Anesthesia and analgesia: how does the role of anesthetists changes in the ERAS program for VATS lobectomy
Introduction
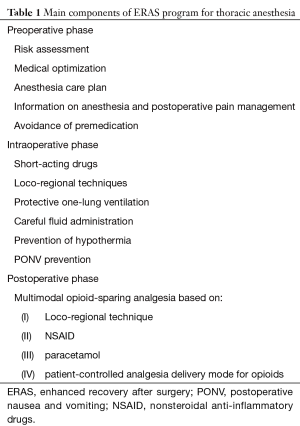
Enhanced recovery after surgery (ERAS) programs are developed to prevent factors that delay postoperative recovery as well as issues that cause complications (1,2). ERAS strategies are based on multidisciplinary approach to optimize the perioperative surgical path. The ERAS society, funded in 2001, has published many guidelines addressing the ERAS pathways for several abdominal surgeries, head and neck surgery and breast surgery (freely available at: www.erassociety.org). The development of video-assist thoracoscopic surgery (VATS) techniques favours the fast recovery after thoracic procedures. Nevertheless, there is little literature on implementation of fast track protocols in thoracic setting. To date, the thoracic noncardiac protocol has not yet been published by the ERAS Society. The purpose of this article is to report on current concepts regarding anesthesiologist’s role in the ERAS pathways for VATS lobectomy. The text is divided into three parts in relation to the three major phases of the surgical path: the preoperative, the intraoperative and the postoperative phase (Table 1).
Full table
Preoperative phase
Preoperative evaluation is essential to estimate postoperative outcome, optimize medical therapy and to identify the best perioperative strategy for the patient undergoing lung surgery (3,4). The anesthesiologist seems to be the ideal person to guide the multidisciplinary team of specialists (surgeon, pulmonologist, cardiologist, oncologist) involved in the risk assessment process (4). This approach considers the type of intervention, age, co-existing comorbidities and other risk factors with pulmonary and cardiac evaluation. These data are combined to optimize the medical therapy, if necessary, and to define the anesthetic plan. This comprises the choice of anesthetics as well as the loco-regional technique. Provide information on anesthesia and postoperative pain management strategy is useful to reduce anxiety and involve the patient in the program, especially if adding a patient-controlled regimen as part of the analgesia protocol (both regional and systemic) is planned. Finally, premedication should be avoided whenever possible. Long-acting drugs can delay postoperative recovery (5). If necessary, small incremental doses of short acting drugs (midazolam, propofol) can be administered in the operating room to facilitate loco-regional anesthetic procedures before induction of general anesthesia. ERAS programs aim to maintain euvolemia, normal cardiac output and oxygen delivery to preserve cellular function and promote tissue injury repair (1). This goal is pursued allowing intake of clear fluids and specific carbohydrate drinks until 2 hours before anesthesia. The anesthesiologist must promote this practice even it mostly depend on the endorsement of the surgical ward staff.
Intraoperative phase
The intraoperative anesthesiologist’s goals to promote ERAS are: rapid recovery from anesthetics, maintenance of homeostasis and postoperative nausea and vomit (PONV) prevention. The main parts of general anesthesia are hypnosis, analgesia and muscle relaxation. Both volatile and intravenous anesthetics result in fast recovery after surgery. Volatile anesthetics attenuate inflammatory response after one-lung ventilation (OLV) compared to intravenous anesthetics (6), but this difference did not translate in better major outcome (7,8). Currently, neither is superior to the other but total intravenous anesthesia (TIVA) is advisable in case of air loss due to dual-lumen tube or bronchial blocker malpositioning or parenchymal leakage to prevent volatile anesthetic diffusion in the operating room. Finally, propofol-based TIVA reduces PONV (9). Intraoperative analgesia is based on opioids administration and loco-regional techniques. Remifentanil has the best favourable pharmacokinetic/pharmacodynamic profile characterized by fast onset and very short context-sensitive half-life (9). Intraoperative use of loco-regional anesthesia has an opioid-sparing effect enhancing the recovery and reducing PONV. Muscle relaxation facilitates tracheal intubation, mechanical ventilation, and surgical exposure. Postoperative residual curarization (PORC) increases morbidity and prolongs recovery (10). The incidence of PORC is reduced when intermediate-acting neuromuscular blocking agents are used (11). Neuromuscular monitoring is mandatory to manage neuromuscular block and guide reversal administration. Sugammadex is the faster and safer reversal drug, when aminosteroids, such as rocuronium and vecuronium, are administered (12,13).
Anesthesiologist must also lead a “protective anesthesia” to ensure the overall homeostasis and enhance the recovery after VATS lobectomy. Mechanical ventilation and fluids are considered major risk factors for acute lung injury (ALI) if not adequately managed (14). Protective OLV is currently based on low tidal volume (4–6 mL/kg), initial low positive end-expiratory pressure (PEEP =5 cmH2O), low FiO2 (15). This approach aims to minimize the ventilator-induced lung injury (VILI) due to mechanical, inflammatory and oxidative stress (16). The treatment of hypoxemia (if the tracheal tube is correctly positioned) is primarily based on optimization of lung ventilation using alveolar recruitment maneuvers and setting the best PEEP level (15,17).
With regard to fluid administration, liberal regimen predisposes to fluid overload and ALI while an excessive restrictive management may result in acute kidney injury (18). Zero fluid balance state is the main target to enhance recovery and improve outcomes (19,20). Today, there is no consensus on the best approach for management of fluid therapy during thoracic surgery. Some authors propose a maintenance basal fluid infusion equal to 1.5 mL/kg/h (18) and to avoid a total crystalloids infusion of 2 L (21). Balanced crystalloids are the first choice fluids while colloids should be used to replace intraoperative losses. Rational management of fluid and vasopressors administration is often based on goal-directed protocols using hemodynamic parameters. Unfortunately, dynamic indices of fluid responsiveness like pulse pressure variation or stroke volume variation are not reliable in open chest condition (22). Similarly, the accuracy of transpulmonary thermodilution system for extravascular lung water in lung resection surgery is controversial (21,23). Thus, the best pragmatic approach is probably to use hemodynamic parameters like arterial pressure, cardiac output (and stroke volume) as well blood lactate and central venous oxygen saturation to estimate oxygen delivery adequacy. Finally, transesophageal echocardiography can be used to evaluate a complex hemodynamic scenario and select the proper treatment (24).
Other crucial intraoperative issues are prevention of hypothermia and PONV. Hypothermia increases bleeding, cardiovascular complications and wound infections (25-27). The patient’s temperature should be always monitored and forced-air and fluid warming system used to counteract intraoperative-induced hypothermia. PONV prophylaxis is fundamental to enhance recovery after general anesthesia. The Apfel score is useful to stratify patients from low-to-high risk for PONV (28) and guide antiemetic prophylaxis. A multimodal approach to PONV should be adopted for all patients (29). The most used antiemetics are dexamethasone, ondansetron and droperidol (30,31).
Finally, postoperative analgesia already begins in the operating room. Intraoperatively, the anesthesiologist uses a multimodal approach based on loco-regional technique with nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol, opioids to encourage the best possible awakening from anesthesia (32). During the intervention, N-methyl-D-aspartate (NMDA) antagonists like ketamine and magnesium sulphate can reduce the risk of opioid induced hyperalgesia decreasing postoperative pain and opioid consumption (33,34). Currently, there are no data on the efficacy of NMDA-antagonists in the context of pain treatment after VATS lobectomy.
Postoperative phase
In the ERAS pathway, from the anesthesiologist’s point of view, acute pain management is the most important postoperative issue. Adequate pain relief is mandatory for enhance recovery because it allows early mobilization, feeding and upturn of gastrointestinal function. The most effective strategy to face the pain is the multimodal approach (32,35,36). It consists in the concomitant use of different analgesic drugs with distinct nociceptive target to enhance the effect of each drug reducing side effects. This concept is extremely important in ERAS protocols to guarantee the greatest pain relief together with opioid-sparing effect (37,38).
The main components of multimodal analgesia are: NSAIDs, paracetamol, opioids and regional analgesia. The goal is to take advantage of several analgesia techniques to minimize the consumption of opioids. NSAIDs and paracetamol reduce opioids demand, postoperative sedation and PONV (39-42). They should always be part of a multimodal pain treatment and administered on a scheduled basis. NSAIDs may be associated with kidney disfunction, gastrointestinal bleeding, and platelet disfunction but there is no evidence of increased postoperative risk of bleeding due to these agents (43). Opioids are used for intraoperative and postoperative analgesia. The opioid-sparing aim of ERAS protocols can’t totally exclude their use, if needed. Given the great interindividual pharmacokinetic and pharmacodynamic variability of opioids, their intravenous continuous infusion or intramuscular administration should be avoided in favour of patient-controlled analgesia (PCA) modality (35). PCA systems allow to individualize opioid consumption contributing to the decrease of opioid-related side effects like hypotension, respiratory depression, itching, PONV, bowel ileus and sedation (44,45). Morphine is the most used opioid to treat acute postoperative pain but, for minimally invasive surgery like VATS, even weak opioids like tramadol and codeine are suitable.
In all ERAS programs, the cornerstone of acute pain management after major surgery is epidural analgesia (2,32,37). Thoracic epidural analgesia (TEA) is recommended as the goal standard technique for pain treatment following thoracotomy (46,47). TEA provides better postoperative analgesia compared with parenteral opioids (48) but it can’t be used in some circumstances (i.e., use of anticoagulants, coagulopathy, spine deformity) and requires proper management in the ward due to issues like hypotension, respiratory depression, urinary retention, and motor block. These limitations have promoted the development of alternative regional techniques. The most efficacious one is thoracic paravertebral block (TPVB). TPVB has a higher safety profile and less side effects than TEA (49,50). After thoracotomy, TPVB is associated with pain relief, major complications, length of hospital stay and 30-day mortality comparable to TEA (49). For these reasons, TPVB is considered the ideal choice for pain management after VATS (51). TPVB can be performed with several techniques: the blind, the ultrasound-guided or the surgical approach. No study has compared these approaches but, currently, the ultra-sound technique seems the preferable. The search for less invasive techniques has led to the proposal of new approaches like the retrolaminar block (RLB) and the mid-point transverse process to pleura (MTP) block (52,53). Both techniques aim to inject the local anesthetic near the paravertebral space but farther away from the pleura and the epidural space. They can be considered “indirect” paravertebral blocks but are not suitable for the placement of a catheter for continuous infusion. Presently, there is no evidence for the use of RLB and MTP block for pain management after VATS lobectomy. Other regional techniques for analgesia after VATS include the intercostal nerve block (ICNB) and the serratus anterior plane block (SAPB). ICNB is a good alternative to TEA and TPVB, if combined with PCA therapy (46). SAPB has been recently proposed for breast surgery (54) but new data are emerging on its efficacy for pain management after thoracic surgery too (55-57). SAPB advantages include ease of execution (under ultrasound guidance) and peripheral action. However, more studies are needed to confirm its role in the context of the VATS lobectomy analgesia. Erector spinae plane (ESP) block is another interesting newly described technique for thoracic analgesia (58). The injection of local anesthetic deep to the erector spinae muscles at T5 level has provided pain relief for thoracic neuropathic pain, ribs fractures and thoracotomy after TEA failure (59,60). Despite its promising results, the limited experience with the ESP block does not yet allow to recommend its use for analgesia after VATS lobectomy.
In summary, many regional analgesic techniques are suitable for pain management after VATS lobectomy. The minimally invasiveness of VATS suggests to reduce both the invasiveness of loco-regional techniques and the potency or dosage of opioids. TPVB is considered the first choice regional technique in this context but ICNB and SAPB can be valuable alternative even if they predispose more easily to the need of opioids. Other techniques, like the ESP block, seem to be able to become alternatives to TPVB in the future. Alongside to regional techniques and opioids, the multimodal analgesia must always comprise one NSAID and paracetamol on a scheduled basis (Figure 1).

Conclusions
Careful evaluation of single patient and planning of the anesthetic care are mandatory to join the ERAS philosophy in the era of VATS lobectomy. Preoperative optimization, minimization of side effects of anesthetics and analgesics, protective OLV, careful fluids administration and multimodal analgesia protocol are the goals that anesthetists must achieve to adhere to an ERAS program.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-8. [Crossref] [PubMed]
- Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of Fast-track surgery. Ann Surg 2008;248:189-98. [Crossref] [PubMed]
- Licker M, Triponez F, Diaper J, et al. Preoperative evaluation of lung cancer patients. Curr Anesthesiol Rep 2014;4:124-34. [Crossref]
- Della Rocca G, Vetrugno L, Coccia C, et al. Preoperative evaluation of patients undergoing lung resection surgery: defining the role of the anesthesiologist on a multidisciplinary team. J Cardiothorac Vasc Anesth 2016;30:530-8. [Crossref] [PubMed]
- Walker KJ, Smith AF. Premedication for anxiety in adult day surgery. Cochrane Database Syst Rev 2009.CD002192. [PubMed]
- Sun B, Wang J, Bo L, et al. Effects of volatile vs. propofol-based intravenous anesthetics on the alveolar inflammatory responses to one-lung ventilation: a meta-analysis of randomized controlled trials. J Anesth 2015;29:570-9. [Crossref] [PubMed]
- Módolo NSP, Módolo MP, Marton MA, et al. Intravenous versus inhalation anaesthesia for one-lung ventilation. Cochrane Database Syst Rev 2013.CD006313. [PubMed]
- Beck-Schimmer B, Bonvini JM, Braun J, et al. Which anesthesia regimen is best to reduce morbidity and mortality in lung surgery? A multicenter randomized controlled trial. Anesthesiology 2016;125:313-21. [Crossref] [PubMed]
- Mandel JE. Considerations for the use of short-acting opioids in general anesthesia. J Clin Anesth 2014;26:S1-7. [Crossref] [PubMed]
- Butterly A, Bittner EA, George E, et al. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth 2010;105:304-9. [Crossref] [PubMed]
- Donati F.. Residual paralysis: a real problem or did we invent a new disease? Can J Anaesth 2013;60:714-29. [Crossref] [PubMed]
- Carron M, Zarantonello F, Tellaroli P, et al. Efficacy and safety of sugammadex compared to neostigmine for reversal of neuromuscular blockade: a meta-analysis of randomized controlled trials. J Clin Anesth 2016;35:1-12. [Crossref] [PubMed]
- Carron M, Zarantonello F, Lazzarotto N, et al. Role of sugammadex in accelerating postoperative discharge: a meta-analysis. J Clin Anesth 2017;39:38-44. [Crossref] [PubMed]
- Licker M, Fauconnet P, Villiger Y, et al. Acute lung injury and outcomes after thoracic surgery. Current Opinion in Anaesthesiology 2009;22:61-7. [Crossref] [PubMed]
- Bernasconi F, Piccioni F. One-lung ventilation for thoracic surgery: current perspectives. Tumori 2017;103:495-503. [Crossref] [PubMed]
- Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg 2015;121:302-18. [Crossref] [PubMed]
- Della Rocca G, Coccia C. Acute lung injury in thoracic surgery. Curr Opin Anaesthesiol 2013;26:40-6. [Crossref] [PubMed]
- Assaad S, Popescu W, Perrino A. Fluid management in thoracic surgery. Curr Opin Anaesthesiol 2013;26:31-9. [Crossref] [PubMed]
- Brandstrup B, Svendsen PE, Rasmussen M, et al. Which goal for fluid therapy during colorectal surgery is followed by the best outcome: near-maximal stroke volume or zero fluid balance? Br J Anaesth 2012;109:191-9. [Crossref] [PubMed]
- Gupta R, Gan TJ. Peri-operative fluid management to enhance recovery. Anaesthesia 2016;71:40-5. [Crossref] [PubMed]
- Chau EHL, Slinger P. Perioperative fluid management for pulmonary resection surgery and esophagectomy. Semin Cardiothorac Vasc Anesth 2014;18:36-44. [Crossref] [PubMed]
- Piccioni F, Bernasconi F, Tramontano GTA, et al. A systematic review of pulse pressure variation and stroke volume variation to predict fluid responsiveness during cardiac and thoracic surgery. J Clin Monit Comput 2017;31:677-84. [Crossref] [PubMed]
- Michard F.. Bedside assessment of extravascular lung water by dilution methods: temptations and pitfalls. Crit Care Med 2007;35:1186-92. [Crossref] [PubMed]
- Vincent JL, Pelosi P, Pearse R, et al. Perioperative cardiovascular monitoring of high-risk patients: a consensus of 12. Critical Care 2015;19:224. [Crossref] [PubMed]
- Kristensen SD, Knuuti J, Saraste A. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management. The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 2014;35:2383-431. [Crossref] [PubMed]
- Devereaux PJ, Sessler DI. Cardiac complications in patients undergoing major noncardiac surgery. N Engl J Med 2015;373:2258-69. [Crossref] [PubMed]
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg 2017;152:784-91. [Crossref] [PubMed]
- Apfel CC, Kranke P, Eberhart LH, et al. Comparison of predictive models for postoperative nausea and vomiting. Br J Anaesth 2002;88:234-40. [Crossref] [PubMed]
- Chandrakantan A, Glass PS. Multimodal therapies for postoperative nausea and vomiting, and pain. Br J Anaesth 2011;107:i27-40. [Crossref] [PubMed]
- Habib AS, El-Moalem HE, Gan TJ. The efficacy of the 5-HT3 receptor antagonists combined with droperidol for PONV prophylaxis is similar to their combination with dexamethasone. A meta-analysis of randomized controlled trials. Can J Anaesth 2004;51:311-9. [Crossref] [PubMed]
- Carlisle JB, Stevenson CA. Drugs for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev 2006.CD004125. [PubMed]
- Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 2017;152:691-7. [Crossref] [PubMed]
- Bell RF, Dahl JB, Moore RA, et al. Perioperative ketamine for acute postoperative pain. Cochrane Database Syst Rev 2006.CD004603. [PubMed]
- De Oliveira GS Jr, Castro-Alves LJ, Khan JH, et al. Perioperative systemic magnesium to minimize postoperative pain: ameta-analysis of randomized controlled trials. Anesthesiology 2013;119:178-90. [Crossref] [PubMed]
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Re- gional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016;17:131-57. [Crossref] [PubMed]
- Savoia G, Alampi D, Amantea B, et al. Postoperative pain treatment SIAARTI recommendations 2010: short version. Minerva Anestesiol 2010;76:657-67. [PubMed]
- Beverly A, Kaye AD, Ljungqvist O, et al. Essential elements of multimodal analgesia in enhanced recovery after surgery (ERAS) Guidelines. Anesthesiol Clin 2017;35:e115-43. [Crossref] [PubMed]
- Kumar K, Kirksey MA, Duong S, et al. A review of opioid-sparing modalities in perioperative pain management: methods to decrease opioid use postoperatively. Anesth Analg 2017;125:1749-60. [Crossref] [PubMed]
- Elia N, Lysakowski C, Tramèr MR. Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology 2005;103:1296-304. [Crossref] [PubMed]
- Boussofara M, Mtaallah MH, Bracco D, et al. Co-analgesic effect of ketoro- lac after thoracic surgery. Tunis Med 2006;84:427-31. [PubMed]
- Memis D, Inal MT, Kavalci G, et al. Intravenous paracetamol reduced the use of opioids, extubation time, and opioid-related adverse effects after major surgery in intensive care unit. J Crit Care 2010;25:458-62. [Crossref] [PubMed]
- Apfel CC, Turan A, Souza K, et al. Intravenous paracetamol reduces postoperative nausea and vomiting: a systematic review and meta-analysis. Pain 2013;154:677-89. [Crossref] [PubMed]
- Gobble RM, Hoang HL, Kachniarz B, et al. Ketorolac does not increase perioperative bleeding: ameta-analysis of randomized controlled trials. Plast Reconstr Surg 2014;133:741-55. [Crossref] [PubMed]
- Palmer PP, Miller RD. Current and developing methods of patient- controlled analgesia. Anesthesiol Clin 2010;28:587-99. [Crossref] [PubMed]
- Kolettas A, Lazaridis G, Baka S, et al. Postoperative pain management. J Thorac Dis 2015;7:S62-72. [PubMed]
- Elmore B, Nguyen V, Blank R, et al. Pain Management Following Thoracic Surgery. Thorac Surg Clin 2015;25:393-409. [Crossref] [PubMed]
- Loop T.. Fast track in thoracic surgery and anaesthesia: update of concepts. Curr Opin Anaesthesiol 2016;29:20-5. [Crossref] [PubMed]
- Block BM, Liu SS, Rowlingson AJ, et al. Efficacy of Postoperative Epidural Analgesia: a meta-analysis. JAMA 2003;290:2455-63. [Crossref] [PubMed]
- Yeung JHY, Gates S, Naidu BV, et al. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev 2016;2:CD009121. [PubMed]
- Kosiński S, Fryzlewicz E, Wilkojc M, et al. Comparison of continuous epidural block and continuous paravertebral block in postoperative analgaesia after video-assisted thoracoscopic surgery lobectomy: a randomised, non-inferiority trial. Anaesthesiol Intensive Ther 2016;48:280-7. [PubMed]
- Kaplowitz J, Papadakos PJ. Acute pain management for video-assisted thoracoscopic surgery: an update. J Cardiothorac Vasc Anesth 2012;26:312-21. [Crossref] [PubMed]
- Voscopoulos C, Palaniappan D, Zeballos J, et al. The ultrasound-guided retrolaminar block. Can J Anaesth 2013;60:888-95. [Crossref] [PubMed]
- Costache I, de Neumann L, Ramnanan CJ, et al. The mid-point transverse process to pleura (MTP) block: a new end-point for thoracic paravertebral block. Anaesthesia 2017;72:1230-6. [Crossref] [PubMed]
- Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound- guided thoracic wall nerve block. Anaesthesia 2013;68:1107-13. [Crossref] [PubMed]
- Khalil AE, Abdallah NM, Bashandy GM, et al. Ultrasound-Guided Serratus Anterior Plane Block Versus Thoracic Epidural Analgesia for Thoracotomy Pain. J Cardiothorac Vasc Anesth 2017;31:152-8. [Crossref] [PubMed]
- Ökmen K, Ökmen BM. The efficacy of serratus anterior block in analgesia for thoracotomy: a retrospective study. J Anesth 2017;31:579-85. [Crossref] [PubMed]
- Ökmen K, Ökmen BM. Evaluation of serratus anterior plane block for pain treatment after Video-assisted thoracoscopic surgery. Anaesth Crit Care Pain Med 2017. [Epub ahead of print]. [PubMed]
- Forero M, Rajarathinam M, Adhikary S, et al. Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: a case series. Scand J Pain 2017;17:325-9. [PubMed]
- Hamilton DL, Manickam B. Erector spinae block for pain relief in rib fractures. Br J Anaesth 2017;118:474-5. [Crossref] [PubMed]
- Forero M, Rajarathinam M, Adhikary S, et al. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: a case report. A A Case Rep 2017;8:254-6. [Crossref] [PubMed]
Cite this article as: Piccioni F, Ragazzi R. Anesthesia and analgesia: how does the role of anesthetists changes in the ERAS program for VATS lobectomy. J Vis Surg 2018;4:9.


