Robot-assisted thoracoscopic right upper bi-lobectomy for pulmonary tuberculosis
Introduction
Lobectomy and bi-lobectomy constitute up to 41.6% of all lung resections for pulmonary tuberculosis (TB) (1). However, sclerosed and calcified lymph nodes are the reasons of technical difficulties during the isolation of hilar structures. The division of dense pleural adhesions is associated with lung lacerations and opening of tuberculous cavities in some cases. For this reason, video-assisted thoracoscopic surgery (VATS) bi-lobectomy is rarely used. Right now robotic surgery is the newest version of VATS. Several thoracic centers have already had experience in robot-assisted thoracoscopic (RATS) pulmonary lobectomy for tuberculosis (2). However, we had found no papers about using robotic surgical system in cases with tuberculous lesions in two pulmonary lobes.
Case presentation
A 31-year-old male was admitted to the Chest center 16/02/2016. He suffered from weakness, cough and fever since April, 2015. X-ray examination showed inflammatory infiltrates with foci’s in the right lung. There was positive sputum smear on M. tuberculosis (MTB). MTB had sensitivity to all anti-TB drugs. The primary course of the medical treatment for tuberculosis with first line drugs lasted for 11 months. The result of the treatment was the formation of large TB lesion in the boundaries of the right upper lobe and cavitary TB in the right middle lobe.
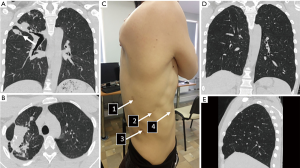
At hospital admission, patient had complaints of weakness and irregular cough. The examinations showed negative sputum smears on MTB. Cardiorespiratory tests did not reveal abnormalities. There were no comorbidities. Computed tomography-scans (CT) before surgery are presented on the Figure 1. The large tuberculous lesion with cavity in the middle lobe after adequate course of antituberculosis treatment was an absolute indication for surgery, according to World Health Organization recommendation (3).
RATS right upper bi-lobectomy was performed on March 2, 2016. The overall operative time was 190 min, intraoperative blood loss was 50 mL. Patient was placed in a lateral decubitus position on the left side. Camera’s port was inserted inferiorly in the 7th intercostal space at the posterior axillary line. Video thoracoscopy showed pleural adhesions in the apex. Two instrumental and assistant ports were inserted in the 6th (middle clavicular line), the 7th (scapular line) and the 9th intercostal spaces (between scapular and posterior axillary lines).
Consecutive steps of surgery are presented on video (Figure 2). There was a feature of vascular anatomy: additional middle lobe artery and seventh segmental artery had the same origin from intermediate trunk of pulmonary artery. Specimen was removed through assistant port, which was expanded up to 3 cm. Two chest tubes were used due to the incomplete volume compliance of the right lower lobe and pleural cavity.
Postoperative period was complicated by prolonged air leak up to the 17th postoperative day. It required replace the chest tube on the 13th day and perform artificial pneumoperitoneum. MTB without drug-resistance was detected in the specimen. The postoperative course of antituberculosis treatment was prolonged with the first line of drugs.
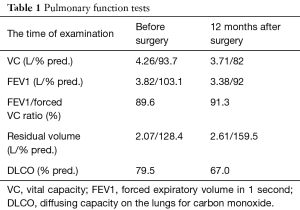
Patient was examined 1 year later after the surgery (Figure 1). Patient had no complaints. Results of pulmonary function test are presented in Table 1. Lung function parameters insignificantly sunk, patient had lost 12.9% of vital capacity (VC), 11.5% of forced expiratory volume in 1 second (FEV1), and 16.2% of diffusing capacity on the lungs for carbon monoxide (DLCO) after bilobectomy. Chest CT did not find later complications and progression of TB (Figure 1).
Full table
Discussion
Minimally-invasive surgery for tuberculosis is an existing topic for discussion. Nowadays, robot-assisted lobectomy became the standard procedure for patients with pulmonary tuberculosis in our thoracic center despite the some features, which usually associated with infectious diseases (dense pleural adhesions, peribronchial fibrosis). This case presents initial experience in robot-assisted bi-lobectomy. In our opinion, four ports are enough for all types of RATS pulmonary resections. Anterior approach is more preferable. It was more convenient to differentiate vascular anatomical abnormalities. Postoperative follow-up showed successful results of complex treatment of pulmonary tuberculosis. However, increase of residual volume may be sign of bronchial obstruction (Table 1). This phenomenon was described in few publications for non-smokers after treatment of pulmonary TB (5). Another reason of functional disorders could be explained by surgical procedure itself. However, the functional recovery of our patient was generally better than in previously reported studies for lung cancer (6). This may be associated with removal of not functional tissue in TB-cases. That’s why we routinely referred such patients to a pulmonologist for rehabilitation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report.
References
- Rohde G, Subotic D. Complex Pleuropulmonary Infections: European Respiratory Monograph 61. European Respiratory Society 2013;61:20-36.
- Yablonskii P, Kudriashov G, Vasilev I, et al. Robot-assisted surgery in complex treatment of the pulmonary tuberculosis. J Vis Surg 2017;3:18. [Crossref] [PubMed]
- World Health Organization. The role of surgery in the treatment of pulmonary TB and multidrug-and extensively drug-resistant TB. Available online: http://www.euro.who.int/en/health-topics/communicable-diseases/tuberculosis/publications/2014/the-role-of-surgery-in-the-treatment-of-pulmonary-tb-and-multidrug-and-extensively-drug-resistant-tb
- Yablonskii P, Kudriashov G, Kiryukhina L, et al. Steps of RATS bilobectomy. Asvide 2018;5:115. Available online: http://www.asvide.com/article/view/23338
- Baig IM, Saeed W, Khalil KF. Post-tuberculous chronic obstructive pulmonary disease. J Coll Physicians Surg Pak 2010;20:542-4. [PubMed]
- Win T, Groves AM, Ritchie AJ, et al. The effect of lung resection on pulmonary function and exercise capacity in lung cancer patients. Respir Care 2007;52:720-6. [PubMed]
Cite this article as: Yablonskii P, Kudriashov G, Kiryukhina L, Avetisyan A. Robot-assisted thoracoscopic right upper bi-lobectomy for pulmonary tuberculosis. J Vis Surg 2018;4:48.


