Subxiphoid single incision thoracoscopic surgery approach for thymectomy: a case report
Introduction
Although rare, thymoma constitutes the most common malignancy of the anterior mediastinum (1). Surgical thymectomy with complete resection of thymoma remains the gold standard in the management of these patients, which has good long term survival and recurrence rates when complete en-bloc resection is achieved (1,2).
Traditionally, thymectomy is approached through a median sternotomy which provides full exposure and access to surrounding mediastinal structures and pericardial fat which may potentially be involved with the tumour. However, over recent years development of video-assisted thoracoscopic surgery (VATS) has provided an attractive alternative minimally invasive operative strategy. Now median sternotomy is reserved for patients in whom complete resection is not thought possible via the VATS approach or due to intra-operative complications. VATS surgery has evolved over time from multiport to uniportal access with the aim of reducing the pain associated with multiple trans-thoracic incisions. Uniportal VATS has become widely adopted as the approach of choice for managing a variety of thoracic diseases including thymectomy (3).
More recently, to further minimise the surgical impact, the uniportal subxiphoid VATS (SVATS) technique has been described. This approach may offer several advantages when performing a thymectomy, including: the ability to access both sides of the chest with a single incision, reduced post-operative pain and chronic thoracostomy neuralgia due to being a muscle sparing incision and to avoiding damage to the intercostal nerves (4).
This case report describes our procedure and technique for performing uniportal subxiphoid VATS thymectomy.
Case presentation
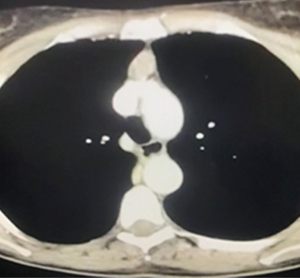
A 51-year-old female myasthenic patient was referred for surgical management of a 2.5 cm anterior mediastinal mass likely to be a thymoma. The computed tomography (CT) scan did not reveal any obvious invasion of surrounding mediastinal structures (Figure 1). The decision was made to proceed with an extended thymectomy. She was otherwise fit and well with no co-morbidities. She had bilateral breast implants.
Surgical procedure
A single staged bilateral surgical intervention was planned. With the patient under general anesthesia and double lumen endotracheal tube intubation we positioned the patient supine with both arms adducted. Inflatable air bags were positioned under the right and left hemithorax. These were later inflated, to tilt the patient and achieve better visualisation of the medial mediastinum as required.
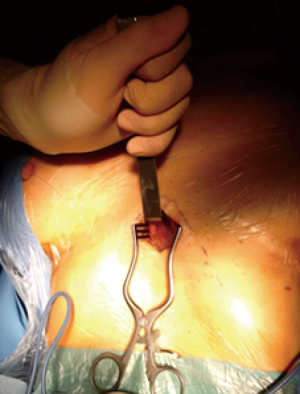
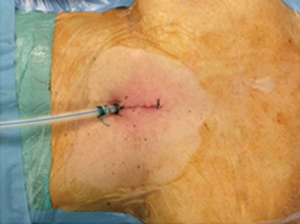
A 3 cm midline vertical incision was made below the sternocostal triangle to expose the xiphoid process. Dissection of the linea alba was performed and the pleural cavity was entered by blunt finger dissection above the level of the diaphragm (Figure 2). A SILS port (Covidien, Mansfield, MA, USA) was then inserted (Figure 3A), and CO2 insufflated at a maximal pressure of 8 mmHg. CO2 insufflation within the mediastinum generates a very useful amount of extra working space within the anterior-superior mediastinum allowing for easier dissection and better visualization of the mediastinal structures especially toward the cranial part of the mediastinum cephalad to the left innominate vein including the upper poles of the thymus.

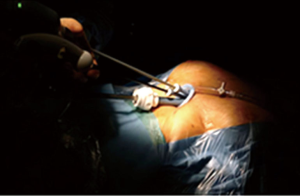
Under visual guidance provided through a 10-mm EndoCAMeleon® Telescope (Karl Storz, Tuttlingen, Germany) the operator utilized grasping forceps designed for single-incision surgery (SILS Hand Instruments Endo Clinch™ II, Covidien, Mansfield, MA, USA—Figure 3B) and performed dissection, coagulation, and division of tissue mainly using the Sonicision™ cordless ultrasonic dissection device (Covidien, Mansfield, MA, USA) and occasionally using a normal straight hook cautery (Figure 4).
The phrenic nerves and mammary arteries and veins bilaterally were visualized throughout the procedure minimizing the risk of injury as was the cranial part of the mediastinum, permitting a safe dissection en-bloc of the thymus, thymic mass, and surrounding fatty tissue anterior to the phrenic nerves. The specimen was removed using an endoscopic retrieval bag (EndoBag, Covidien, Mansfield, MA, USA).
One 28 Fr drain was placed via the subxiphoid incision (Figure 5) and placed on −2 KPa suction using a Thopaz system (Medela, Switzerland).
Post-operative management
The patient was mobilized and received intensive physiotherapy from day 0 with minimal pain. The drain was removed on the first post-operative day and the patient was discharged home on the second post-operative day. Adequate post-operative analgesia was achieved with paracetamol alone. Final histology confirmed a Masaoka stage I thymoma with an R0 resection.
Discussion
Although surgical resection through a median sternotomy remains the gold-standard approach for thymectomy it is associated with significant morbidity. Division of the sternum requires a large incision and is associated with greater pain, length of hospital stay and slower return to pre-morbid function when compared to VATS thymectomy. VATS thymectomy has been demonstrated to have several advantages including reduced intraoperative blood loss, earlier removal of chest drains, reduced requirement for blood products, reduced inflammatory cytokine response, shorter hospital stay and superior cosmesis (5). VATS thymectomy can be performed through left, right or bilateral approaches, which is dependent on pre-operative planning, intra-operative findings but often surgeon preference. There are several studies which suggest the superiority of a VATS approach to thymectomy compared to median sternotomy without compromising the oncological outcome (6).
As the minimally invasive era has evolved, the recent development of uniportal thoracoscopic access has become increasingly popular. This approach was first described by Rocco et al. for minor thoracic and pulmonary procedures and is now used for a variety of major thoracic procedures including pulmonary lobectomies (3).
A further development has been the use of the subxiphoid VATS approach which has been described for a number of cardiothoracic procedures including subxiphoid pericardial window creation, coronary artery surgery, ablative sympathectomy, pulmonary wedge resection and even lobectomy (7-10). The potential benefits of the subxiphoid VATS approach includes reduced postoperative pain and the absence of chest wall paraesthesia due to preservation of the intercostal innervation and the absence of chest drains impinging on the intercostal neurovascular bundles.
Uniportal subxiphoid VATS access provides excellent views of the anterior mediastinum as well as of the two pleural spaces including the phrenic nerves making it an ideal alternative approach to performing a thymectomy. This access and view provides the surgeon the opportunity to perform an oncologically radical and safe resection of the thymus and peri-thymic fatty tissues with low risk of incurring phrenic nerve injury.
The subxiphoid VATS technique can be learnt by surgeons experienced in uniportal VATS. The camera views and instrument positioning can be more challenging than for conventional VATS but the necessary skills can be acquired over a short learning curve, particularly for minor procedures. The approach has been demonstrated to be safe with good short-term outcomes and superior cosmetic results (7-11).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Tomaszek S, Wigle DA, Keshavjee S, et al. Thymomas: review of current clinical practice. Ann Thorac Surg 2009;87:1973-80. [Crossref] [PubMed]
- Regnard JF, Magdeleinat P, Dromer C, et al. Prognostic factors and long-term results after thymoma resection: a series of 307 patients. J Thorac Cardiovasc Surg 1996;112:376-84. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Yano M, Moriyama S, Haneda H, et al. The Subxiphoid Approach Leads to Less Invasive Thoracoscopic Thymectomy Than the Lateral Approach. World J Surg 2017;41:763-70. [Crossref] [PubMed]
- Reddy RV. The advantages of VATS: a systematic review. Thorax 2005;60:238. [Crossref]
- Raza A, Woo E. Video-assisted thoracoscopic surgery versus sternotomy in thymectomy for thymoma and myasthenia gravis. Ann Cardiothorac Surg 2016;5:33-7. [PubMed]
- Aresu G, Jiang L, Bertolaccini L. Subxiphoid video-assisted major lung resections: the Believers' speech. J Thorac Dis 2017;9:E387-E389. [Crossref] [PubMed]
- Hernandez-Arenas LA, Lin L, Yang Y, et al. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur J Cardiothorac Surg 2016;50:1060-6. [Crossref] [PubMed]
- Hernandez-Arenas LA, Guido W, Jiang L. Learning curve and subxiphoid lung resections most common technical issues. J Vis Surg 2016;2:117. [Crossref]
- Aresu G, Wu L, Lin L, et al. The Shanghai Pulmonary Hospital subxiphoid approach for lobectomies. J Vis Surg 2016;2:135. [Crossref]
- Aresu G, Weaver H, Wu L, et al. The Shanghai Pulmonary Hospital uniportal subxiphoid approach for lung segmentectomies. J Vis Surg 2016;2:172. [Crossref]
Cite this article as: Karunanantham J, Fok M, Ali JM, Peryt A, Coonar A, Aresu G. Subxiphoid single incision thoracoscopic surgery approach for thymectomy: a case report. J Vis Surg 2017;3:147.