Thoracoscopic anatomic lung resections for cancer in patients with previous cardiac surgery
Introduction
Video-assisted thoracoscopic surgery (VATS) lobectomy is become the preferred approach for resection of early stage lung cancer. With increasing experience in VATS, this strategy has been also used in more complex procedures. Herein, we reported the feasibility of VATS anatomical resections for lung cancer in consecutive series of patients undergoing previous history of cardiac surgery.
Study population
Study population included four consecutive patients (Table 1) scheduled for VATS resection for early stage lung cancer in two high volume Italian centres. All patients underwent previous cardiac surgeries as coronary artery by-pass graft (CABG) using left internal mammary artery (LIMA) graft (n=1), cardiac transplantation (n=2), and mitral valve replacement (n=1). The median interval between cardiac operations and lung resections was 71 [36–180] months.
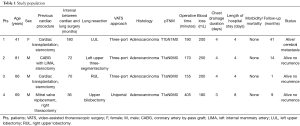
Full table
Surgical technique
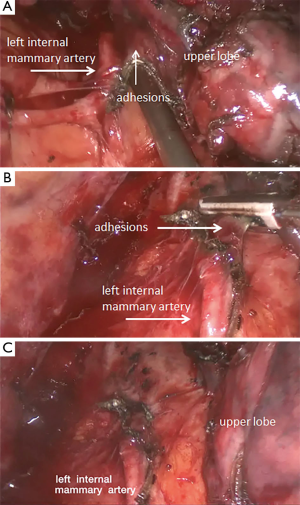
All procedures were performed under general anaesthesia and using selective-one lung ventilation. The surgeon and his assistant stand anterior to the patient. In three patients, a three-port approach was used with a 3–4 cm utility incision made through the 4th or 5th intercostal space just anterior to the latissimus dorsi muscle; a 10-mm camera port inserted at the anterior axillary line at the 7th intercostal space and the third port placed at the posterior axillary line at the 7th–8th intercostal space. In patient 4, an uniportal approach was used with a single 4–5 cm incision made through the 4th or 5th intercostal space just anterior to the latissimus dorsi muscle. The initial step was to lyse all adhesions related to sternotomy or thoracotomy that attached the lung parenchyma to the mediastinum, diaphragm and chest wall. In patient 2, additional adhesions were lysed between the LIMA graft and upper lobe (Figure 1). Then, in all cases anatomic resection with individual ligation of arteries, veins and bronchus was performed in a standard manner. Lobectomy was carried out in patient 1 and in patient 3; in patient 2 a left upper three-segmentectomy instead of left upper lobectomy was carried due to respiratory reserve; and in patient 4 an upper bilobectomy instead of right upper lobectomy was performed for surgical clearance since the tumor branched the horizontal fissure. The specimen was retrieved through the utility incision in an endoplastic bag. A systematic lymph node dissection completed the operation and a single 28 Fr. drainage was left in pleural cavity. Examples are reported in Figure 2 (patient 2) and in Figure 3 (patient 3).
Results
In all cases, the procedure was performed using VATS without needing conversion to thoracotomy. The resection of the adhesions related to previous sternotomy and thoracotomy and hilar dissection were carried out without particular technical problem using blunt dissection and/or vessel-sealing device (Ligasure, Valleylab, Colorado, United States) or ultrasonic-driven scalpel (Ultracision, Ethicon, Cincinnati, United States) according to surgeon’s preference. The median operative time and estimated blood loss was 180 [155–405] minutes and 200 [180–250] mL, respectively; the median chest drainage duration and length of hospital stay were 4 [3–4] days, and 4 [4–8] days, respectively. No injury of the heart and of the LIMA graft occurred during the operation. No cardiac or other post-operative complications were recorded. At last follow-up [median follow-up:16 (1–41) months], all patients were alive without recurrence but patient 1 who presented cerebral metastasis two months ago and underwent radiotherapy.
Discussion
The main concern of VATS lobectomy in patients undergoing previous cardiac surgery is the presence of intra-thoracic adhesions that may lead to difficult recognition of anatomy and risk of injuring to the heart or to the internal mammary artery (IMA) graft during hilum dissection. However, VATS anatomical resection remains a feasible procedure also in this groups of patients as reported by recent reports (3,4). Serna-Gallegos et al. (3) performed VATS lobectomy in 87 patients with a history of cardiac surgery. The conversion rate was 16.1% (14/87) and no intraoperative mortality was found. Similarly, Shah et al. (4) carried out VATS lobectomy in 14 patients undergoing previous CABG with ipsilateral IMA graft. The conversion rate was 7% (1/14); post-operative morbidity, mortality and survival were similar to the control group.
Despite more limited, also our experience confirmed these results. The main challenge of VATS was represented by patient 3 undergoing LIMA. In this patient, the pleura was previously opened and drained; therefore, such situation promoted dense adhesions between the lung and the grafts that was challenging to dissect. Despite some authors (4-6) proposed to leave some lung tissue attached to the LIMA graft to reduce the risk of graft injury during the dissection, however we separated the graft from the lung using vessel-sealing device (Ligasure, Valleylab, Colorado, US) that allowed a safe dissection of the adhesions. In theory, this strategy could reduce the risk of local recurrence and/or infection since devitalized lung parenchyma was not leave attached to the graft. Conversely, in the remaining cases we did not find specific difficulties to perform VATS resections. In patient 1 and patient 3 undergoing cardiac transplantation, the pleura was not opened and in patient 4 undergoing mitral valve repair, even if it was opened, the adhesions of pleura remained limited and they did not increase significantly the surgical difficulties for a VATS resection (7,8).
For the success of the procedure, the selection of patients is mandatory. An accurate review of chest computed tomography (CT) scan allows identifying the adhesions and guides the resection. In patients undergoing CABG, a pre-operative magnetic resonance imaging (MRI) or CT-angiography of heart should be performed to define the exact graft location and its patency. From a technical point of view, all adhesions that fix the lung parenchyma to the mediastinum and to the chest wall and/or diaphragm should be lysed before hilar dissection. This maneuver could be initially performed through the utility incision in the 4th and 5th intercostal space in order to create then enough space to allow placement of a trocar and a camera to lyse the residual adhesions. In patients undergoing CABG, if the proper plane between graft and lung parenchyma is not clear for the presence of dense adherences, leaving some lung tissue attached to the graft may be a safe alternative to preserve the graft. On the other hand, if the preoperative exams show an occluded graft, it could be also resected without any cardiac complications (9). In case of bleeding or graft injury, emergent thoracotomy is required and cardiac surgical team should be mobilized to aid in revising the graft and/or performing a redo-CABG as needed. Thus, such operations need to be performed in centers where cardiac surgery is available. A cardiac surgeon must be informed that this type of procedure is performed and therefore he should be in stand-by for the safety of the patients. In addition, the legs of the patients with saphenous veins should be prepared in order to have rapidly an available graft in case of CABG injury. This preliminary precaution is very useful and may change the prognostic of a difficult cardiac situation. Hilar and mediastinal adhesions too dense for safe dissection are an absolute contraindication for VATS resection and in these cases conversion to thoracotomy is mandatory.
VATS over thoracotomy presented well-defined advantages including short length of hospital stay, less postoperative pain, better postoperative lung function, and equivalent oncologic results (10). Patients undergoing previous cardiac procedures are treated with immunosuppressive therapy and/ or anticoagulant therapy and they are at higher risk of postoperative complications as pneumonia or empyema compared to normal patient. Thus, this strategy could be particularly indicated in this group of patients to reduce the surgical trauma and to facilitate healing, recovery and early return to daily activities.
Conclusions
VATS resection in patients undergoing cardiac procedure is a feasible but complex procedure with a reported mortality rate of 5.7% and a conversion rate of 15.9% (1,2). Thus, it should be performed in hospitals with high experience in VATS and having a cardiac surgery team ready to manage injury to CABG.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Fiorelli A, Amore D, Mendogni P, et al. The video edited the main steps of left upper three-segmentectomy for lung adenocarcinoma in 81-year-old man undergoing previous coronary artery by-pass graft with left internal mammary artery. Asvide 2017;4:539. Available online: http://www.asvide.com/articles/1896
- Fiorelli A, Amore D, Mendogni P, et al. The video edited the main steps of right upper lobectomy for lung adenocarcinoma in 61-year-old man undergoing cardiac transplant. Asvide 2017;4:540. Available online: http://www.asvide.com/articles/1897
- Serna-Gallegos DR, Merry HE, McKenna RJ Jr. Video-assisted thoracic surgery in patients with previous sternotomy and cardiac surgery. Innovations (Phila) 2017;12:15-20. [Crossref] [PubMed]
- Shah AA, Worni M, Onaitis MW, et al. Thoracoscopic left upper lobectomy in patients with internal mammary artery coronary bypass grafts. Ann Thorac Surg 2014;98:1207-12. [Crossref] [PubMed]
- Santini M, Fiorello A, Vicidomini G, et al. The use of LigaSure for preservation of a previous coronary artery bypass graft by using the left internal thoracic artery in a left upper lobectomy. J Thorac Cardiovasc Surg 2008;136:222-3. [Crossref] [PubMed]
- Halkos ME, Sherman AJ, Miller JI Jr. Preservation of the LIMA pedicle after cardiac surgery in left upper lobectomy. Ann Thorac Surg 2003;76:280-1. [Crossref] [PubMed]
- Abi Jaoude W, Tiu B, Strieter N, et al. Thoracoscopic native lung pneumonectomy after single lung transplant: initial experience with 2 cases. Eur J Cardiothorac Surg 2016;49:352-4. [Crossref] [PubMed]
- Decaluwe H, Van Raemdonck D, Verleden G, et al. Thoracoscopic lobectomy after bilateral lung transplantation. Interact Cardiovasc Thorac Surg 2014;19:515-7. [Crossref] [PubMed]
- Serna-Gallegos D, Merry H, McKenna RJ Jr. Video-assisted thoracic surgery after median sternotomy for cardiac surgery. Thorac Surg Clin 2015;25:349-54. [Crossref] [PubMed]
- Caronia FP, Fiorelli A, Ruffini E, et al. A comparative analysis of Pancoast tumour resection performed via video-assisted thoracic surgery versus standard open approaches. Interact Cardiovasc Thorac Surg 2014;19:426-35. [Crossref] [PubMed]
Cite this article as: Fiorelli A, Amore D, Mendogni P, Tosi D, Nosotti M, Santini M, Curcio C. Thoracoscopic anatomic lung resections for cancer in patients with previous cardiac surgery. J Vis Surg 2017;3:188.


