Thymic MIS: state of the art across the world (Russian Federation)
Background
Modern management of mediastinal diseases expand the role of surgery greatly. Most thymic masses need the surgical treatment, and total resection of tumors is a general prognostic factor for good results. Any thymic masses may be malignant, so conservative treatment or observation without morphological verification is associated with high risk of tumor invasion into the border organs. In addition, thymectomy, regardless of morphological changes of the thymus considered as a component of comprehensive treatment of myasthenia gravis. Regardless of morphogenesis (malignant or benign), any mass in the anterior mediastinum is a potential threat to the compression of vital organs.
There is more than 70 years history of open approaches for surgical treatment of thymic tumors. Most authors prefer different types of sternotomy than thoracotomy. VATS access became widely introduced only last 20 years, and quickly became popular among thoracic surgeons. First papers, which showed the possibility of using robot-assisted operations in thymic surgery, appeared in 2006–2007 years.
The aim of this paper is to show the current situation of minimally invasive surgery of thymic diseases in the Russian Federation.
Thymic surgery in Russia: literature review
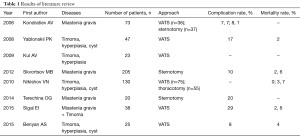
Analysis of Russian literature with national search system (http://elibrary.ru) showed 299 papers, which contain key word: thymectomy. Clinical trials, which were performed during last 10 years, were selected. Articles with the same title and with the same list of authors were excluded. Thereby eight original trials were found, that contain results of 561 thymectomies (Table 1). Forty-three percent of patients (244 from 561) were operated by VATS. Most articles are devoted to surgical treatment in patients with myasthenia gravis. Comparison trials showed advantages of VATS versus open approaches (sternotomy and thoracotomy). Rate of postoperative complications was 7.7–17% and 10–30%, mortality was 0–2.6% and 0–3.7% for minimally invasive and open thymectomy, respectively. Also VATS groups of patients are characterized by less pain and early recovery. Also noteworthy, the technical protocol for VATS thymectomy in some clinics provides the absence of chest tube in cases with uneventful surgery.
Full table
Unfortunately, existing publications do not reflect all features of thymic surgery. The annual report of the Association of Thoracic Surgeons of Russia contains limited information about the number of surgeries, complications and mortality. In this context, the survey of all Russian thoracic centers was performed to study the general trend in this field.
Current status of thymic surgery in Russia: methods of investigation
ESTS Database annual report is one of the most detailed reports containing data on thymic surgery (1). There is no analogue of this database in Russia, unfortunately. Analysis of annual report of Association of Thoracic Surgeons of Russia showed that overall number of surgical procedures for mediastinal diseases remains at the same level last years (1,324–1,405 surgeries per year). Little part of these (14%) performed for diseases of the thymus.
We developed a questionnaire in order to find branches of evolution of minimally invasive surgery of thymic gland in our country. There were different questions about features of preoperative examination, indications for surgery, surgical techniques and postoperative management of patients with thymic diseases (Table 2). To make a survey we have sent out a questionnaire to 30 thoracic centers in all regions of the Russian Federation, which had experience in thymic surgery.
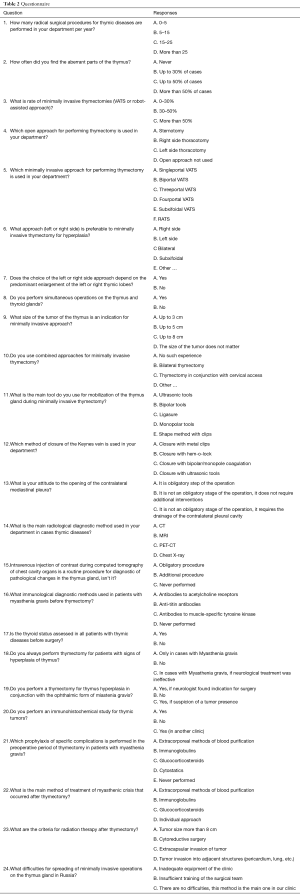
Full table
Results of the survey and its discussion
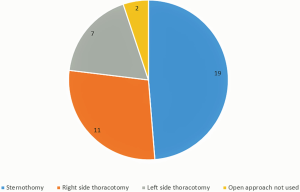
We received responses from 25 (83%) thoracic departments. This frequency of response matched with data of Association of Thoracic Surgeons of Russia about number of thoracic centers, which had experience in minimally invasive thymic surgery. At least 25 radical operations per year for thymic diseases were performed in each center. Today, the main part surgical procedures are performed by minimally invasive approach, and our survey was planned for study of these. In addition we asked about open approaches in one of the questions. So the most surgeons (19/76%) prefer sternotomy among all open approaches (Figure 1).
Preoperative assessment of patients
Symptoms of the diseases of the thymus gland are divided into four groups: local symptoms of compression or invasion of surrounding organs, general symptoms, thymus-associated syndromes, asymptomatic. The essential feature of the thymic disease is a high rate of thymus-associated syndromes (neuromuscular diseases, hematologic syndromes, diffuse connective tissue diseases and endocrine syndromes). Therefore, a diverse clinical picture necessitates a detailed examination of patients. Current diagnostic algorithm is described in “Clinical recommendations for the diagnosis and treatment of myasthenia gravis” by Russian Society of neurologists [2013].
Radiological methods are the most commonly used diagnostic procedures. Routine X-ray examination is associated with a very low diagnostic efficacy. Currently, computed tomography is used in all clinics in the Russian Federation as a gold standard for diagnostic of mediastinal masses. Nevertheless, the computed tomography with intravenous injection of contrast is performed routinely only in 52% (13 centers) of all thoracic departments. MRI is an infrequent examination (5/25% of respondents). We received information that PET-CT used only in one clinic.
The prevalence of myasthenia gravis and myasthenic syndromes among all thymus-associated syndrome influenced to the plan of preoperative examination. Routine diagnostic algorithm included neuro myography and the level measurement of antibodies to acetylcholine receptors in all centers. Such patients are often transmitted to the thoracic clinic from neurological department (15/60% of respondents) after full examination and course of preoperative treatment, if required. Other patients come to surgical center (mainly with tumors) after screening radiological examination. Additionally, antibodies to muscle-specific tyrosine kinase are determined in three departments (12%), anti-titin antibodies are determined in five departments (20%).
Widespread belief, that autoimmune diseases of the thyroid gland and myasthenia gravis is frequent combination (2,3). However, the experience of simultaneous operations on the thyroid and thymus glands showed in work only of five thoracic centers (20%). In this context, the assessment of thyroid status performed by nine respondents (36%) before surgery.
Indication and volume for surgery
All mediastinal masses are an absolute indication for surgery, and also an indication for thymectomy, now well known (4,5). Currently, the most authors consider that the adequate volume of surgery for patients with myasthenia gravis is extended thymectomy with the total remove of the fat tissue in anterior mediastinum and infrathyroid area (6). Frequent opinion is that total remove of fat associated with the possible presence of aberrant thymic tissue in majority of cases. However, 12 respondents (48%) said they had never met aberrant thymus lobes in their practice. Experience of 11 (44%) centers showed presence of abberant thymic tissue in up to 30% cases.
Surgery for hyperplasia of the thymus gland is marked by heterogeneous views. Sixteen respondents (64%) performed thymectomy in all patients with a combination of hyperplasia and myasthenia gravis. In eight centers (32%), surgical treatment was performed in such cases only if the neurological therapy was ineffective.
Perioperative period
One of the points of the perioperative period is the prevention of specific complications in patients with myasthenia gravis. Extracorporeal methods of blood purification (for crysis) (15 respondents/60%) and glucocorticosteroids (18 respondents/72%) are used in the most of the clinics.
Another point is the detailed examination of removed specimens with determination of the type of thymoma and degree of tumor’s invasion. Pathological examination includes an immunochemistry tests in all centers.
Postoperative treatment has to be performed under supervision of neurologist, if required. The reasons for radiation therapy are tumor invasion into surrounding organs (18 respondents/72%), extracapsular tumor invasion (9 respondents/36%) and cytoreductive surgery (13 respondents/52%).
Surgical approach for thymectomy: features of VATS thymectomy
Today VATS is the most usable approach for surgical procedures for thymic diseases (more than 50% surgeries per year in 17 from 25 clinics). Nevertheless, different surgical schools showed various techniques.
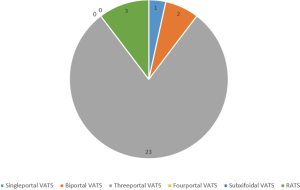
The feasibility of uniportal thoracic surgery is proved on the example of lobectomies. However, uni- and biportal VATS were performed only in three centers (12%), according to the results of the survey. Most common approach is three portal VATS (23 centers/92%). We did not get results about the use of subxyfoidal access in any clinic (Figure 2).
The preferred side of the approach is the right (Figure 3) (7). However, five respondents (20%) used left-side (Figure 4) (8), and one used bilateral approach (4%). Sixty-eight percent of the respondents (17 respondents) planned operation in conformity with enlarged right or left lobes of thymus gland, and 12% of respondents (13 respondents) used additional cervical approach for removed cervical part of thymus.

The standard technique of operation included isolation of the thymus gland with an ultrasonic or bipolar dissector and clipping of the Keynes vein. Total removal of anterior mediastinal fat from low level of pleural cavity to infrathyroid area is one of the key points of operation in cases associated with myasthenia gravis. This step became more simple with apply of ultrasonic devices. Opening of the contralateral pleura during this step could help to visualize phrenic nerve and clear boundaries of fat dissection. The majority of surgeons (17 respondents/68%) consider this method to be dispensable, but 24% of them (6 respondents) placed additional chest tube in the contralateral pleural cavity in such cases. Other surgeons (single center/4%) did not use pleural drainage for uncomplicated cases. However, standard technique of thymectomy includes positioning of one chest tube, and its removal on the first postoperative day.
Technique of operation: features of RATS approach
Initially, robotic surgical systems were designed for comfortable work in a confined space. Exactly such area in the chest is mediastinum. So the first surgical procedures in the most thoracic centers were resections of mediastinal masses and thymectomy. Generally, spread of robotic thoracic surgery in the Russian Federation associated with difficulties due to the high cost. Today, we have information about initial experience of robotic thymectomy in three centers in Russia.
Features of operation and preoperative preparation are the same as for VATS thymectomy. Additional step is the docking of robotic system under 15–20 degree of patient head. We use VATS-based approach for robot-assisted operation with three robotic ports (one port for camera and two ports for tools) and one assistant port. Suction/irrigation, retraction and removal of specimen are performed from assistant port. Precise preparation and improved visualization during robotic surgery make it possible to refuse of the additional cervical approach for to remove infrathyroid fat. The side of surgery also depends on localization of thymoma or the most enlarged lobe of thymus gland. However, left-side approach for thymectomy is more comfortable versus VATS, due to technical features of robotic surgical system.
Single-center experience in robot-assisted thymectomy (Saint-Petersburg Research Institute Phthisiopulmonology)
During period from January 2014 to March 2017, 14 patients with different disease of thymus gland underwent thymectomy with using of surgical robotic system (da Vinci Si Robotic System). There were 11 patients with thymomas and 3 patients with thymic cysts. Three cases were associated with myasthenia gravis and were underwent preoperative treatment in neurological department.
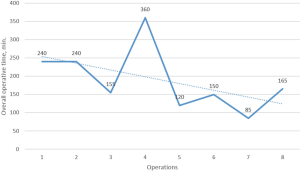
The most operations were performed with right-side approach (10 patients/77%) (Figure 5) (9). Learning curve of surgery showed on Figure 6. In these cases average operative time was 202+81 min (console operative time was 87+29 min). Intraoperative blood loss was 30–200 mL. In two cases of thymoma robot-assisted thymectomies were combined with: (I) robot-assisted right upper lobectomy (for peripheral NSCLC); (II) right-side hemi-thyroidectomy thyroid goiter (transcervical approach).

Left-side approach was used in four cases (average and console operative time were 252±17 and 210±10 min respectively) (Figure 7) (10). Intraoperative blood loss was 30–100 mL.

There was one case (7%) with conversion to thoracotomy due to large size of tumor and dense adhesions in the area of apex of tumor, and it was the case with previous strumectomy (for thyroid goiter).
There were no postoperative morbidity and mortality in this initial series of patients.
Conclusions
The question of the validity of minimally invasive surgery in diseases of the thymus gland has been widely discussed in the medical literature in the last 20 years.
Current status of thymic surgery in Russia is presented by VATS as a standard access for all thymic diseases (in 19 thoracic centers/6%).
Robotic surgery today is a developing technology today, in this way the first results showed the possibility of robotic procedures as a future alternative for VATS approach in the thymic surgery.
Nevertheless, inadequate equipment (3 centers/12%) and insufficient training (5 centers/20%) of surgical team are factors, which brake the development of minimally invasive surgery in some thoracic centers.
Acknowledgements
We thank our colleagues: Ablitsov AY (Mosccow), Avzalethdinov AM (Ufa), Akopov AL and Dvoreckii CY (St. Petersburg), Atyukov MA (St. Petersburg), Bagirov MA (Moscow), Bazarov DV (Moscow), Benyan AS (Samara), Broder IA and Sekhniaidze DD (Tyumen), Gumerov II (Ulyanovsk), Kochenogov AV (Vologda), Kotrunov V.V. (Volgograd), Korobeinikov FV (Novosibirsk), Kozak AR (St. Petersburg), Nechay VS (Tula), Pikin OV (Moscow), Pechetov AA (Moscow), Pischik VG (St. Petersburg), Popov MI (Moscow), Porkhanov VA and Danilov VV (Krasnodar), Pushkin SY (Samara), Ratnov SA (Lipetsk), Razumovsky AY (Moscow), Sigal AM (Kazan), Skriabin SA (Murmansk), Sulimanov RA (Novgorod), Topolnitsky EB (Tomsk), Voronchikhin AE (Izhevsk), who provided the insight and expertise that was greatly assisted in the research, although they may not agree with all of the interpretations and conclusions of this paper. We thank Vadim Pischik and Evgenii Shepichev for provision of video of VATS thymectomy that much improved the manuscript. We also thank Igor Vasilev for help in concept and design of this paper and Nina Koneva for improving the use of English in the manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- ESTS Database annual report 2015. Available online: http://www.ests.org/_userfiles/pages/files/ESTS%20201Silver_Book_FULL_PEF.pdf
- Budavari AI, Whitaker MD, Helmers RA. Thymic hyperplasia presenting as anterior mediastinal mass in 2 patients with Graves disease. Mayo Clin Proc 2002;77:495-9. [Crossref] [PubMed]
- Weissel M. Mild clinical expression of myasthenia gravis associated with autoimmune thyroid disease. J Clin Endocrinol Metab 1997;82:3905-6. [PubMed]
- Ried M, Guth H, Potzger T, et al. Surgical resection of thymoma still represents the first choice of treatment. Thorac Cardiovasc Surg 2012;60:145-9. [Crossref] [PubMed]
- Ried M, Marx A, Götz A, et al. State of the art: diagnostic tools and innovative therapies for treatment of advanced thymoma and thymic carcinoma. Eur J Cardiothorac Surg 2016;49:1545-52. [Crossref] [PubMed]
- Novellino L, Longoni M, Spinelli L, et al. “Extended” thymectomy, without sternotomy, performed by cervicotomy and thoracoscopic technique in the treatment of myasthenia gravis. Int Surg 1994;79:378-81. [PubMed]
- Yablonskii P, Kudriashov G, Pischik V, et al. VATS thymectomy (right-side approach). Asvide 2017;4:349. Available online: http://www.asvide.com/articles/1663
- Yablonskii P, Kudriashov G, Pischik V, et al. VATS thymectomy (left-side approach). Asvide 2017;4:350. Available online: http://www.asvide.com/articles/1664
- Yablonskii P, Kudriashov G, Pischik V, et al. RATS thymectomy (right-side approach). Asvide 2017;4:351. Available online: http://www.asvide.com/articles/1665
- Yablonskii P, Kudriashov G, Pischik V, et al. RATS thymectomy (left-side approach). Asvide 2017;4:352. Available online: http://www.asvide.com/articles/1666
Cite this article as: Yablonskii P, Kudriashov G, Pischik V, Sigal E, Nuraliev S. Thymic MIS: state of the art across the world (Russian Federation). J Vis Surg 2017;3:119.