Thoracoscopic approach to congenital diaphragmatic hernias in adults: Southampton approach and review of the literature
Introduction
Symptomatic congenital diaphragmatic hernias (CDH) are very rare in the adult population, and there has been only scanty literature about them. Surgery is indicated for the acute and the chronic presentation in the adult population. video assisted thoracoscopic surgery (VATS) is evolving in this field, and new cases are being reported every day. We present two cases of right and left symptomatic Bochdalek hernias in adults, and discuss their presentation and surgical management utilizing VATS. We aim to review the literature in this subject about hernias through abnormal congenital defects. What this account is not discussing is the transhiatal hernias through the natural orifices in the diaphragm such as sliding or rolling hiatus hernia. In addition, it is not our intention to discuss in any greater detail neonatal CDH.
Case 1 (Figure 1) (1)

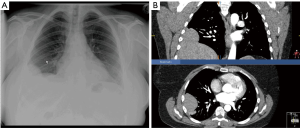
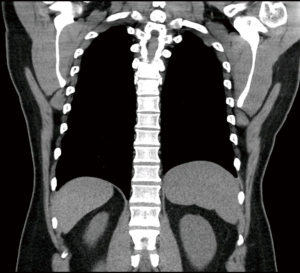
A 41 years old lady was referred to our unit with exacerbating shortness of breath on exertion, and inability to lie flat for two years. Recently she was puffed out getting into her clothes, and has given up soprano quire singing. She was getting 3–4 chest infections requiring antibiotics per year. Her past history included laparoscopy for endometriosis. Chronic obstructive pulmonary disease (COPD) was suspected, however; bronchodilators were of no avail. Her chest X-ray suggested an abnormal shadow related to her right diaphragm, and her chest and upper abdomen computed tomography (CT) scan suggested a defect in the right dome of diaphragm, with possible herniation of the liver in the chest. There were no interstitial lung changes to account for the shortness of breath (Figure 2A,B). A ‘sniff’ test under fluoroscopic screening revealed significant paradoxical movement of the right diaphragm. Nerve conduction studies of the right phrenic nerve revealed normal conduction velocities and absence of diaphragm paralysis.
Under general anesthesia and single lung ventilation she underwent VATS exploration of her right chest. Single-use optical trocars were used for port-access. These air-seal trocars have a transparent plastic sleeve, into which the thoracoscopy could be fitted before insertion, enabling the surgeon to monitor the passage of the instrument through the layers of the chest wall, avoiding injury to adherent lung. A total of 4 ports were used, two 12 mm and two 5 mm. The operating ports were carefully chosen for a posterior approach (i.e., surgeon standing posterior to the patient). The use of carbon dioxide (CO2) was crucial to push the diaphragm down and guide the repair. The intrathoracic pressure was kept below 12 mmHg. At times of hemodynamic compromise, all that was needed was to allow some of the gas to escape through one of the ports to reduce the pressure. We used a 30-degree scope, but there are other options such as the EndoCAMeleon® (Karl Storz, Tuttlingen–Germany), and Articulating-Tip ENDOEYE FLEXTM (Olympus, Shinjuku, Tokyo, Japan).
On introduction of the camera, the liver was seen herniating into the chest as predicted. A posterolateral 8 cm defect in the diaphragm was noted between the aponeurotic central tendon and the muscular costal origin, consistent with a Bochdalek hernia. The surface of the liver was bare and there was no hernia sac. Small diaphragmatic fenestrations were noted covered only by thin translucent pleura. There was no sign of endometriosis on the surface of the diaphragm. The HARMONIC® ultrasonic device (Johnson & Johnson, Ethicon, Cincinnati, USA) was used to release the adhesions between the liver and the neck of the hernia without technical difficulty. Once all the adhesions were released, the liver slipped into its natural anatomical position within the abdomen. The Endostitch™ (Medtronic-Covidien, Minneapolis, Minnesota, USA) was used to repair the defect in the diaphragm. It is used with matching special needle and Ethibond No 0 suture material. To improve anchorage into the diaphragm and safeguard against tear, 1×2 centimeter pledges of Teflon were used on either side of the stitch. This theme was also extended to plicate the diaphragm in a single suture line, using interrupted stitches radially designed from cardiophrenic angle towards the lateral chest wall, burying the hernia repair into the peritoneal space like a ship’s keel.
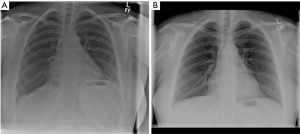
At the end of the procedure a 24-F intercostal drain was introduced and the lung was allowed to inflate. An extrapleural catheter was fitted for continuous postoperative titration of Bupivacaine analgesia. Postoperatively the patient was electively admitted to the intensive care unit (ITU) as planned. She was extubated 8 hours later and was transferred to the general ward the following morning. She was allowed home in two days, with a satisfactory chest X-ray (Figure 3A). She was then seen in a follow up clinic six months later, and was noted to have significant subjective improvement of her breathing. Her chest X-ray documented sustainability of a low and flat right diaphragm (Figure 3B).
Case 2 (Figure 4) (2)

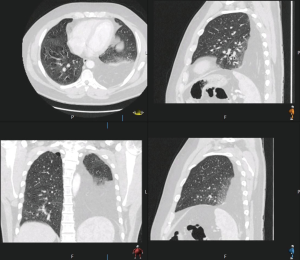
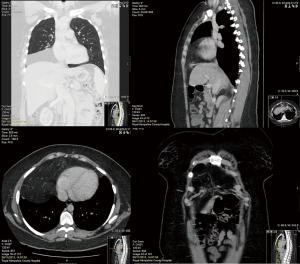
A 46 years old male was referred to our unit suffering from worsening shortness of breath. Previously he was very fit, cycling 8 miles daily. He reached a stage where he could not finish a sentence without being short of breath. Acute admission to hospital was followed by a chest X-ray, which revealed left sided lung consolidation. A CT scan suggested a posterolateral deficiency in the left diaphragm consistent with a left Bochdalek hernia, and possible herniation of the greater omentum into the left chest (Figure 5). His FEV1 =3.73 L (101.9% predicted) and transfer factor TLCO =9.94 mmol/min/kPa (96.8% predicted). He had a –8% drop in Vital Capacity from sitting to supine position.
He underwent VATS exploration of his left chest using the same technique as the first case. Again four ports and CO2 were used, keeping pressures <12 mmHg. Almost all of the greater omentum was found in the chest, herniating through a posterolateral single defect in the diaphragm, consistent with a Bochdalek hernia. Due to adhesions with the hernia ring beyond the vision of the thoracic approach, it was not possible to reduce the omentum back to the abdomen. The omentum was therefore transected close to the neck of the hernia using a stapling device (Tri StapleTM, Endo GIATM, Medtronic-Covidien, Minneapolis, Minnesota, USA). This was performed after thorough checking that there was no herniating small bowel hiding within the omentum. The hernia defect could have been repaired ideally by a synthetic patch, but at the time we had no experience with such patch repair. Therefore; the defect was closed end to end using the Endostitch™ device (Medtronic-Covidien, Minneapolis, Minnesota, USA).
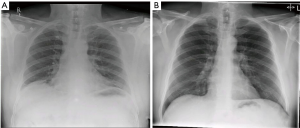
His recovery was uncomplicated and was discharged on the second postoperative day. On six months follow up he had noticed significant subjective improvement and was asymptomatic (Figure 6A,B). His diaphragm on that occasion remained low with clear lung fields. His shortness of breath recurred after one year and a fresh CT was ordered. The left hemidiaphragm was found to be slightly higher than the right, but without evidence of recurrence of the hernia (Figure 7). There were minor emphysematous changes but nothing to account for his shortness of breath.
Discussion
CDH and structural anomalies of the diaphragm have been described, studied, and treated for over 400 years (3). In 30% of CDH patients, genomic analyses have identified a range of genetic defects, including chromosomal anomalies, copy number variants and sequence variants. It is thought to be part of a multisystem genetic syndrome, as CDH-associated genetic mutations affect not only development of the diaphragm but also directly affect the development of other organs, such as the heart and lungs (4). Anatomy of the human diaphragm at birth and the possible types of diaphragmatic defects were elegantly schematically shown by Kardon et al. (2017) (5).
Bochdalek hernia
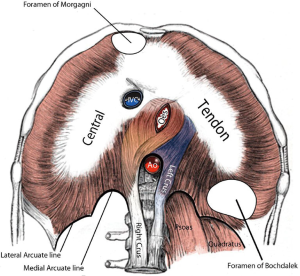
In 1848, Vincent Alexander Bochdalek first described a congenital hernia resulting from the developmental failure of the diaphragmatic posterolateral foramina to fuse properly (5-8). Bochdalek hernia is one of the most common abnormalities presented in infants with a reported incidence of about 1 in 3,000 live births, and represents about 80% of CDH (9). They are associated with significant morbidity and mortality due to associated pulmonary hypoplasia, pulmonary hypertension and heart failure. The majority are diagnosed antenatal or in the neonatal period. During embryonic development a septum known as the septum transverse develops between pleural and peritoneal cavities, but does not completely separate the two, leaving large defects known as the pleuroperitoneal canals on either side. Around the 8th week of gestation, the pleuroperitoneal membrane forms over the canals and closes the connection between the chest and abdomen (Figure 8). As the right pleuroperitoneal canal closes earlier than the left, a Bochdalek hernia predominantly occurs on the left chest (80% of cases) (5). A hernia sac has been reported to be present in 10 to 38% of cases (10). There was no hernia sac in our two cases and this is consistent with other reports in the literature (11-13).
The survival rate for infants born with Bochdalek hernias varies from institution to institution; but overall, it has remained at about 50% for nearly half a century, despite advances in neonatal intensive care, anaesthesia, and surgery (8). Bodwitch is credited for the most extensive paper on the subject of paediatric Bochdalek hernias giving a numerical analysis of all the cases recorded in the medical literature between the years 1610–1846 (14). Of the 118 cases of CDH collected by Livingston, 83 were on the left side, 18 on the right, 4 were central, 2 were double, and in one case the diaphragm was absent (15).
New therapies are emerging for prenatal diagnosis of Bochdalek hernia. Fetal endoscopic tracheal occlusion (FETO) and prenatal transplacental fetal treatments, aim to normalize lung development and pulmonary vascular tone to prevent and treat lung hypoplasia and pulmonary hypertension (9,16). FETO takes advantage of fluid production within the fetal lung to induce stretch and growth by preventing lung fluid from escaping the airway. The current approach includes insertion of a balloon to occlude the trachea at 26–28 weeks of gestation, followed by removal of the balloon at 34 weeks (16).
Symptomatic Adult congenital Bochdalek hernia on the other hand, is extremely rare with a prevalence of 0.17–6% of all diaphragmatic hernias. There are fewer than 100 cases of Bochdalek hernia reported in adults in the literature and fewer than 20 of those cases involve right-sided hernias (6). In the United Kingdom, a general consultant thoracic surgeon is likely to encounter only a single case in a whole career. Paralysed diaphragm could be incriminated as in our first case. Tension pneumothorax has been suspected on the chest X-ray (17). Recurrent abdominal pain, postprandial fullness and vomiting are the most common abdominal symptoms in adults (18). Herniating colon, small intestines, liver, kidney, gall bladder, spleen, pancreas, stomach, appendix and omentum have all have been previously reported. Acute presentation can be life threatening, especially with threatened bowel in the chest (6,10,18). The respiratory symptoms are related to the ‘space occupying lesion’ in the chest, namely, shortness of breath on exertion.
In females the mechanism of herniation becomes complex. Whereas Bochdalek hernia is a single congenital defect, clinically it is not very different from multiple large defects thought to be diaphragmatic fenestrations (18). How these multiple fenestrations come to existence is a subject of debate. Whether these are congenital or acquired is unknown. Fenestrations are thought to represent sloughing of endometriosis foci, however; endometrial deposits have only been found in 60% of cases. The relationship between diaphragm fenestrations and catamanial pneumothorax is well established, and the presence of a liver hernia through these fenestration have been described before by Sanna et al. 2011 (19). The increased intra-abdominal pressure during pregnancy is thought to be a major cause of herniation through these defects in females. Usually fenestrations are multiple, whereas Bochdalek hernia is a single defect in a specific location. Our first case, the lady had a history of endometriosis for which had laparoscopic examination. At operation there was evidence of tiny fenestrations not entirely communicating the peritoneal to the pleural space. Whether the diaphragmatic defect is originally a fenestration that has been dilated by a herniating liver, helped by multiple pregnancies is unknown.
Repair of a symptomatic Bochdalek hernia is recommended in the adult population. Despite the assumption that this is a congenital abnormality that has existed for a long number of years, and the advocacy of leaving well alone, yet potentially life-threatening bowel obstruction can ensue (4,20). It is preferable to deal with the problem electively when the patient is fit, rather than acutely under life-threatening conditions such as bowel incarceration. Haemothorax and intra-abdominal hemorrhage complicating normal pregnancy have been separately reported as a complication of Bochdalek hernia (21,22).
Generally speaking, the diaphragm is a disputed turf between thoracic and upper gastro-intestinal surgeons, both specialties claiming superiority of their approach. For thoracic surgeons it remained ‘the nuclear option’ for a long time, no one dared to push the button. Walker as early as 1900 realized that “on account of the difficulty of reducing the gut, ligating the sac, and stitching the rent in the diaphragm, the transpleural route is preferable” (23). The hernia can be treated via thoracotomy assisted with laparoscopy with good effect (11). In urgent cases with possible threatened bowel, the access of choice is a low thoracotomy (7th intercostal space). Such access allows extension into the abdomen if needed, by radial or circumferential phrenotomy. Alternatively, the skin incision could be extended into a thoraco-abdominal incision and the costal margin is cut. Our two cases discussed here presented with non life-threatening conditions, giving time to think about minimal access surgery (VATS). Very few reports are found in the literature about symptomatic adults with Bochdalek hernia, however; a similar case to our second case was published by Frantzides in 2013 (24). He managed to close the defect primarily without a patch, and the area near the chest wall did not seem to pose a challenge. Daniel Gwan-Nulla demonstrated how to repair a recurrent Bochdalek hernia by VATS using a patch (25).
Morgagni hernia (also called hernia of Morgagni-Larrey)
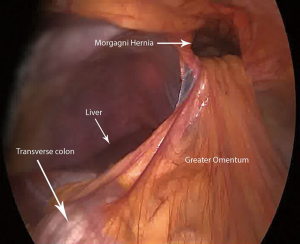
In 1769, Morgagni described the substernal herniation of the abdominal viscera into the chest cavity on autopsy examinations (26). In 1828, Larrey described a surgical approach to the pericardial cavity through an anterior diaphragmatic defect (27). The hernia space described by both Morgagni and Larrey is a triangular space between the muscle fibers of the diaphragm originating from the xiphoid process and the nearby costal margin on either side, and inserted on the central tendon of the diaphragm (Figure 8). These hernias are not usually discovered in newborns, and are not usually associated with pulmonary hypoplasia. They are usually asymptomatic, making their debut due to incarcerated or threatened bowel in the chest. They represent 3% of all CDH (28). Herniation to the right chest is by far commoner than the left (90%) and the most common contents of the hernia are the omentum, followed by the colon, small intestine, and stomach. Almost always a hernia sac exists (92%). The CT is usually diagnostic (29). Figure 9 shows a CT of 43 years old lady referred to our unit with chronic right lower chest pain and shortness of breath on exertion for two years. She was thought to have chronic lower lobe consolidation, but her CT scan confirmed the presence of a Morgagni hernia (Figure 10). She underwent successful laparoscopic repair of her Morgagni hernia by the upper gastro-intestinal surgeons in our institution, and a synthetic patch was used. Only the greater omentum was herniating at operation. This was a seminal case in which we picked up the technique of patch repair, which we soon implemented to patch a defect in the pericardium (30). Inter-disciplinary exchange of experience is vital for pushing the envelope and blazing the trail of VATS. Figure 4 shows how we were pontificating repair of a Bochdalek hernia by laying down a synthetic patch. Not long after our case, Daniel Gwan-Nulla elegantly demonstrated how to repair a recurrent Bochdalek hernia using a patch (25). We could have benefited from his experience if it was published before ours. Certainly development of the social media, including blogs, social networks, video and photo-sharing sites on the Internet made exchange of surgical experience and acquisition of new techniques swift and effective (31). The number of visual periodicals and websites that primarily give free access to video material has exponentially increased in the last 5 years. The paper-printed material and the orthodox operative atlases are finding it difficult to pull their weight against the video-format material. No doubt we will witness further expansion in video-publishing of surgical information in the near future. It has the advantage of reaching far more viewer than subscription paper-printed format journals, and relevance is immediately judged by the number of hits, shares and blogs.
Thoracic surgeons do not deal with Morgagni hernias, or at least not for the moment. The current state of affairs is that it is the domain of the upper GI surgeons, who claim it is easier dealt with from the peritoneal cavity (32). A patch is usually needed to cover the defect. Thoracic surgeons are not familiar with views of the subxiphoid area from a chest perspective. This is highlighted in a case published by Komatsu describing VATS missing the Morgagni hernia as a lipoma, and the patient re-presented with bowel incarceration requiring laparotomy (33). In acute presentations with threatened bowel in the chest, surgical access is controversial. Abdominal access (by laparotomy) allows the entire contents of the abdomen to be examined, bowel anastomosed, and a colostomy fashioned should the need arise (34). On the other hand, thoracotomy allows better adhesiolysis of a chronic bowel herniation, at the risk of poor exposure of the hernia ring. Nakashima et al presented their experience with VATS repair of Morgagni hernia, and they advocate it as first choice over laparoscopic approach in the management of adult patients with Bochdalek or Morgagni hernias and severe adhesion (35). As thoracic robotic experience evolves we will see in the not too distant future thoracic surgeons venturing in this area of patch repair of CDH. After all what’s in the chest is best dealt with by chest surgeons, “Render to Caesar the things that are Caesar’s”.
Conclusions
Symptomatic Bochdalek hernia, and possibly Morgagni hernia in the adult population could be safely repaired by VATS with good and lasting results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Amer K. VATS repair of right Bockdalek hernia and diaphragmatic plication. Asvide 2017;4:522. Available online: http://www.asvide.com/articles/1841
- Amer K. VATS repair of left Bochdalek hernia. Asvide 2017;4:523. Available online: http://www.asvide.com/articles/1842
- Irish MS, Holm BA, Glick PL. Congenital diaphragmatic hernia. A historical review. Clin Perinatol 1996;23:625-53. [PubMed]
- He S, Sade I, Lombardo G, Prabhakaran K. Acute presentation of congenital diaphragmatic hernia requiring damage control laparotomy in an adult patient. J Surg Case Rep 2017.rjx144. [PubMed]
- Kardon G, Ackerman KG, McCulley DJ, et al. Congenital diaphragmatic hernias: from genes to mechanisms to therapies. Dis Model Mech 2017;10:955-970. [Crossref] [PubMed]
- Rout S, Foo FJ, Hayden JD, et al. Right-sided Bochdalek hernia obstructing in an adult: case report and review of the literature. Hernia 2007;11:359-62. [Crossref] [PubMed]
- Korom S, Canyurt H, Missbach A, et al. Catamenial pneumothorax revisited: clinical approach and systemic review of the literature. J Thorac Cardiovasc Surg 2004;128:502-8. [Crossref] [PubMed]
- Golombek SG. The history of congenital diaphragmatic hernia from 1850s to the present. J Perinatol 2002;22:242-6. [Crossref] [PubMed]
- Stege G, Fenton A, Jaffray B. Nihilism in the 1990s: the true mortality of congenital diaphragmatic hernia. Pediatrics 2003;112:532-5. [Crossref] [PubMed]
- Kocakusak A, Arikan S, Senturk O, et al. Bochdalek's hernia in an adult with colon necrosis. Hernia 2005;9:284-7. [Crossref] [PubMed]
- Laaksonen E, Silvasti S, Hakala T. Right-sided Bochdalek hernia in an adult: a case report. J Med Case Rep 2009;3:9291. [Crossref] [PubMed]
- Shen YG, Jiao NN, Xiong W, et al. Video-assisted thoracoscopic surgery for adult Bochdalek hernia: a case report. J Cardiothorac Surg 2016;11:165. [Crossref] [PubMed]
- Yamaguchi M, Kuwano H, Hashizume M, et al. Thoracoscopic treatment of Bochdalek hernia in the adult: report of a case. Ann Thorac Cardiovasc Surg 2002;8:106-8. [PubMed]
- Bodwitch HI. A treatise on diaphragmatic hernia. Buffalo Med J 1853;9:65-95.
- Livingston. Diseases of the newly born. 2nd ed. In: Emmett Holt L, editor. The Diseases of Infancy and Childhood. D. Appleton and Company: New York, 1903:116.
- Hedrick MH, Estes JM, Sullivan KM, et al. Plug the lung until it grows (PLUG): a new method to treat congenital diaphragmatic hernia in utero. J Pediatr Surg 1994;29:612-7. [Crossref] [PubMed]
- Dalton AM, Hodgson RS, Crossley C. Bochdalek hernia masquerading as a tension pneumothorax. Emerg Med J 2004;21:393-4. [Crossref] [PubMed]
- Kanazawa A, Yoshioka Y, Inoi O, et al. Acute respiratory failure caused by an incarcerated right-sided adult Bochdalek hernia: report of a case. Surg Today 2002;32:812-5. [Crossref] [PubMed]
- Sanna S, Taurchini M, Monteverde M. Catamenially recurring pneumothorax with partial liver herniation: a particular view. Respiration 2011;82:476-7. [Crossref] [PubMed]
- Ekanayake E, Fernando SA, Durairajah PL, et al. Incarcerated Bochdalek hernia causing bowel obstruction in an adult male patient. Ann R Coll Surg Engl 2017;99:e159-61. [Crossref] [PubMed]
- Koca YS, Barut I, Yildiz İ, et al. The Cause of Unexpected Acute Abdomen and Intra-Abdominal Hemorrhage in 24-Week Pregnant Woman: Bochdalek Hernia. Case Rep Surg 2016;2016:6591714. [Crossref] [PubMed]
- Niwa T, Nakamura A, Kato T, et al. An adult case of Bochdalek hernia complicated with hemothorax. Respiration 2003;70:644-6. [Crossref] [PubMed]
- Walker EW. Diaphragmatic hernia. JAMA 1900;35:778.
- Thoracoscopic Congenital Left Diaphragmatic Hernia Repair (CDH). In: Frantzides CT, Carlson MA, editors. Video Atlas of Advanced Minimally Invasive Surgery. Philadelphia: Elsevier, 2013.
- Gwan-Nulla D. VATS Repair of Recurrent Congenital Bochdalek Hernia With Intrathoracic Herniation of the Kidney and Portion of the Pancreas. Available online: https://www.ctsnet.org/article/vats-repair-recurrent-congenital-bochdalek-hernia-intrathoracic-herniation-kidney-and. Last accessed 19th November 2017.
- Morgagni G. Seats and causes of diseases. In: Cadell T, Millar A, editors. London: 1769.
- Larrey D. De plaies du pericarde et du coeur clinique chirugicale. In: Gubon P, editor. Paris: 1828:284.
- Minneci PC, Deans KJ, Kimb P, et al. Foramen of Morgagni hernia: changes in diagnosis and treatment. Ann Thorac Surg 2004;77:1956-9. [Crossref] [PubMed]
- Gossios KJ, Tatsis CK, Lykouri A, et al. Omental herniation through the foramen of Morgagni. Diagnosis with chest computed tomography. Chest 1991;100:1469-70. [Crossref] [PubMed]
- Amer K. VATS Pericardial patch: minimally invasive stitching. CTSNet, Inc. Available online: https://doi.org/ [Crossref]
- Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T 2014;39:491-520. [PubMed]
- Gonzalez HA, Kwazneski DR, Awais O, et al. Minimally-invasive Morgagni hernia repair. Available online: https://youtu.be/cIlD36YOHoE
- Komatsu T, Takahashi Y. Is this a mediastinal tumor? A case of Morgagni hernia complicated with intestinal incarceration mistaken for the mediastinal lipoma previously. Int J Surg Case Rep 2013;4:302-4. [Crossref] [PubMed]
- Kesieme EB, Kesieme CN. Congenital diaphragmatic hernia: review of current concept in surgical management. ISRN Surgery 2011;2011:974041. [Crossref] [PubMed]
- Nakashima S, Watanabe A, Hashimoto M, et al. Advantages of video-assisted thoracoscopic surgery for adult congenital hernia with severe adhesion: report of two cases. Ann Thorac Cardiovasc Surg 2011;17:185-9. [Crossref] [PubMed]
Cite this article as: Amer K. Thoracoscopic approach to congenital diaphragmatic hernias in adults: Southampton approach and review of the literature. J Vis Surg 2017;3:176.


