Uniportal non-intubated thoracic surgery
Introduction
In the modern thoracic surgery, the minimally invasive video-assisted thoracoscopic surgery (VATS) approach has become the gold standard. Uniportal VATS is the most advanced evolution of the minimally invasive technique and has reportedly advantages, like a reduced morbidity, shorter length of stay and less postoperative pain (1,2). This technique allows the possibility to include patients in enhanced recovery after surgery (ERAS) programs, in order to optimize the therapeutic pathway, shorten the length of stay and reduce hospital costs (3,4). Non-intubated procedures are not a new concept in thoracic surgery, as they were performed since the late 20 s until the introduction of mechanical ventilation in the 60 s (5). The modern application of the non-intubated technique in VATS procedures allows performing surgeries with minimal sedation without general anesthesia, maintaining throughout the operation spontaneous breathing. The principle is to create an iatrogenic spontaneous pneumothorax, which can provide a good lung isolation without the need of a double lumen tube. Amongst the advantages of non-intubated procedures, there are the lower incidence of postoperative nausea and the reduced adverse effects of intubation related injuries and ventilation induced lung injuries (6). Uniportal VATS is particularly suitable to perform in awake patients, even though coughing and patients’ movements can make this technique more challenging for both the thoracic surgeon and the anesthetist (7).
Patient selection and workup
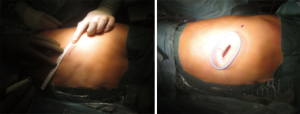
Starting a new program of non-intubated uniportal VATS should be a slow process and the patients undergoing this kind of operations should be carefully selected for minor procedures. Contraindications are related to the experience of the surgical and anesthesiological team and to the patients’ characteristics. Absolute contraindications are the inexperience of the team, a difficult airway management and the patient refusal. Relative contraindications include obesity, previous surgery or radiation with the high risk of possible adhesions and persistent cough (8) (Table 1). Patients with a reduced lung function are very good candidates as avoiding tracheal intubation will decrease the risk of tracheostomy and prolonged ventilation (9). Good results are reported in the literature for awake uniportal VATS surgery for minor and major resections. It is proven to be a feasible and safe technique in many thoracic surgery operations including lung and pleural biopsies (10,11), pleural effusions (12), surgery for pneumothorax (13), lung volume reduction surgeries (14), thymectomies (15), decortications (16,17), metastasectomies (18) and anatomical lunge resections (19-21). The risks and benefits of this technique should be evaluated individually and every patient must be eligible for intubation in case of complications or non-compliance.
Full table
Preoperative preparation
The patient should be aware of the pros and cons of this particular technique, as the patient’s cooperation is essential while performing an awake or non-intubated surgery. Patients should be informed and prepared for what is going to happen in theatre, from the positioning to the monitoring, the sedation and the possible intubation.
The team members should have experience in uniportal VATS from the surgical and anesthetic point of view. The thoracic surgeon should be proficient in VATS and the anesthetist comfortable in inserting the double lumen tube in lateral position and inducing the general anesthesia in an emergency setting. It is essential that the anesthetist responsible for the case reviews the patient well before the surgery and plans everything carefully. In particular, opening of the jaw is essential in case of emergency lateral decubitus intubation.
Likewise an accurate and thorough briefing with the surgical team is mandatory to decide position of the port, preoperative blocks and plans for emergency conversion. Non-intubated surgery should not be regarded as a technique to perform the last operation of the day quickly to avoid spending time intubating the patient. It is a procedure that requires significant skills and full anesthetist’s attention.
Equipment
Surgeon
The surgeon should have the equipment needed to perform a uniportal VATS, based on his preferences. Energy devices can help in case of adhesions and should be available in theater. Local anesthesia is an important part in non-intubated procedures, so it should always be available throughout the operation. We suggest performing preoperative paravertebral blocks under ultra-sound guidance and then block the incision site, before and after the incision with local anesthetic to avoid muscle twitching.
Anesthetist
The anesthetist and anesthetic nurse should be expert in thoracic surgery and be prepared for an emergency intubation with the patient in lateral position and conversion to general anesthesia. Single and double lumen tubes should be available, together with a bronchoscope and the anesthetic drugs.
Anesthesia
In our experience, the patient should have at least two large peripheral venous catheters, and the arterial pressure can be monitored through a 3-lead electrocardiogram or an arterial line, depending of the patient’s comorbidities. Through this line are also performed the blood gas analysis throughout the operation to monitor the blood gases, in particular for early detection of hypercapnia. Pulse oximetry should be employed as well. Figure 1 shows the positioning of the patient from the anesthetist’s point of view.
The concept of “non-intubated” varies largely in the literature as it implies the absence of the tracheal tube, but not the kind of sedation/anesthesia that the patients are receiving (22). In the majority of the latest reports, the patients are light sedated, mostly with propofol or remifentanil through a targeted-controlled infusion (23,24). The sedation is useful to reduce discomfort and anxiety during the procedure, allowing the performance of minor and major surgeries. The anesthetist should be expert in handling the sedation, as it is essential to maintain spontaneous ventilation without causing hypercapnia. Facemasks or nasal cannulas are applied to deliver oxygen. We prefer, though, to use a laryngeal mask as it protects the airways and allows rescue positive pressure ventilation.
Loco-regional anesthesia
Analgesia is a paramount element in non-intubated procedures. Classically, thoracic epidural analgesia is thought to be the most effective pain relief technique, even though it is related with a large number of complications, like haematomas and nerve injuries (25). Furthermore this technique can cause hypotension and so need of fluids, vasopressors and urinary catheter insertion. This can slow down the patients’ recovery and delay discharge; therefore this kind of analgesia is mostly avoided in enhanced recovery programs. Alternatively, other loco-regional anesthetic techniques are the intercostal nerve blocks or paravertebral blocks, which seem to provide a better outcome in this setting (8,11,26). The incision site can also be injected with a mixture of short- and long-acting local anesthetics to intensify the pain control. In the uniportal approach, only one intercostal space needs to be injected.
Surgical procedures
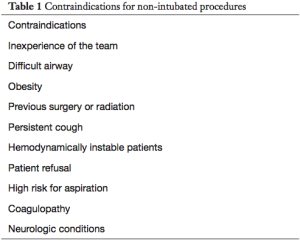
The patient is positioned in lateral decubitus position (Figure 2). Using pillows to sustain the arms gives the patient a physiological position and reduces shoulder pain postoperatively. The surgeon operates in front of the patient and the assistant can stay on the same or on the other side of the operating table. Figure 3 shows the skin incision and Figure 4 the application of the intercostal block. Non-intubated uniportal VATS can be performed in minor and major procedures. Minor procedures include:
- pleural effusions, pleural biopsies and talc pleurodesis (12,26);
- lung biopsies and wedge resections of suspect nodules (27);
- thymectomies (28);
- surgery for pneumothorax (13);
- lung volume reduction surgery (14);
- empyemas (16,17);
- metastasectomies (18).
Pleural biopsies and talc pleurodesis can be managed very easily through this technique (26), just as wedge resections for indeterminate pulmonary nodules (27). Figure 5 shows a pulmonary wedge resection of a pulmonary nodule in the left upper lobe.
Non-intubated VATS thymectomy with epidural analgesia in patients with myasthenia gravis is also reported to be beneficial, as it avoids muscle relaxants and it reduces the risk of prolonged ventilation and re-intubation (28).
Major procedures are anatomical resection like segmentectomies, lobectomies and pneumonectomies. These procedures are technically more challenging and are associated with a higher risk for complications like major bleeding. The decision to perform a non-intubated uniportal VATS major resection depends on the previous team’s experience and should only be taken if the team is already proficient in intubated VATS anatomical resections and minor non-intubated procedures. Numerous reports in the literature show that this technique is feasible and it can possibly shorten considerably the length of stay in hospital, suggesting a faster recovery when compared to intubated VATS (15,19,30). Further studies are warranted to evaluate the short- and long-term results and survival of the awake uniportal VATS anatomical resections.
Post-operative management
The combination of uniportal approach and non-intubated technique allows a minor level of invasiveness, which results in a faster recovery. In a study back in 2014, Ambrogi and Mineo compared the outcomes of patients who underwent non-intubated lung biopsies for interstitial lung disease using the uniportal VATS approach with intercostal blocks and the triportal VATS with epidural analgesia (31). The results showed that uniportal VATS with intercostal blocks was beneficial regarding the intra- and the postoperative outcomes.
In the literature, recent reports show that non-intubated uniportal VATS procedures provide less postoperative pain, an earlier mobilization and a faster discharge than intubated VATS procedures, without increasing the complication rate or the mortality (10,15,18). The enhanced recovery program for thoracic surgery has been introduced in many centers around the world. Irons and Martinez describe the postoperative ERAS protocol for non-intubated uniportal VATS at the Papworth Hospital (8). The patients are treated with intravenous fluids for 12 hours and aggressive opioid-based pain therapy. They can start to drink and eat 4 hours postoperatively and receive early physiotherapy within 12 hours. They have only one chest drain, which is connected to a digital portable drain system that facilitates early mobilization.
Tips, tricks and pitfalls
The non-intubated technique is based on an iatrogenic pneumothorax, which creates enough space to perform the surgery. The hypoxia that develops consequently is normally minimal and can be controlled using supplementary oxygen. Hypoventilation is typical in this kind of surgery and causes hypercapnia, which can be intensified from the sedation. Usually the hypercapnia is well tolerated intraoperatively and it resolves a short time after the procedure (24). As soon as the pneumothorax is induced there is a sudden tachypnea. The anesthetist must be aware of that and don’t give further analgesia/propofol otherwise the patient will stop breathing. The tachypnea is a physiological mechanism and will settle in a couple of minutes.
Cough can represent a big problem during the surgery and make the procedure more technically challenging for the surgeon. Remifentanil and off label intravenous lidocaine normally help in avoiding cough. Short acting local anesthetic can also be injected on the lung surface or in the mediastinum (i.e., vagus area) to stop the cough (8,27).
Conclusions
A survey between the members of the European Society of Thoracic Surgery (ESTS) showed that non-intubated VATS procedures are already performed by a large number of ESTS members for minor procedures (25). In Asia the application of the non-intubated technique for major procedures is already widely used (15, 32). With the publication of new data and the spreading of uniportal VATS in many centers worldwide in the last decades, the application of the non-intubated technique in major procedure like anatomic resections is expected to grow also in Europe and in USA. This technique can potentially be beneficial for high-risk patients but also could be used for the routine procedures as well, but more data are needed to establish the real benefit for these groups of patients. For the surgeons who would like to start using this technique, it is wise to begin with the minor procedures and then escalate to the anatomical resection as the team acquires enough experience. The anesthetist has a key role in this kind of procedures and the tight cooperation between surgical and anesthetic team is vital to accomplish good results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Rocco G. Non-intubated uniportal lung surgery. Eur J Cardiothorac Surg 2016;49:i3-i5. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Scarci M, Solli P, Bedetti B. Enhanced recovery pathway for thoracic surgery in the UK. J Thorac Dis 2016;8:S78-83. [PubMed]
- Migliore M, Deodato G. A single-trocar technique for minimally-invasive surgery of the chest. Surg Endosc 2001;15:899-901. [Crossref] [PubMed]
- Vischnevski AA. Local anesthesia in thoracic surgery: lungs, heart and esophagus. Minerva Anestesiol 1954;20:432-5. [PubMed]
- Cui F, Liu J, Li S, et al. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J Thorac Dis 2016;8:2226-32. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Irons JF, Martinez G. Anaesthetic considerations for non-intubated thoracic surgery. J Vis Surg 2016;2:61. [Crossref] [PubMed]
- Pompeo E. State of the art and perspectives in non-intubated thoracic surgery. Ann Transl Med 2014;2:106. [PubMed]
- Hung WT, Hsu HH, Hung MH, et al. Non-intubated uniportal thoracoscopic surgery for resection of lung lesions. J Thorac Dis 2016;8:S242-50. [PubMed]
- Pompeo E, Dauri M. Awake Thoracic Surgery Research Group. Is there any benefit in using awake anesthesia with thoracic epidural in thoracoscopic talc pleurodesis? J Thorac Cardiovasc Surg 2013;146:495-7.e1. [Crossref] [PubMed]
- Mineo TC, Sellitri F, Tacconi F, et al. Quality of life and outcomes after nonintubated versus intubated video- thoracoscopic pleurodesis for malignant pleural effusion: comparison by a case-matched study. J Palliat Med 2014;17:761-8. [Crossref] [PubMed]
- Li S, Cui F, Liu J, et al. Nonintubated uniportal video-assisted thoracoscopic surgery for primary spontaneous pneumothorax. Chin J Cancer Res 2015;27:197-202. [PubMed]
- Pompeo E, Rogliani P, Tacconi F, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg 2012;143:47-54, 54.e1
- Wang ML, Galvez C, Chen JS, et al. Non-intubated single-incision video-assisted thoracic surgery: a two- center cohort of 188 patients. J Thorac Dis 2017;9:2587-98. [Crossref] [PubMed]
- Moon EJ, Go YJ, Chung JY, et al. Non-intubated thoracoscopic surgery for decortication of empyema under thoracic epidural anesthesia: a case report. Korean J Anesthesiol 2017;70:341-4. [Crossref] [PubMed]
- Akopov A, Egorov V, Deynega I, et al. Awake video-assisted thoracic surgery in acute infectious pulmonary destruction. Ann Transl Med 2015;3:100. [PubMed]
- Mineo TC, Sellitri F, Fabbi E, et al. Uniportal non-intubated lung metastasectomy. J Vis Surg 2017;3:118. [Crossref] [PubMed]
- Liu J, Cui F, Pompeo E, et al. The impact of non-intubated versus intubated anaesthesia on early outcomes of video-assisted thoracoscopic anatomical resection in non-small-cell lung cancer: a propensity score matching analysis. Eur J Cardiothorac Surg 2016;50:920-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [Crossref] [PubMed]
- Guo Z, Shao W, Yin W, et al. Analysis of feasibility and safety of complete video-assisted thoracoscopic resection of anatomic pulmonary segments under non-intubated anesthesia. J Thorac Dis 2014;6:37-44. [PubMed]
- Hung MH, Hsu HH, Chen KC, et al. Nonintubated thoracoscopic anatomical segmentectomy for lung tumors. Ann Thorac Surg 2013;96:1209-15. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Uniportal video-assisted thoracoscopic left upper lobectomy under spontaneous ventilation. J Thorac Dis 2015;7:494-5. [PubMed]
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation. J Thorac Dis 2014;6:31-6. [PubMed]
- Pompeo E, Sorge R, Akopov A, et al. Non-intubated thoracic surgery—A survey from the european society of thoracic surgeons. Ann Transl Med 2015;3:37. [PubMed]
- Alrawi SJ, Raju R, Acinapura AJ, et al. Primary thoracoscopic evaluation of pleural effusion with local anesthesia: an alternative approach. JSLS 2002;6:143-7. [PubMed]
- Pompeo E, Mineo TC. Awake operative videothoracoscopic pulmonary resections. Thorac Surg Clin 2008;18:311-20. [Crossref] [PubMed]
- Tsunezuka Y, Oda M, Matsumoto I, et al. Extended thymectomy in patients with myasthenia gravis with high thoracic epidural anesthesia alone. World J Surg 2004;28:962-5; discussion 965-6. [Crossref] [PubMed]
- Bedetti B, Patrini D, Bertolaccini L, et al. Non-intubated uniportal VATS wedge resection of an indeterminate pulmonary nodule in the left upper lobe. Asvide 2018;5:035. Available online: http://asvidett.amegroups.com/article/view/22426
- Guo Z, Yin W, Pan H, et al. Video-assisted thoracoscopic surgery segmentectomy by non-intubated or intubated anesthesia: a comparative analysis of short-term outcome. J Thorac Dis 2016;8:359-68. [Crossref] [PubMed]
- Ambrogi V, Mineo TC. VATS biopsy for undetermined interstitial lung disease under non-general anesthesia: comparison between uniportal approach under intercostal block vs. three-ports in epidural anesthesia. J Thorac Dis 2014;6:888-95. [PubMed]
- Tacconi F, Pompeo E. Non-intubated video-assisted thoracic surgery: where does evidence stand? J Thorac Dis 2016;8:S364-75. [Crossref] [PubMed]
Cite this article as: Bedetti B, Patrini D, Bertolaccini L, Crisci R, Solli P, Schmidt J, Scarci M. Uniportal non-intubated thoracic surgery. J Vis Surg 2018;4:18.