Navigational bronchoscopy-guided dye marking to assist resection of a small lung nodule
Introduction
In minimally invasive thoracic surgery, one must consider that 63% of pulmonary nodules less than 10 mm in diameter or greater than 5 mm from the pleural surface cannot be detected using palpation techniques through port incisions (1). Various methods to assist with localization of pulmonary nodules have been described, each with their own advantages and disadvantages. This includes CT guidance for hookwire placement, radiotracer placement or percutaneous injection of methylene blue and then usually the need to be transported to the OR for surgical resection (2). Electromagnetic navigational bronchoscopy (ENB) can be performed by the surgeon at the same setting as the planned lung resection to localize the lesion and dye mark the pleura. We have previously described our experience in 70 cases where ENB-guided dye marking was used to localize pulmonary nodules (3). Here we present a case where this technique was employed to resect a suspicious small pulmonary nodule.
Case presentation
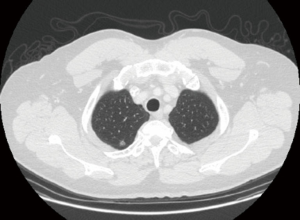
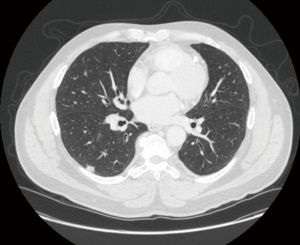
A 59-year-old male, previous heavy smoker, who had recently undergone a sigmoid colectomy for T1N1a colon adenocarcinoma was found to have a 1 cm superior segment right lower lobe nodule (Figure 1). The patient had a CT-guided needle biopsy of the lesion, showing adenocarcinoma of lung origin. In preoperative evaluation of his CT images, the operating surgeon noticed a small nodule in his right upper lobe that was persistent on recent CT scan evaluations (Figure 2). He was scheduled for a right lower lobe superior segmentectomy for his known cancer and for ENB dye with wedge resection of the upper lobe nodule (Figure 3).
Procedure
Planning
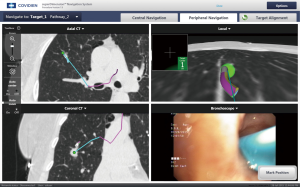
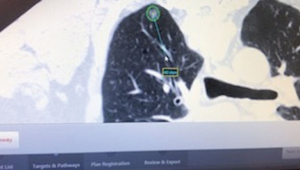
In our institution, we use the superDimension Navigation System (Covidien Inc., Minneapolis, MN, USA) for localizing lung nodules. Preparing for an ENB case involves uploading a CD of the patient’s chest CT (ideally 1–1.25 slice thickness) into planning software provided by the company that uses 3D images to find a pathway to the lesion of interest, ideally using the closest bronchus. For this patient, a pathway was created to locate the right upper lobe nodule (Figure 4).
Operating room
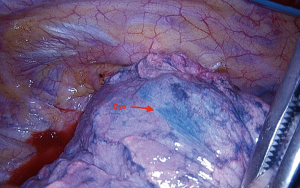
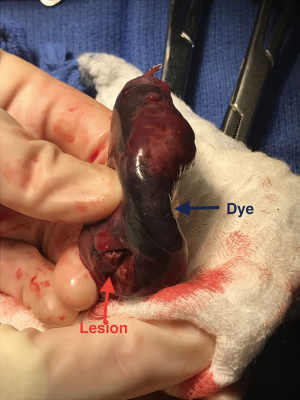
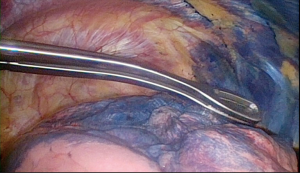
In the operating room, a location board that creates the electromagnetic field was placed under the mattress in the area where the patient’s chest would be (Figure 5). The patient then underwent general anesthesia with a single lumen tube. First a regular bronchoscopy was performed to clear the airway of secretions. Using the predesigned plan, an extended working catheter was directed through the posterior segment of the right upper lobe and guided to within 1 cm of the nodule using a locatable guide (Figure 6). Once in position, the guide was removed and a bronchoscopic needle, preloaded with methylene blue, was inserted through the extended working catheter that was still directed at the nodule. The needle was advanced out of the catheter and 0.5 mL of methylene blue was injected and then the needle was advanced for another 1 cm and an additional injection of 0.5 mL of dye was given. The needle and extended working catheter were removed, the airway cleared of secretions and the single lumen tube was replaced with a double lumen tube. The patient was then placed in the left lateral decubitus position for VATS surgery and three port sites were used. Once the patient’s known right lower lobe adenocarcinoma was confirmed by visualization and palpation, location of the blue dye in the pleura of the upper lobe was done so the small nodule could be resected first before the dye dissipated (Figure 7). Resection of the area was done with a linear stapler, taking care to take adequate margins around the dye mark as the dye is sometimes adjacent, as opposed to right on top, to the nodule. The specimen was examined in the OR where the nodule was seen just off to the side of the blue dye (Figure 8) and the specimen was sent for permanent evaluation. The surgeon then proceeded with the planned right lower lobe superior segmentectomy for the patient’s known 1 cm adenocarcinoma.
Postoperative
His chest tube was removed on post-op day 1 and the remainder of his hospital course was uncomplicated. The definitive histopathological diagnosis of the lesion in the right upper lobe was a 3-mm atypical adenomatous hyperplasia (AAH). The right lower lobe lesion was a pT1aN0M0. The patient has since started his chemotherapy for his colon cancer.
Discussion
The case described was an excellent example of how ENB dye marking can help locate and manage a lung nodule minimally invasively, even at 3 mm in size. As with any technology there will be a learning curve but the steps in the procedure are simple for any thoracic surgeon to perform.
Adverse events, such as bleeding or pneumothorax, are rarely seen when using ENB as compared to CT-guided methods (5). The main limitation is failure of proper injection of the methylene blue, whether one sees no dye marking at all on the lung or the needle passed through the pleura and dye is now dispersed throughout the pleural space (Figure 9). In this situation, if one is still unable to palpate the nodule with VATS, then a thoracotomy may necessary. Also be mindful, that if the pleural marking doesn’t match the area expected by CT, that improper placement of chest sensors or the location board can lead to erroneous location of the catheter in the lung despite the program indicating you are at the nodule.
For this patient, the suspicious nodule was an AAH which has been recognized in the 2004 World Health Organization (WHO) classification of lung cancers as a pre-invasive lesion of lung adenocarcinoma, though the incidence and time required for AAH to develop in to early stage adenocarcinoma is not well-defined (6). This case report is not meant to encourage more aggressive resection of AAH lesions; but, as the patient was having a definitive cancer operation on the same side, the surgeon felt that removing this suspicious nodule was appropriate, especially given its favorable location for a wedge.
Conclusions
ENB-guided dye localization is a feasible and safe technique that can be used to help thoracic surgeons identify either small or deep pulmonary nodules that might be difficult to palpate in minimally invasive cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: B Weksler is (I) proctor for Intuitive Surgery; (II) consultant for Bard; (III) scientific advisory board, Biodesix.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
- Cuadrado DG, Grogan EL. Localization Techniques for Small Lung Nodules. Oper Tech Thorac Cardiovasc Surg 2014;19:179-98. [Crossref]
- Marino KA, Sullivan JL, Weksler B. Electromagnetic Navigation Bronchoscopy for Identifying Lung Nodules for Thoracoscopic Resection. Ann Thorac Surg 2016;102:454-7. [Crossref] [PubMed]
- Sullivan JL, Martin MG, Weksler B. Planning and intraoperative use of electromagnetic navigational bronchoscopy to identify and resect a small right upper lobe pulmonary nodule. Asvide 2017;4:450. Available online: http://www.asvide.com/articles/1746
- Zhang W, Chen S, Dong X, et al. Meta-analysis of the diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules. J Thorac Dis 2015;7:799-809. [PubMed]
- Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol 2005;40:90-7. [Crossref] [PubMed]
Cite this article as: Sullivan JL, Martin MG, Weksler B. Navigational bronchoscopy-guided dye marking to assist resection of a small lung nodule. J Vis Surg 2017;3:131.