The state of uniportal video-assisted thoracoscopic surgery in North America: a survey of thoracic surgeons
Introduction
Since the development of video-assisted thoracoscopic surgery (VATS) in the 1990s, the frontiers of minimally invasive thoracic surgery have continued to expand. In 2004, Rocco was one of the first thoracic surgeons to bring attention to uniportal VATS with his publication on uniportal VATS wedge pulmonary resections (1). In 2011, Gonzalez-Rivas published the first report of a successful major anatomic lung resection using the uniportal VATS approach (2). After a period of relative quiescence, recent years have been characterized by an exponential growth in the number of published reports and case series focusing on uniportal VATS. Most publications originate from Asia and Europe with only around 15 papers from the North America (3). We could not identify these specific references within the reference section of this article. In our search of the English-language literature using the MEDLINE database from 1996 to 2016 (keywords: uniportal, single-port, VATS, thoracoscopy) yielded 290 relevant citations. Only three (1%) original VATS research publications originated from North America (4-6). North American original research papers on this topic represent a very small percentage of the current existing literature on uniportal VATS. In the context of the 2017 Annual Asian Single-Port VATS Symposium held in Shanghai, China, we sought to describe current the state of uniportal VATS in North America and explore factors that could influence future adoption.
Methods
In March 2017, a five-question survey was distributed to North American thoracic surgeons with a clinical practice focused on non-cardiac thoracic surgery and to thoracic surgery residents, and residents received an additional survey with further questions (Supplementary files). Potential survey respondents were identified through personal connections of one of the co-authors (S Gilbert) and through their membership in the General Thoracic Surgical club and the New York Society for Thoracic Surgery. Respondents were encouraged to distribute the survey to other potentially interested surgeons. The survey data was completely anonymous. Based on unofficial communications and surgeon membership data from the Canadian Association of Thoracic Surgeons and the Society of Thoracic Surgeons (STS), we estimated the total number of North American surgeons whose clinical practice is primarily focused on non-cardiac thoracic surgery at 600. Therefore, we estimated that at least 83 respondents would be required to achieve a 95% confidence level and a 10% margin of error on the results. Statistical comparisons of categorical variables were performed using Fisher’s exact test.
Results
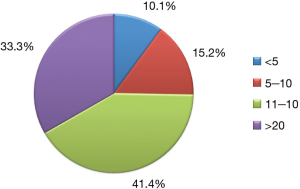
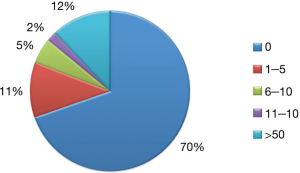
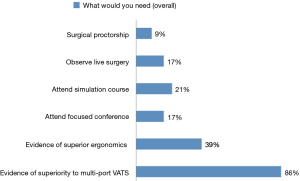
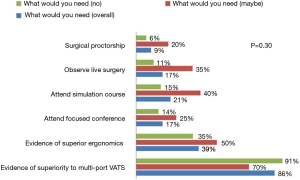
The estimated response rate to the survey was 16.5% (99/600). The majority of respondents were experienced with 41.4% (41/99) having been in practice for 11–20 years; 33.3% (33/99) for over 20 years, 15.2% (15/99) for 5–10 years, and only 10% in practice for less than 5 (10/99) years (Figure 1). The majority (70%; 69/99) of surgeons had never performed a uniportal VATS procedure, however, 18% (18/99) had completed between 1–20 cases and 12% (12/99) reported having performed over 50 cases (Figure 2). The majority of respondents (66%; 65/99) did not perceive any significant advantage associated with uniportal VATS. A small proportion of surgeons (10%; 10/99) were convinced that uniportal VATS was superior to multiport VATS and the remainder of the surgeons surveyed were uncertain (24%; 24/99). The majority of respondents (66%; 65/99) stated that they were not planning to adopt uniportal VATS but one third of the group was open-minded to integrating this approach to their practice. When surgeons were asked to state what could potentially convince them to adopt uniportal VATS, they were allowed to select more than one answer. Scientific evidence of superiority (86%; 85/99) and/or of superior ergonomics (39%; 39/99), attendance to focused conferences with a practical simulation component (38%; 38/99), and the availability of surgical proctorship (9%; 9/99) were the most commonly selected responses (Figure 3). When we divided the surgeons according their plan to adopt uniportal VATS (i.e., yes, no, or maybe), we found no statistical difference between what they identified as essential factors to promote the adoption of the technique (P=0.30) (Figure 4).
Nine surgical residents responded to the survey. Most of them (78%; 7/9) were about to enter a thoracic surgery residency training program in Canada or United States. All residents had regular exposure to advanced minimally invasive procedures and 44% (4/9) had already been exposed to uniportal lung resection with a case volume ranging from 1–5 to over 50 procedures. Most respondents (8/9; 89%) were either planning for or considering the pursuit of further dedicated training in minimally invasive thoracic surgery after completing their residency. The majority of residents surveyed were either convinced or open minded to the concept that uniportal VATS may present advantages over multi-port VATS (78%; 7/9). One third (33%; 3/9) of residents were planning to incorporate uniportal VATS into their practice, another third were uncertain, and the remaining one third did not plan to use this approach in the future.
Discussion
This survey is the first of its kind to provide a glimpse into the status of the uniportal VATS in North America. The responses suggest that there are few early adopters of this approach as compared to other parts of the world. There appears to be a small nucleus of North American surgeons who have already gained experience with uniportal VATS. However, we have yet to see a commensurate number of either case-series or comparative studies focused on uniportal VATS from North American centers. In addition to obtaining a snapshot in time, the survey was designed to complete a basic needs assessment to guide future efforts in promoting a wider spread adoption of uniportal VATS. We anticipate this process to require significantly more time and effort in North America given reports from major societal databases showing limited adoption (≤35% of recorded cases) of conventional multi-port VATS (7,8). Based on the information gathered through this survey, it would appear that obstacles to a more generalized embrace of uniportal VATS also lie in the lack of perceived advantages to uniportal VATS amongst surgeons, the need for more comparative evidence with other established approaches, and improved access to more local workshops with practical and simulation-based components.
Meta-analysis of data from Europe and Asia suggests that uniportal VATS is at least equivalent if not superior to multi-port VATS both in surgical ergonomics and perioperative outcomes (9,10). Despite this, the survey responses clearly indicated that there is a perceived deficit in the scientific evidence between uniportal and multi-port VATS, and that this is a major barrier to integration. This may reflect bias against evidence emanating from other continents and/or a simple lack of proper dissemination of the existing evidence amongst the North American thoracic surgical community. North American surgeons who are interested in uniportal VATS should be encouraged to critically appraise its performance and submit their results for peer-reviewed publication.
Conclusions
We acknowledge the limitations associated with any attempt to generalize survey results to the general population (i.e., North American thoracic surgeons). As we gather more data on the safety and efficacy of uniportal VATS and as other, non-intercostal, alternative VATS approaches emerge into clinical practice, it will be increasingly important to ensure that surgical safety and quality remain under the highest scrutiny. Ongoing efforts to accurately define emerging VATS approaches (e.g., subxyphoid, subcostal, transcervical, etc.) and to adopt standardized terminology will enable the international thoracic surgery community to perform a more objective appraisal of their respective merits.
Supplementary
Questionnaire
- How many years have you been in practice?
- <5 years
- 5–10 years
- 11–20 years
- >20 years
- How many uniportal VATS resections have you conducted?
- 0
- 1–5
- 6–10
- 11–20
- >50
- Do you think uniportal VATS have any advantages over VATS?
- Yes
- No
- Maybe
- Are you planning to integrate uniportal VATS into your practice?
- Yes
- No
- Maybe
- What would you need to integrate uniportal VATS into your practice? Please check all that apply.
- Surgical proctorship
- Observe live surgery
- Attend simulation course
- Attend focused conference
- Evidence of superior ergonomics
- Evidence of superiority to multi-port VATS
Resident survey
- I am currently or plan to be a thoracic surgery resident/fellow in
- Canada
- United States
- Other
- What year of training are you in?
- 0 (not yet started)
- 1
- 2
- 3
- Do you plan to obtain MIS thoracic training in addition to thoracic residency?
- Yes
- No
- Maybe
- Are you regularly (e.g., every week) exposed to advanced VATS/laparoscopic procedures in your training?
- Yes
- No
- How many uniportal VATS lung resections have you participated in?
- 0
- 1–5
- 6–10
- 11–20
- 21–30
- 31–40
- 41–50
- >50
- Do you think that uniportal VATS has any advantage of multi-port VATS?
- Yes
- No
- Maybe
- Are you planning to integrate uniportal VATS lung resection into your practice?
- Yes
- No
- Maybe
Acknowledgements
We would like to express our deepest gratitude to Dr. Mark Allen, Mrs. Bonnie Lemmerman, Dr. Faiz Bhora, and Mrs. Carol Ann Budhai for their assistance in distributing the survey.
Footnote
Conflicts of Interest: This research was presented at the 5th Annual Asian Single Port VATS Symposium in Shanghai, China, March 2017.
References
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, García J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Tu CC, Hsu PK. Global Global development and current evidence of uniportal thoracoscopic surgery. J Thorac Dis 2016;8:S308-18. [PubMed]
- French DG, Thompson C, Gilbert S. Transition from multiple port to single port video-assisted thoracoscopic anatomic pulmonary resection: early experience and comparison of perioperative outcomes. Ann Cardiothorac Surg 2016;5:92-9. [Crossref] [PubMed]
- Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Kara HV, Balderson SS, D'Amico TA. Modified uniportal video-assisted thoracoscopic surgery (VATS). Ann Cardiothorac Surg 2016;5:123-6. [Crossref] [PubMed]
- Boffa DJ, Allen MS, Grab JD, et al. Data from the Society of thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247-54. [Crossref] [PubMed]
- Ceppa DP, Kosinski AS, Berry MF, et al. Thoracoscopic lobectomy has increasing benefit in patients with poor pulmonary function: a society of thoracic surgeons database analysis. Ann Surg 2012;256:487-93. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [Crossref] [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
Cite this article as: Yeung C, Gilbert S. The state of uniportal video-assisted thoracoscopic surgery in North America: a survey of thoracic surgeons. J Vis Surg 2018;4:19.