Micro-incision thoracoscopic treatment of primary spontaneous pneumothorax: the “loop” technique
Introduction
Video-assisted thoracoscopic surgery (VATS) is the standard surgical procedure for patients with primary spontaneous pneumothorax (PSP) (1).
Yamamoto et al. (2) in 1998 published a small series of 6 patients operated using a single incision approach with a flexible bronchoscope as a camera with good results. However, a standardized technique for VATS wedge pulmonary resection through a single port (SITS) was first reported by Rocco et al. (3). SITS has many advantages over three-port VATS, including favorable cosmetic results and lower rates of postoperative pain and paresthesia (4,5). Patients affected by PSP are in the most of the cases young and otherwise healthy. PSP is benign affection and therefore the goal of surgery as well as solving the pneumothorax and reducing the risk of recurrence should be aimed at creating the least functional and aesthetic damage to these patients who must resume a social and work life as normal as possible.
In order to minimize surgical insult we studied a new surgical approach for the treatment of spontaneous pneumothorax performing a micro-single incision to insert in the chest the thoracoscope and the stapler while the lung is suspended to perform the wedge resection with a hand-made loop avoiding the necessity of further cumbersome, dedicated and expansive surgical instrument.
Patient selection and workup
We use this technique for patients with ipsilateral primary spontaneous pneumothorax (PSP) recurrence, persistent air leakage after chest tube drainage, contralateral PSP according to the current guidelines. The case we present is a 27-year-old male arrived at the Emergency Room complaining of the onset of an acute right chest pain. The chest X-ray showed a 3 cm wide right-sided apical pneumothorax. The patient had undergone a standard three ports VATS because of a contralateral spontaneous pneumothorax in 2009, so we decided to bring the patient directly into the operating room. No other radiological exams are needed.
Pre-operative preparation
Routine laboratory tests, chest X-rays, EKG, trichotomy.
Equipment preference card
- 30-degree, 5 mm thoracoscope;
- A 15 mm flexible thoracic trocar;
- Endoscopic graspers;
- A mechanical stapler (Endo GIA™ Ultra Universal Standard, Covidien Products);
- A cautery hook;
- A cautery tip cleaner (for pleural abrasion);
- ETHIBOND EXCEL® Polyester Suture 2, Ethicon - Johnson & Johnson Medical S.p.A.
Patient positioning
A double-lumen endotracheal tube is inserted and the patient is placed in a lateral decubitus position on the table next to its anterior edge. The table is arched to open the intercostal space maximally. The surgeon stands on the abdominal side of the patient.
Nurse and assistant positioning
The scrub nurse and the assistant surgeon stand on the opposite side with respect to the operating surgeon.
Procedure
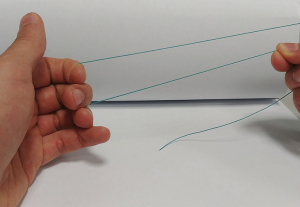
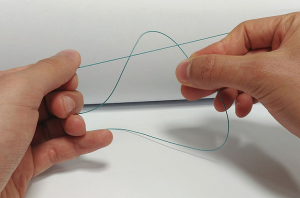
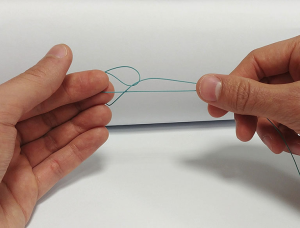
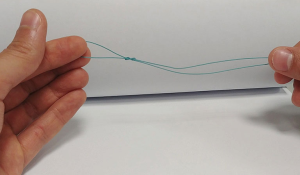
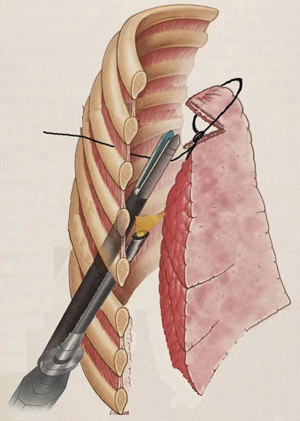
A surgical incision of 2 cm in length is performed on the midaxillary line, on the 8th intercostal space. Using a 5-mm- diameter 30-degree thoracoscope, a dystrophic area at the apex of the superior lobe is identified (Figure 1). A non-absorbable braided suture (ETHIBOND EXCEL® Polyester Suture 2, Ethicon - Johnson & Johnson Medical S.p.A.) is passed from outside into the chest wall, through the IV intercostal space on the anterior axillary line, and a slip-knot is tied in order to create a loop outside the chest. Then a 5 mm endograsp is used to bring the loop inside the chest and adjust it around the dystrophic area of the lung. This is used to isolate and suspend the damaged area (Figures 2,3). The lesion is then elevated at the centre of the chest cavity by pulling the thread on the side of the chest wall, creating an angle and making space to introduce a stapler to excise the lesion. Once the resection is completed, the tissue is removed by pulling on the thread on the incisional side. The lower lobe is then retracted superiorly and the inferior pulmonary ligament is transected with a cautery hook, in order to avoid a postoperative residual pleural space at the apex. Mechanical abrasion pleurodesis to all of the chest cavity, except to the diaphragm, is performed using a cautery tip cleaner. Finally, a 24F chest tube is inserted into the pleural cavity through the incision site and the skin is closed around the tube (Figure 4).

Postoperative management
The patient is extubated in the OR and transferred to the ward. Postoperative pain relief is provided by intravenous paracetamol three times per day. Suction drainage at −20 cmH2O is used. We use a digital chest drainage system (Thopaz™, Medela Italia Srl). Chest tube is removed when the pleural effusion is lower than 400 mL/day and air leak flow <40 mL/min for more than 8 h (and without spikes of airflow greater than this value), in this case 48 hours after the operation (7). Follow-up chest X-rays is performed one month after the operation. There were no complications at 6 months follow-up.
Tips, tricks and pitfalls
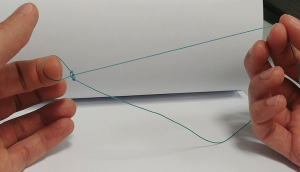
A slip knot is tied in order to create the loop. As shown in the Figure 5, first of all you need to take the end of the robe and wrap it around two fingers, so the end is under the middle portion of the thread. Then (Figure 6) you need to bring the end up and over the middle portion of the line and keep it facing down. With the two fingers you need to bring the middle portion of the thread and pull it through the loop while holding the ends (Figures 7,8). At this point the loop is created and you can try to test it losing or tying it (Figure 9).
We suggest to use an angulated instrument to hold the cautery tip cleaner and perform the mechanical pleurodesis so it’s possible to reach every part of the parietal pleura, even close to the access.
Conclusions
VATS is nowadays a common procedure in thoracic surgery and the standard approach for primary spontaneous pneumothorax. In the last few years, single port VATS is taking up space over the standard three ports because of less postoperative pain, lower paraesthesia rate and shorter hospital stay (4). Patients affected by PSP are in the most of the cases young and otherwise healthy. PSP is a benign affection and therefore the goal of surgery as well as solving the pneumothorax and reducing the risk of recurrence should be aimed at creating the least functional and aesthetic damage to these patients who must resume a social and work life as normal as possible. In the past, different groups described surgical techniques using different devices an mini loop retractors to suspend the lung for performing wedge resections (8,9).
This technique allowed us to perform a uniportal thoracoscopic lung resection and pleural abrasion reducing further the skin and intercostal incision without compromising the effectiveness of pneumothorax treatment.
Son et al. described the anchoring suture technique for single port VATS wedge resection (10,11); in this case the needle is passed through the lung parenchyma instead of creating a loop anchoring the lung.
Recently Tsuboshima et al. (12) described good results using a technique called modified Chest Wall Pulley (mPulLE) for Lung Excision. In their approach the lung is suspended using a kind of pulley through a single incision. They report a significant difference between the mPulLE cases and the three-port VATS cases in the operative time and the number of autosutures used.
The operative field using a 30° camera is optimal to perform a complete pleural abrasion as well the division of the pulmonary ligament is easy to perform.
Our loop technique allows to perform SITS without increasing the cost of the operation because no other device is needed. In our case we were able to resect blebs without problems, the recovery was excellent and no complications related to the procedure were reported.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this article and any accompanying images.
References
- Treasure T. Minimally invasive surgery for pneumothorax: the evidence, changing practice and current opinion. J R Soc Med 2007;100:419-22. [Crossref] [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [Crossref] [PubMed]
- Campisi A, Dell’Amore A, Giunta D, et al. The “loop” technique, from the incision to the wound closure. Asvide 2018;5:085. Available online: http://asvidett.amegroups.com/article/view/22881
- Pompili C, Brunelli A, Salati M, et al. Impact of the learning curve in the use of a novel electronic chest drainage system after pulmonary lobectomy: a case-matched analysis on the duration of chest tube usage. Interact Cardiovasc Thorac Surg 2011;13:490-3. [Crossref] [PubMed]
- Ichinose J, Nakahara K, Kina S, et al. One-port video-assisted thoracic surgery for pneumothorax using mini loop retractor. Kyobu Geka 2010;63:371-4. [PubMed]
- Tsuboshima K, Matoba Y, Sato M, et al. Evaluation of 2 ports video-assisted thoracoscopic surgery (VATS) using endo-close for primary spontaneous pneumothorax. Kyobu Geka 2013;66:210-3. [PubMed]
- Son BS, Kim DH, Lee SK, et al. Small Single-Incision Thoracoscopic Surgery Using an Anchoring Suture in Patients With Primary Spontaneous Pneumothorax: A Safe and Feasible Procedure. Ann Thorac Surg 2015;100:1224-9. [Crossref] [PubMed]
- Jeon HW, Kim YD. Does 11.5 mm guided single port surgery has clinical advantage than multi-port thoracoscopic surgery in spontaneous pneumothorax? J Thorac Dis 2016;8:2924-30. [Crossref] [PubMed]
- Tsuboshima K, Nagata M, Wakahara T, et al. Feasibility of single-incision thoracoscopic surgery using a modified chest wall pulley for primary spontaneous pneumothorax: a propensity score matching analysis. Surg Today 2017;47:1129-34. [Crossref] [PubMed]
Cite this article as: Campisi A, Dell’Amore A, Giunta D, Congiu S, Daddi N, Dolci G. Micro-incision thoracoscopic treatment of primary spontaneous pneumothorax: the “loop” technique. J Vis Surg 2018;4:35.