Needlescopic-assisted uniportal video-assisted thoracoscopic pulmonary anatomical segmentectomy
Introduction
Sublobar resection has been shown to be an effective alternative approach in the treatment of lung cancer (1-3). Although segmentectomy and wedge resection are grouped as sublobar resections, segmentectomy is more technically challenging than wedge resection, and current evidence suggests that wedge resection is associated with higher local recurrence compared with anatomical segmentectomy (4,5). Furthermore, several recent meta-analyses have shown that segmentectomy can be an oncologic equivalent of lobectomy (6,7). The development of uniportal video-assisted thoracoscopic surgery (VATS) in recent years has greatly changed the preference of thoracic surgeons in major pulmonary resections to segmentectomies. The potential advantages are less pain, better cosmesis, and direct surgical view for the operator (8,9). However, thoracoscopic anatomical segmentectomy is a complex and time-consuming procedure, and it was generally performed through three or more thoracic incisions, even though some of the experts had reported their experiences (10,11). Needlescopic instruments that are 3 mm in diameter or less are commonly utilized as adjuncts to traditional laparoscopy or single-port laparoscopic surgery and result in almost invisible surgical wounds (12). Needlescopic VATS was developed before uniportal VATS; however, its applications are confined to minor procedures such as sympathectomy for palmar hyperhidrosis and simple lung wedge resections (13-15). Here, we report our experience with thoracoscopic anatomical segmentectomy using the technique of uniportal VATS with the assistance of the additional needlescopic instruments.
Operating room set-up and surgical instruments
The standard set-up of the operating room consisted of two monitors, positioned at the front and back of the patient. The uniportal surgeon is positioned on the ventral side of the patient with the cameraman and the needlescopic surgeon on the dorsal side (Figure 1).
A 10-mm, 30° angled HD video-thoracoscope was used in all cases. Regular uniportal VATS instruments and needlescopic instruments were used (Figure 2).
Operative technique
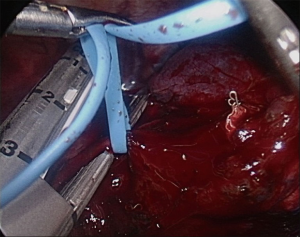
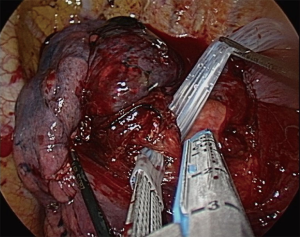
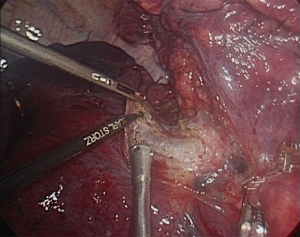
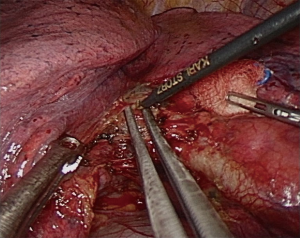
The size and the location of the utility incision are identical to those of regular uniportal VATS. After the uniportal system had been set up, two additional needlescopic ports were made under thoracoscopic guidance. The levels of needlescopic ports should be lower than the uniportal incision to prevent mirror image for the needlescopic surgeon. Similar to uniportal VATS technique, the 30-degree thoracoscopy is inserted in the posterior part of the incision and the instruments are placed below the camera. In the setting of needlescopic-assisted uniportal VATS, the procedure usually begins with hilar dissection. Adequate exposure of the hilar area is achieved by the instrument inserted through the uniport, such as curve suction and Endo Peanut, and the dissection deep to the perivascular sheath can be easily performed using needlescopic hook electrocautery with countertraction provided by a needlescopic grasper using a two-hand surgical maneuver (Figure 3). Segmentectomy follows the principles of pulmonary anatomical resections such as division of segmental veins, segmental arteries, and the lobar segmental bronchus. Dissection around the vascular structures can be efficiently performed with collaboration between the thoracoscopic dissector and needlescopic hook electrocautery, just like in open surgery (Figure 4). With the assistance of the needlescopic instruments, the anvil of endostapler can safely pass through the pulmonary vessels and bronchus in the same way as in multiportal VATS using vascular loops (Figure 5) or Penrose drain tube guidance (Figure 6). After the segmentectomy, radical mediastinal lymphadenectomy completes the procedure and a chest tube is inserted through the uniportal incision.
Video atlas of needlescopic-assisted uniportal VATS segmentectomy
- Right upper lobe posterior (S2) segmentectomy (Figure 7);
- Right lower lobe anterior (S8) segmentectomy (Figure 8);
- Left upper lobe apicoposterior (S1 + S2) segmentectomy (Figure 9).



Results
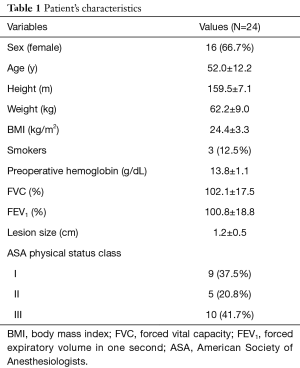
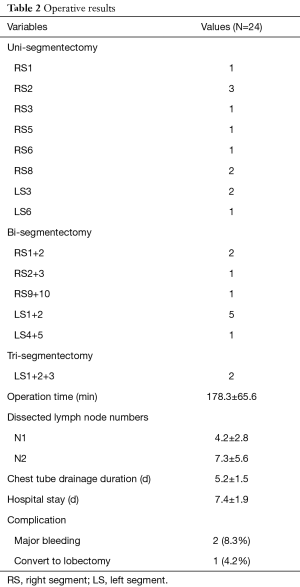
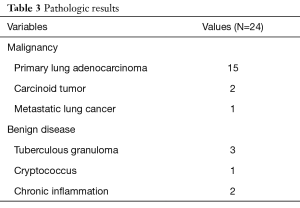
From December 2016 to June 2017, 22 consecutive patients underwent 24 segmentectomies for malignant or benign pulmonary diseases. Eight patients were male and 14 were female. Within the group, two female patients underwent bilateral thoracoscopic surgeries and the other patients underwent unilateral surgeries; their preoperative characteristics are reported in Table 1. The mean age was 52 years, and the median body mass index was 24.4 kg/m2. The median tumor size was 1.2 cm. The mean forced vital capacity was 102.1% of predicted and the mean forced expiratory volume in 1 second was 100.8% of predicted. At the time of the procedure, the American Society of Anesthesiologists Physical Status Classification grade was class 1 in 9 patients, class 2 in 5, and class 3 in 10. The operative results are reported in Table 2. There were 12 uni-segmentectomies, 10 bi-segmentectomies, and 2 tri-segmentectomies. The mean operation time was 178.3 minutes. The mean duration of chest tube drainage was 5.2 days, and the mean duration of hospital stay was 7.4 days. There were two episodes of major bleeding which were successfully controlled without conversion to thoracotomy or conventional VATS, and one case required conversion to lobectomy due to unidentifiable lesion in the resected segment. Of the 24 nodules evaluated, 18 were malignant and 6 were benign lesions (Table 3). Pathological examination showed that adenocarcinoma was the most common malignancy.
Full table
Full table
Full table
Conclusions
We have presented our experience with needlescopic-assisted uniportal VATS segmentectomy, which is an extension of uniportal VATS. Based on the technique of uniportal VATS, the assistance of additional needlescopic instruments was expected to make the procedure easier and safer without compromising the advantages of uniportal VATS, and the surgery can be performed with better collaboration between the uniportal surgeon and surgical assistant.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study has been approved by the Research Ethics Committee of National Taiwan University Hospital, Hsin-Chu Branch (approval number: 106-032-E).
References
- Okada M, Nishio W, Sakamoto T, et al. Effect of tumor size on prognosis in patients with non-small cell lung cancer: the role of segmentectomy as a type of lesser resection. J Thorac Cardiovasc Surg 2005;129:87-93. [Crossref] [PubMed]
- Kent M, Landreneau R, Mandrekar S, et al. Segmentectomy versus wedge resection for non-small cell lung cancer in high-risk operable patients. Ann Thorac Surg 2013;96:1747-54; discussion 1754-5.
- Nakamura K, Saji H, Nakajima R, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 2010;40:271-4. [Crossref] [PubMed]
- El-Sherif A, Gooding WE, Santos R, et al. Outcomes of sublobar resection versus lobectomy for stage I non-small cell lung cancer: a 13-year analysis. Ann Thorac Surg 2006;82:408-15; discussion 415-6. [Crossref] [PubMed]
- Sienel W, Dango S, Kirschbaum A, et al. Sublobar resections in stage IA non-small cell lung cancer: segmentectomies result in significantly better cancer-related survival than wedge resections. Eur J Cardiothorac Surg 2008;33:728-34. [Crossref] [PubMed]
- Bao F, Ye P, Yang Y, et al. Segmentectomy or lobectomy for early stage lung cancer: a meta-analysis. Eur J Cardiothorac Surg 2014;46:1-7. [Crossref] [PubMed]
- Zhang L, Li M, Yin R, et al. Comparison of the oncologic outcomes of anatomic segmentectomy and lobectomy for early-stage non-small cell lung cancer. Ann Thorac Surg 2015;99:728-37. [Crossref] [PubMed]
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections--a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Evolving from conventional video-assisted thoracoscopic lobectomy to uniportal: the story behind the evolution. J Thorac Dis 2014;6:S599-603. [PubMed]
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5 Suppl 3:S226-33. [PubMed]
- Aresu G, Weaver H, Wu L, et al. The Shanghai Pulmonary Hospital uniportal subxiphoid approach for lung segmentectomies. J Vis Surg 2016;2:172. [Crossref]
- Krpata DM, Ponsky TA. Needlescopic surgery: what's in the toolbox? Surg Endosc 2013;27:1040-4. [Crossref] [PubMed]
- Chang YC, Chen CW, Huang SH, et al. Modified needlescopic video-assisted thoracic surgery for primary spontaneous pneumothorax: the long-term effects of apical pleurectomy versus pleural abrasion. Surg Endosc 2006;20:757-62. [Crossref] [PubMed]
- Oda M, Matsumoto I, Takizawa M, et al. Needlescopic video-assisted wedge resection combined with the subcostal trans-diaphragmatic approach for undetermined peripheral pulmonary nodules. Surg Endosc 2013;27:3671-7. [Crossref] [PubMed]
- Sihoe AD, Hsin MK, Yu PS. Needlescopic video-assisted thoracic surgery pleurodesis for primary pneumothorax. Multimed Man Cardiothorac Surg 2014;2014. pii: mmu012.
- Yang SM, Wu WT, Liu YH, et al. Right upper lobe posterior (S2) segmentectomy. Asvide 2017;4:397. Available online: http://www.asvide.com/articles/1711
- Yang SM, Wu WT, Liu YH, et al. Right lower lobe anterior (S8) segmentectomy. Asvide 2017;4:398. Available online: http://www.asvide.com/articles/1712
- Yang SM, Wu WT, Liu YH, et al. Left upper lobe apicoposterior (S1 + S2) segmentectomy. Asvide 2017;4:399. Available online: http://www.asvide.com/articles/1713
Cite this article as: Yang SM, Wu WT, Liu YH, Ko HJ. Needlescopic-assisted uniportal video-assisted thoracoscopic pulmonary anatomical segmentectomy. J Vis Surg 2017;3:138.