Minimal-invasive thoracic surgery in pediatric patients
Video-assisted thoracoscopic surgery (VATS) passed through a tremendous development during the last two decades (Figure 1).
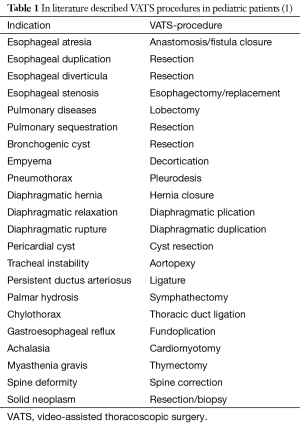
Technical and structural problems as mentioned below prolongated the introduction of this surgical technique in the treatment of pediatric patients, especially in the field of lung resection. In the terminology one speaks of minimal invasive surgery if the surgical intervention is explained only about trocar-incisions and of VATS if, in addition, one utility-incision is used. The application of VATS-procedures in children commonly is described for nearly all indications in pediatric thoracic surgery (1) (Table 1).
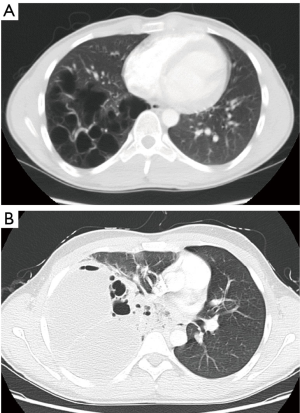
In the following representation should be entered exclusively on VAT-lung-resections in children. In thoracic surgery of adult patients’ thoracoscopic assisted lung resections are carried out most often with oncological indications. By contrast it is carried out in pediatric patients predominantly with benign diagnoses. On the one hand this is due to the fact that malignant entities seem to be more often with adults and on the other hand to the fact that the tumors are often progressed much further in children, so that an VATS is not possible any more. In practice the most frequent indication for lung resections with children is a congenital pulmonary airway malformation (CPAM) (2). In this disease, the best time for an operation is often discussed in the interdisciplinary dialogue (2). We recommend that the operation should be performed electively as far as possible, since in the case of emergency the surgical procedure is often much more difficult and the perioperative course is associated with much higher risks (Figure 2).
In large patient collectives, VATS lobectomy has proven to be a safe procedure (3). In the surgery of adults, however, a learning curve of the respective surgeon is clearly described (4). The same applies to the performance of VATS resections in childhood (5). The problem is the fact that these procedures are carried out very often in thoracic surgery departments in adults' surgery and therefore a corresponding experience can be gained quickly. In pure departments for pediatric surgery, however, the operating frequency is often not large enough to establish this method. This is why a cooperation model is offered in many places in Germany according to the motto “The doctor comes to the patient”. This means that experienced thoracic surgeons operate the children at institutions, where, in addition to departments for childhood surgery, children's intensive care facilities are available. Against this background, the question arises whether VATS lobectomy leads to measurable advantages in pediatric patients? In the review of the literature, a lower complication rate is found for the minimally invasive procedure than in open surgery (6). The average surgery time was longer in the case of thoracoscopic procedures, while the length of stay in the hospital was shorter (6).
The optimal time for elective pulmonary operations in children is discussed differently: the reasoning is primarily related to technical aspects of surgery. Above all, considerations play a role in how the available surgical technique can be applied practically and safely: if children prosper physically well, we prefer an operation time around 12–14 months of life. At this time, the classical thoracoscopic surgical technique can be used to a large extent with the aid of a “utility incision”, in particular because the thoracic cavity is then sufficiently large (Figure 3). However, there is also the opinion that the operation should be carried out as early as possible in the infant age (7). In this case, ports with valves must be used so that a permanent low pressure (4–6 mmHg) can be maintained during the operation by means of a low-flow with carbon dioxide (7). This serves to complete collapse of the lung and to increase the space for the surgical technique.

Basic requirement for all thoracoscopically-assisted lung resections in childhood is the availability of one lung ventilation. Depending on the size of the child and depending on the diameter of the respiratory tract, different ventilation strategies are available for this purpose (8).
Endoscopic stapling devices are available for the separation of lung tissue. A bipolar sealing device (LigasureTM Medtronic, Dublin, Ireland) has also proved its worth in small children and infants to complete the fissures (7). The procedure for the closure of the bronchus is also dependent on the size of the child: both separation and closure with an endo-stapler or the sharply removal is followed by a suture (monofil, resorbable). In very small children, a clipping of the bronchus with an endo clip is also possible. A special feature of the preparation in the peribronchial tissue of children is the lymph nodes. Compared to adults, they are relatively larger, consistency and often compressive. Attention must be paid to this while the vessels are prepared. Various methods and techniques are available for the closure of pulmonary vessels or a systemic artery during operation of a pulmonary sequestration: when the anatomical conditions allow, endo-staplers can be safely used. The ligature is also possible as is the application of endo clips to small vessels. In the latter case care must be taken that they are not removed during the intraoperative manipulations of the lungs. The LigasureTM, which is available in a 5-mm design, is widely used for vascular occlusion on the pulmonary arteries. Finally, there was a further development in the field of endo-stapling-devices in the size range of 5 mm with application to lung vessels and lung parenchyma of children (9).
Conclusions
Video-assisted thoracoscopic lung resections in children and infants are technically feasible and safe. There is evidence that this type of surgery provides an advantage compared to open surgery. The application is in practice limited in part by a lack of medical specialization. The surgical technique is in constant improvement and development.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Ure BM, Schmidt AI, Jesch NK. Thoracic surgery in infants and children. Eur J Pediatr Surg 2005;15:314-8. [Crossref] [PubMed]
- Kapralik J, Wayne C, Chan E, et al. Surgical versus conservative management of congenital airway malformation in children: A systematic review an meta-analysis. J Pediatr Surg 2016;51:508-12. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-55; discussion 425-6. [Crossref] [PubMed]
- Petersen RH, Hansen HJ. Learning thoracoscopic lobectomy. Eur J Cardiothorac Surg 2010;37:516-20. [Crossref] [PubMed]
- Rothenberg S.. First decade’s experience with thoracoscopic lobectomy in infants and children. J Pediatr Surg 2008;43:40-44; discussion 45. [Crossref] [PubMed]
- Adams S, Jobsen M, Sangnawakij P, et al. Does thoracoscopy have advantages over open surgery for asymptomatic congenital lung malformations? An analysis of 1626 resections. J Pediatr Surg 2017;52:247-51. [Crossref] [PubMed]
- Rothenburg SS, Middlesworth W, Kadennhe-Chiweshe A, et al. Two decades of experience with thoracoscopic lobectomy in infants and children: Standardizing techniques for advanced thoracoscopic surgery. J Laparoendosc Adv Surg Tech A 2015;25:423-8. [Crossref] [PubMed]
- Fabila TS, Menghraj SJ. One lung ventilation strategies for infants and children undergoing video assisted thoracoscopic surgery. Indian J Anaesth 2013;57:339-44. [Crossref] [PubMed]
- Rothenburg S.. Thoracoscopic lobectomy in infants and children utilizing a 5 mm stapling device. J Laparoendosc Adv Surg Tech A 2016;26:1036-8. [Crossref] [PubMed]
Cite this article as: Kugler C. Minimal-invasive thoracic surgery in pediatric patients. J Vis Surg 2018;4:10.