Uniportal lobectomy and segmentectomy—is it for all?
Introduction
Management of lung cancer has evolved significantly over the last 2 decades. Ginsberg’s landmark trial in 1995, especially, set the stage for management of early-stage lung cancer, and lobectomy became widely adopted as the gold standard treatment approach (1,2). In recent years, video-assisted thoracoscopic surgery (VATS) has emerged as a viable alternative to open approaches, with comparable long-term outcomes, and overall oncologic efficacy for early-stage non-small cell lung cancers (2,3).
With advancements in imaging modalities, and as institutional experience in thoracoscopic techniques accrues, there has also been a widespread interest and adoption of VATS approaches in various areas of thoracic surgery including lobectomy, pneumonectomy, esophagectomy, anterior mediastinal surgery, and mediastinal lymph node dissections (2,4-6). Likewise, the advent of more sophisticated dissection tools has been an impetus for technical innovations in thoracoscopic approaches, especially uniportal VATS. These innovative approaches are promising, however, data on their efficacy is still limited. Nonetheless, the lessons learned from experience with the 2-port and 3-port VATS lobectomy and segmentectomy can be applied to further improve the efficacy of uniportal approaches, in terms of achieving oncologic efficacy and improving patient outcomes. In this perspective, we review contemporary outcomes of uniportal lobectomy and segmentectomy, highlight our institutional experience, and examine various aspects that would impact widespread adoption of this innovative technique.
Contemporary outcomes
The role of VATS approaches has become increasingly important in the current era in the management of primary lung tumors (7,8). The emergence of video-mediastinoscopy and thoracoscopic mediastinal lymph node dissection has also been shown to play a pivotal role in improving the accuracy of staging of patients (7,8). While there is no standardized approach for VATS, the most common or conventional approaches in many institutions include either the 2-incision or the 3-incision approaches (9,10).
The concept of uniportal VATS was first developed by Rocco and his colleagues for various diagnostic and therapeutic procedures in the early 2000s (11,12). Their initial experiences with 15 patients who underwent wedge resections, either for interstitial lung disease or treatment of primary spontaneous pneumothoraces, was promising (11,12). Similar to multiportal VATS, as experience with basic procedures accumulated over time, more complex procedures evolved through this approach. Gonzalez-Rivas and his colleagues first reported their experience with uniportal VATS lobectomy in 2010 (13,14). In the initial series of 134 patients, the authors demonstrated outstanding results, with a low conversion rate (only six patients) (14). Over the last 5 years, this group has further refined their technique for uniportal lobectomy, and also demonstrated the safety of uniportal VATS segmentectomy. For instance, in their series of 17 patients with median tumor size was 2.3 cm, they had no conversions, and with chest tube duration of 1.5 days (range, 1–4 days) and length of stay of 2 days (range, 1–6 days) (15). With increasing expertise, this group have also demonstrated the role of uniportal VATS in increasingly advanced and complex cases (16).
Likewise, Wang et al. demonstrated their uniportal VATS experience in 14 lobectomy and 5 segmentectomy patients with radical mediastinal lymph node dissection (all performed through a single incision of 3–5 cm) and found no conversions and no 30-day mortality (17). More recently, Wang and his colleagues demonstrated no significant differences in operative times, blood loss, number of lymph nodes retrieved, drainage times, length of stay or postoperative complications between patients undergoing either uniportal, 2-port or traditional 3-port VATS lobectomy (18).
While the safety and efficacy of the uniportal approach has clearly been demonstrated, the potential advantages of a single port as compared to multi-port approaches have not been fully studied. A recent systematic review and meta-analysis was performed, identifying eight observational studies (19). Uniportal VATS lobectomy was associated with reduction in rate of complications, length of stay, and chest tube duration (19). However, in a prospective, randomized trial that compared uniportal versus the 2-port approaches, there was no difference in operative or 30-day mortality and no difference in median morphine use within first 3 days or duration of hospital stay (20).
In addition to transthoracic uniportal lobectomy, other single port approaches have also been reported, including sub-xiphoid uniportal VATS approaches and subcostal VATS, although further studies are needed to assess their overall efficacy compared to the traditional VATS approach (15,21,22). While initial studies are encouraging, the outcome advantages for the uniportal VATS still approach remain unknown. Moreover, studies examining pain and quality of life differences between uniportal and multiport VATS are required to determine any benefit other than cosmetic.
Surgical indications
Indications for uniportal lobectomy and segmentectomy are fundamentally similar to conventional 2- or 3-port VATS approaches. The indications for VATS lobectomy are basically the same as those for conventional lobectomy, including non-small cell lung cancer, metastatic cancer, and carcinoid tumors. Patients with presence of T4 tumors are often not ideal candidates for VATS lobectomy as they require a more systematic and direct approach to resection in order to achieve R0 resection.
Similarly, there are certain clinical situations in which a segmentectomy is the preferred operation. Segmentectomy is reasonable in patients with peripheral T1N0, less than or equal 2 cm tumors with concurrent limited cardiopulmonary reserve, or synchronous lung primary tumors. This cohort can include patients with pure ground glass opacities that are less than 2 cm, and those with co-existing other comorbidities such as age and frailty. These indications can also be translated reasonably to patients with semi-solid lesions. Additionally, for ground glass lesions, the risk of nodal or distant metastasis is very low and thus parenchymal preservation approach is ideal, especially in view of heightened probability of multi-focality with these lesions.
Our institutional experience
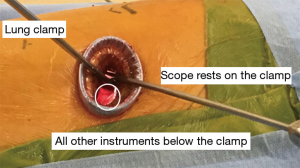
While some may argue that the uniportal lobectomy is better for lower lobes compared to upper lobes, this technique does require more skill and experience. Likewise, the difficulty also arises in managing and optimizing multiple instruments, including the camera, through the same incision (18,21-24). In some cases, the surgeon may need to navigate the camera. Likewise, the concept of “direct visualization” is irrelevant because the camera can always be moved from another incision to the access incision.
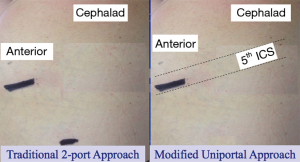
Our institution has utilized three approaches: 2-port, modified uniportal (Figure 1), and classic uniportal (Figure 2). The standard 2-incision approach for VATS, which includes 1-camera port incision (made in the 8th intercostal space along posterior axillary line), and the 4-cm anterior access incision (made in the 5th intercostal space along the anterior axillary line where the ribs are widest. Our technique has been described in detail previously (9).
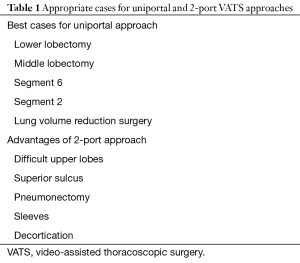
In the modified uniportal VATS approach (Figure 1) (23), a 4-cm anterior access incision is made in the 5th intercostal space but the space is opened approximately 1-cm more anterior and posterior than the extent of the skin incision. At the same time, small 5-mm counter-incision in the same interspace adjacent to the operating incision is made, which helps to keep the camera separate from the operating instruments, and gives the chest tube its own incision. We believe this modified approach may be more reasonable and address some of the disadvantages perceived with uniportal VATS approaches. Furthermore, with experience, we have been able to select appropriate cases for each approach (Table 1).
Full table
Future directions and challenges
Technological advances have markedly transformed the philosophy of thoracic surgery and have improved patient outcomes with VATS surgery. While recent innovations in uniportal VATS approaches have been promising, data on long-term patient and oncologic outcomes are limited and in some cases, discrepant. Thus, a comprehensive analysis of outcomes, and comparison to 2-port and multiport VATS approaches, will provide a more robust foundation for future improvement in techniques. Importantly, specific training in uniportal VATS is critical, which may be achieved by direct interaction with experienced surgeons in high-volume centers or simulation training for future trainees (25). There is indeed significant room for improvement as these innovations continue to evolve.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Yang CJ, Kumar A, Klapper JA, et al. A National Analysis of Long-term Survival Following Thoracoscopic Versus Open Lobectomy for Stage I Non-small-cell Lung Cancer. Ann Surg 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Yang CF, D'Amico TA. Open, thoracoscopic and robotic segmentectomy for lung cancer. Ann Cardiothorac Surg 2014;3:142-52. [PubMed]
- Hirji SA, Balderson SS, Berry MF, et al. Troubleshooting thoracoscopic anterior mediastinal surgery: lessons learned from thoracoscopic lobectomy. Ann Cardiothorac Surg 2015;4:545-9. [PubMed]
- Yan TD, Cao C, D'Amico TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg 2014;45:633-9. [Crossref] [PubMed]
- Berry MF, D'Amico TA, Onaitis MW, et al. Thoracoscopic approach to lobectomy for lung cancer does not compromise oncologic efficacy. Ann Thorac Surg 2014;98:197-202. [Crossref] [PubMed]
- Schuchert MJ, Pettiford BL, Pennathur A, et al. Anatomic segmentectomy for stage I non-small-cell lung cancer: comparison of video-assisted thoracic surgery versus open approach. J Thorac Cardiovasc Surg 2009;138:1318-25.e1. [Crossref] [PubMed]
- Zhao ZR, Situ DR, Lau RWH, et al. Comparison of Segmentectomy and Lobectomy in Stage IA Adenocarcinomas. J Thorac Oncol 2017;12:890-6. [Crossref] [PubMed]
- Zwischenberger BA, D'Amico TA, Tong BC, How I. Teach a Thoracoscopic Lobectomy. Ann Thorac Surg 2016;101:846-9. [Crossref] [PubMed]
- Demmy TL, James TA, Swanson SJ, et al. Troubleshooting video-assisted thoracic surgery lobectomy. Ann Thorac Surg 2005;79:1744-52; discussion 1753.
- Rocco G, Brunelli A, Jutley R, et al. Uniportal VATS for mediastinal nodal diagnosis and staging. Interact Cardiovasc Thorac Surg 2006;5:430-2. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [Crossref] [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. ScientificWorldJournal 2012;2012:780842. [PubMed]
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5 Suppl 3:S226-33. [PubMed]
- Yang Y, Guerrero WG, Algitmi I, et al. Complex uniportal video-assisted thoracoscopic sleeve lobectomy during live surgery broadcasting. J Thorac Dis 2016;8:1345-8. [Crossref] [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [Crossref] [PubMed]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411-5. [Crossref] [PubMed]
- Han KN, Kim HK, Choi YH. Uniportal video-assisted thoracoscopic surgical (VATS) segmentectomy with preoperative dual localization: right upper lobe wedge resection and left upper lobe upper division segmentectomy. Ann Cardiothorac Surg 2016;5:147-50. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Lei J, et al. Subxiphoid uniportal video-assisted thoracoscopic middle lobectomy and anterior anatomic segmentectomy (S3). J Thorac Dis 2016;8:540-3. [Crossref] [PubMed]
- Kara HV, Balderson SS, D'Amico TA. Modified uniportal video-assisted thoracoscopic lobectomy: Duke approach. Ann Thorac Surg 2014;98:2239-41. [Crossref] [PubMed]
- Cheng K, Zheng B, Zhang S, et al. Feasibility and learning curve of uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2016;8:S229-34. [PubMed]
- Sandri A, Filosso PL, Lausi PO, et al. VATS lobectomy program: the trainee perspective. J Thorac Dis 2016;8:S427-30. [Crossref] [PubMed]
Cite this article as: Hirji SA, Balderson SS, D’Amico TA. Uniportal lobectomy and segmentectomy—is it for all? J Vis Surg 2017;3:180.