A word of caution—when uniportal VATS should not be done
Within the last few years, uniportal video-assisted thoracic surgery (U-VATS) has gained popularity. Migliore et al. introduced this approach for simple minimally invasive thoracic procedures more than 10 years ago (1). Since that time, the technique was adopted by a growing number of thoracic surgeons. When U-VATS and its use is compared to the classic technology adoption curve (Figure 1, adopters are grouped in “innovators”, “early adopters”, “early majority”, “late majority” and “laggards”), Migliore and his group would be the group of innovators. The uniportal access was then used by Gonzalez-Rivas et al. to perform the first U-VATS lobectomy in 2011 (2). For this achievement he is also considered an innovator in the technology adoption curve. Since 2011, a considerable amount of literature on U-VATS has been published. Reports include resections of all different lobes, segmentectomies, pneumonectomies, and even sleeve resections (bronchial and vascular sleeves) demonstrating the feasibility and safety of U-VATS. According to the adoption curve, let us assume that the authors of these studies are all in the group of early adopters. A lot of effort has been undertaken to promote the U-VATS approach and to present it as the best possible technique for minimally invasive thoracic surgery: Numerous thoracic surgeons are traveling to China to see the World’s most renowned uniportal surgeons live doing more than 70 (!) cases a day in a single center. Books have been written to explain the technique. Even this special issue of the Journal of Visualized Surgery is dedicated to transfer the knowledge that has already been gained and to attract more thoracic surgeons to be part of the “early majority”.
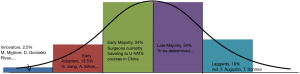
And yet, U-VATS has not reached the “late majority” of thoracic surgeons and is not the most common minimally invasive approach worldwide. This article—opposing all other articles in this special issue—is supposed to raise awareness why U-VATS is still not as widespread as conventional VATS (C-VATS) anatomic lung resections. From a “laggard’s” perspective, we will discuss circumstances, where a U-VATS approach should be reevaluated. Please consider that these circumstances represent our opinion, and sometimes—without scientific background—express a (C-VATS experienced) laggard’s gut feeling.
For the sake of discussion, we will not challenge the given fact that a minimally invasive approach is beneficiary to our patients. Even though the minimally invasive thoracic community was lacking a bullet-proof argument about its benefits, C-VATS was introduced and due to an ever-growing number of retrospective (and some prospective) data gradually adopted by many. Depending on local expertise, C-VATS penetration rates vary from 0 to 90% or even more (3). In general, a constant rise of a minimally invasive approach is recognized. Finally, in 2016, Licht et al. published a prospective randomized controlled trial (RCT) showing less pain and a better quality of life in patients undergoing a C-VATS approach compared to an anterolateral thoracotomy for anatomic lung resections (4). This study brought the so far missing RCT evidence of benefits and therefore peace of conscience to the minimally invasive C-VATS community.
Since its introduction, U-VATS is presented as a refinement of C-VATS. As such, it should demonstrate advantages, in an optimal setting for both, surgeons and patients. If it’s the most beneficiary technique for patients, what hinders surgeons to adopt the technology and revise their technique? There will be the same factors at play than with the change from open thoracotomy to C-VATS: oncologic concerns, economic reasons, lack of instruments/infrastructure (high definition video tower), education/teaching, operating room schedule, and personal perception to name just a few (3). But the most influencing factor of all will be the burden of change itself: Leaving one’s comfort zone might be the biggest resistor of all. When you are comfortable doing a C-VATS lobectomy, why should you take the challenge of doing a U-VATS approach?
One way to overcome a surgeon’s resistance would be to convince him or her with solid data. But are there any recognized and well-documented advantages of U-VATS? Proponents argue that due to the single intercostal space involved in U-VATS, it results in less postoperative pain and paresthesia, increasing the benefits of a minimally invasive approach (5). In a RCT published in 2016, however, there was no difference in postoperative pain scores between U-VATS and C-VATS. Moreover, this study also demonstrated no difference in the perioperative outcomes like chest drain duration, length of hospital-stay and pain medication intake (6). The study also supports an observational study published in 2015 concluding that there was no difference in postoperative pain and recovery between C-VATS and U-VATS (7). In contrast, we do find criticisms of this RCT as well as studies supporting the less-pain-concept for lobectomies, including one recently published report by Wang et al. (8,9). However, these data are retrospective in nature and therefore considered to be of minor evidence.
Another convincing aspect might be ergonomics as an improvement for surgeons. U-VATS series claim better ergonomics (10). However, the technique needs a skilled (and athletic) assistant who is able to hold the camera steady for sometimes several hours. A survey in 2012 already documented varying degrees of discomfort mainly in the neck, shoulders and back due to thoracoscopic surgery, symptoms that are considered musculoskeletal diseases in environmental health sciences (11). Static postures as carried out by the camera assistant in U-VATS, i.e., holding the camera in the upper corner of the uniportal access, will probably intensify this problem. In C-VATS the position and posture of the assistant holding the camera is undoubtedly more convenient (Figure 2).
Regarding the so far available evidence, we do strongly agree with Gonzalez-Rivas et al. that more solid data are needed to elaborate differences between U-VATS and C-VATS and possibly clarify benefits of one approach over the other (8).
When reading U-VATS case series, it is challenging to read “between the lines”. Phrases like “Although it is technically demanding, …” or “…is a viable alternative approach to C-VATS in selected patients, especially in patients with early peripheral lung cancer with good anatomy and in good general condition” already point out some facts that should be considered (9,13). U-VATS seems to be more challenging than a C-VATS approach. With multiple instruments introduced via a single incision the procedure gets more complicated. Especially for surgeons, who were trained doing a C-VATS lobectomy, the change is not as easy as one might think. As Detterbeck and Molins put it, “user-friendliness trumps effectiveness: if a new technique is hard to perform or learn, adoption will be limited” (3). Liu et al. point out that learning U-VATS might even be easier for younger surgeons who have never been formally trained doing C-VATS anatomic resections (14).
So, when should a U-VATS approach not be done? Factors that should be considered in our opinion are:
- Lack of experience: an inexperienced minimally invasive thoracic surgeon should not try to accomplish a U-VATS lobectomy. This is nothing but dangerous to the patient;
- Lack of systematic U-VATS training: even experienced minimally invasive surgeons should undergo a formal education of U-VATS before attempting the procedure;
- Tumor location and size: large and centrally located tumors with possible involvement of central vessels and airways should not be attempted, at least not during the learning curve and possibly only in a high-volume U-VATS center;
- Hospital volume: without an appropriate number of anatomic resections, the learning curve (for any type of minimally invasive approach) will be hard to complete.
Surgeons willing to master U-VATS should obtain courses teaching minimally invasive techniques, no one should try to re-invent the wheel. While a lot of supporting material is available online and can be used to increase one’s understanding of the procedure, only direct communication and discussion with colleagues will reveal tips and trick.
Completing a resection with U-VATS should never be an obligation. If a surgeon encounters problems or feels to be out of the comfort zone, he or she should take every effort to regain confidence! This might be either by adding a second or third port or even convert to thoracotomy. It is important to never endanger a patient’s life or compromise oncologic principles. As McKenna et al. wrote, a conversion should never be considered a failure but rather a step towards patient’s safety (15).
With all due respects to the achievements of the great inventors of U-VATS anatomic resections, we need to make sure we are offering the best and safest treatment to our patients. For some it might be U-VATS, for others it might be better to stay with C-VATS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Migliore M, Deodato G. Single-trocar technique for minimally-invasive surgery of the chest. Surg Endosc 2001;15:899-901. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Detterbeck F, Molins L. Video-assisted thoracic surgery and open chest surgery in lung cancer treatment: present and future. J Vis Surg 2016;2:173. [Crossref] [PubMed]
- Bendixen M, Jørgensen OD, Kronborg C, et al. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 2016;17:836-44. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS techniquefor spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411-5. [Crossref] [PubMed]
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Damico TA, Jiang G, et al. Uniportal video-assisted thoracic surgery: a call for better evidence, not just more evidence. Eur J Cardiothorac Surg 2016;50:416-7. [Crossref] [PubMed]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [Crossref] [PubMed]
- Welcker K, Kesieme EB, Internullo E, et al. Ergonomics in thoracoscopic surgery: results of a survey among thoracic surgeons. Interact Cardiovasc Thorac Surg 2012;15:197-200. [Crossref] [PubMed]
- Augustin F, Schmid T. Overview within the left thoracic cavity with convenient ergonomics for both, operating surgeon and camera assistant. Asvide 2018;5:072. Available online: http://asvidett.amegroups.com/article/view/22809
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Liu CY, Lin CS, Shih CH, et al. Singleport video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [PubMed]
- McKenna RJ Jr. Complications and learning curves for video-assisted thoracic surgery lobectomy. Thorac Surg Clin 2008;18:275-80. [Crossref] [PubMed]
Cite this article as: Augustin F, Schmid T. A word of caution—when uniportal VATS should not be done. J Vis Surg 2018;4:29.


