to 7–8 mmHg to relieve the tension and avoid tear of tissues;
- Accurate assessment, measurement, delineation and marking of defects and proposed exit points of transabdominal sutures are vitally important to ensure sufficient coverage of the defects and avoidance of folding of the meshes after fixation;
- Composite mesh should be preprocessed and softened by soaking into normal saline before putting into peritoneal cavity. The mesh is then rolled along the axis of a clean atraumatic instrument with the cellulose film facing inward, and put into the abdominal cavity via 12 mm trocar to avoid breaking of the anti-adhesive film;
- When the dome of bladder prohibits adequate placement and fixation of mesh, it should be mobilized according principle of TAPE technique;
- The trans-abdominal sutures should exit 1 cm lateral to the edges of the meshes to allow spreading out and tenting of the mesh (Figure 2). This can facilitate the fixation by titanium tacks in true double crowning manner. When tacks are fired, counter-action should be provided by compressing the abdominal wall from outside against the tacker which is firing from inside the peritoneal cavity. The overlapping part of the meshes should be fixed securely to avoid recurrence at this region.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional review board in our center waived the approval process and the informed consent of case video for single patient if it contains surgical procedures or techniques with no individual identifier and intended risk for individual patient.
References
- Alexander AM, Scott DJ. Laparoscopic ventral hernia repair. Surg Clin North Am 2013;93:1091-110. [Crossref] [PubMed]
- Funk LM, Perry KA, Narula VK, et al. Current national practice patterns for inpatient management of ventral abdominal wall hernia in the United States. Surg Endosc 2013;27:4104-12. [Crossref] [PubMed]
- Arita NA, Nguyen MT, Nguyen DH, et al. Laparoscopic repair reduces incidence of surgical site infections for all ventral hernias. Surg Endosc 2015;29:1769-80. [Crossref] [PubMed]
- Yang XF, Liu JL. Laparoscopic repair of abdominal incisional hernia. Ann Transl Med 2016;4:342. [Crossref] [PubMed]
- Fan JKM, Yip J, Fung M, et al. Minimally Invasive Approach to Supra-pubic and Non-Midline Lower Abdominal Ventral Hernia – An Extended Indication of TAPE Technique. J Minim Invasive Surg 2017;20:84-92. [Crossref]
- Yang X, Jiang L, Li Y, et al. Laparoscopic repair of multiple incisional hernias with 2 overlapping composite meshes. Available online: Asvide 2018;5:175. Available online: http://www.asvide.com/article/view/23517
Cite this article as: Yang X, Jiang L, Li Y, Liu J, Fan JK. Laparoscopic repair of multiple incisional hernias in a single midline incision by double composite mesh. J Vis Surg 2018;4:58.