Congenital bronchial atresia in adults: thoracoscopic resection
Introduction
Bronchial atresia is a congenital malformation arising during the formation of bronchi. It consists in a partial defect of a bronchus—usually at a segmental level—leading to the distension of the corresponding pulmonary parenchyma. They belong to the group of congenital pulmonary airway malformations (CPAM), which is different from the group of bronchopulmonary sequestrations (BPS) (1). Both malformations can be associated. CPAM are most often diagnosed in the neonatal period or in the young child (2), and sometimes in the adult, as in the case of the patients of this series. Pneumothorax (3), infection (4) and, in the long term, degradation of the pulmonary parenchyma are the main complications (1). Surgery is indicated, especially now that—in most patients—it can be safely performed without opening the chest (5).
Patients and methods
Between 2007 and 2017, eight patients were operated on for a congenital bronchial atresia (CBA) in our department. All patients had a chest computed tomographic (CT) scan with intravenous contrast and, more recently a 3-dimensional modelisation based on CT. Intraoperative and postoperative data (including demographic criteria, clinical symptoms, surgical procedure, and final histology) were recorded from this database which was approved from our Institutional Review Board (CEPAR 2013-002).
All eight patients were operated on by a full thoracoscopic approach with a fissure-based dissection of vascular elements. The technique has already been reported (6) and will not be described here.
Results
Among the eight patients, there were five males and three females with a median age of 29.5 years (range, 14 to 48 years). All patients were symptomatic with recurrent pneumoniae but one, in which CBA was incidentally discovered.
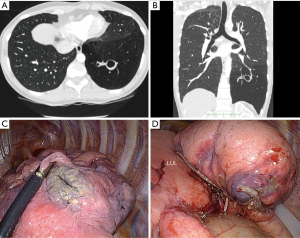
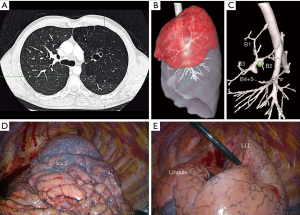
CT scan was in favor of CBA in all cases usually showing a cystic lesion within a distended parenchyma (Figure 1). 3D modelisation, based on injected CT, can clearly demonstrate the bronchial interruption and the pathological hyperinflated parenchyma (Figure 2). Five out of the pulmonary resections were a lobectomy and 3 an anatomic segmentectomy. No intraoperative complication occurred. Mean operation time was 204 min (range, 127–315 min), and mean blood loss was 89 mL (range, 0–200 mL). Five patients (62.5%) had minor postoperative complications: air leak (n=4) and pneumothorax (n=1) after chest tube removal, requiring drainage. Mean drainage duration was 5.5 days (range, 3–11 days). Mean hospital stay was 7.1 days (range, 4–14 days).
The diagnosis of CBA was confirmed on final pathological examination.
Discussion
Bronchial atresia is a rare congenital malformation related to a defect in vascularization during the development of the bronchial bud, resulting in a cul-de-sac termination of one or more bronchi. The adjacent pulmonary parenchyma develops normally and secretes mucus, which accumulates and forms mucoid impactions and/or bronchocele (1,2). Collateral ventilated alveoli (Kohn’s pores) provoke air retention and distension of the lung downstream of the atresia, which can cause recurrent infections and even mycobacterium infection (4) and, in the long term, destruction of the corresponding parenchyma. Pneumothorax can also reveal the malformation (3). Atresia is more common in segmental bronchi than in lobar ones. It can affect several territories (1,2). Although this abnormality is more often segmental than lobar (7), lobectomy is the most frequently reported resection since the remaining parenchyma is usually compressed by the abnormal segment, which is hyperinflated by trapping and by mucus accumulation (7,8). In a series of 29 bronchial atresias in children reported by Morikawa et al., a segmentectomy was performed in only three cases (9). Other congenital malformations may be associated with bronchial atresia such as pectus excavatum (10). At histology, CBA is defined by an obstructed bronchus, which does not communicate with the rest of the bronchial tree, associated with bronchocele and surrounded by an over-inflated pulmonary parenchyma. Sometimes communication with the bronchial tree is preserved, but its light is occluded. Also, normal bronchoscopy does not eliminate the diagnosis of atresia. Thoracic CT demonstrates malformation by typically showing a cystic lesion within a distended parenchyma zone. 3D modelisation provides an additional help to the surgeon.
Bronchial atresia is most often diagnosed in the neonatal period or in childhood, with a radiological abnormality or repeated lung infections in the same territory, explaining why the largest series reported are pediatric (1,9). It is rarely discovered in adults, especially after 40 years (11). All our patients were operated by a full thoracoscopic approach (9). These patients are indeed young, with no comorbidity and with a good quality parenchyma. The limit between the healthy and pathological parenchyma facilitates thoracoscopic segmentectomy (12,13). In two patients of our series, the segment adjacent to the malformation was too pathological and a lobectomy seemed justified. In one of our patients with an atresia involving two different lobes, we limited the extent of the resection to a lobectomy by leaving in place a pathological segment in order to prevent a re-expansion issue.
Conclusions
- Surgical treatment of CBA seems justified, even in asymptomatic cases, to prevent recurrent infectious pulmonary complications and long-term lung alteration.
- Parenchyma-sparing treatment should be discussed whenever possible.
- A thoracoscopic approach should be used whenever possible.
Acknowledgements
None.
Footnote
Conflicts of Interest: D Gossot is consultant for an instrument manufacturer (Delacroix Chevalier). The other authors have no conflicts of interest to declare.
References
- Hardee S, Tuzovic L, Silva CT, et al. Congenital Cystic Lung Lesions: Evolution From In-utero Detection to Pathology Diagnosis-A Multidisciplinary Approach. Pediatr Dev Pathol 2017;20:403-10. [Crossref] [PubMed]
- Asada M, Yano S, Okayasu K, et al. A case report of congenital bronchial atresia--a review of 43 cases in Japan. Nihon Kyobu Geka Gakkai Zasshi 1991;39:463-8. [PubMed]
- Igai H, Kamiyoshihara M, Nagashima T, et al. Anatomical segmentectomy for pneumothorax associated with congenital bronchial atresia. Eur J Cardiothorac Surg 2013;43:198. [Crossref] [PubMed]
- Matsuoka K, Ueda M, Miyamoto Y. Mycobacterium avium infection complicating congenital bronchial atresia. Asian Cardiovasc Thorac Ann 2016;24:808-10. [Crossref] [PubMed]
- Cappeliez S, Lenoir S, Validire P, et al. Totally endoscopic lobectomy and segmentectomy for congenital bronchial atresia. Eur J Cardiothorac Surg 2009;36:222-4. [Crossref] [PubMed]
- Gossot D. Atlas of endoscopic major pulmonary resections. 2nd edition. Berlin: Springer-Verlag, 2017.
- Antón-Pacheco J, Galletti L, Cabezalí D, et al. Management of bilateral congenital bronchial stenosis in an infant. J Pediatr Surg 2007;42:E1-3. [Crossref] [PubMed]
- Seo T, Ando H, Kaneko K, et al. Two cases of prenatally diagnosed congenital lobar emphysema caused by lobar bronchial atresia. J Pediatr Surg 2006;41:e17-20. [Crossref] [PubMed]
- Morikawa N, Kuroda T, Honna T, et al. Congenital bronchial atresia in infants and children. J Pediatr Surg 2005;40:1822-6. [Crossref] [PubMed]
- van Klaveren RJ, Morshuis WJ, Lacquet LK, et al. Congenital bronchial atresia with regional emphysema associated with pectus excavatum. Thorax 1992;47:1082-3. [Crossref] [PubMed]
- Mordant P, De Dominicis F, Berna P, et al. Tracheobronchial and pulmonary parenchymatous congenital abnormalities requiring surgical treatment in adults. Rev Pneumol Clin 2012;68:110-6. [Crossref] [PubMed]
- Tsuchida M, Aoki K, Hashimoto T, et al. Segmental bronchial atresia of the left upper lobe treated with segmental resection under video-assisted thoracic surgery. Surg Laparosc Endosc Percutan Tech 2001;11:217-20. [Crossref] [PubMed]
- Macias L, Ojanguren A, Dahdah J, et al. Thoracoscopic anatomical resection of congenital lung malformations in adults. J Thorac Dis 2015;7:486-9. [PubMed]
Cite this article as: Traibi A, Seguin-Givelet A, Grigoroiu M, Brian E, Gossot D. Congenital bronchial atresia in adults: thoracoscopic resection. J Vis Surg 2017;3:174.


