Use of autologous platelet rich plasma (PRP) in stopping massive hemoptysis at the Lung Center of the Philippines: a pilot study
Introduction
Massive hemoptysis is a sequelae from the different disease entities related to the lung. This may be from different infections caused by bacteria, fungal and even carcinoma. Priority is to have a patent airway and isolating the bleeding bronchus from the adjacent areas. In our institution identification and localization is done usually in the active stage with the use of flexible bronchoscope instead of rigid bronchoscope, so that expectoration by the patient is still possible and this followed by Fogarty balloon tipped blockade.
Isolation of the bleeding bronchus is done either by using a balloon tipped Fogarty catheter which tamponade the area; endotracheal intubation with a single lumen or double lumen to isolate the bleeding lung, or angiographically guided embolization which blocks the blood supply (1). The situation in our institution is the unavailability of the Fogarty catheter. Angiographic embolization though available in other institution is an expensive procedure for our patients and at times they are not stable to undergo the procedure. Intubating the patient does not stop the bleeding though it protects the airway.
In order to solve the problem of unavailability, expensiveness and difficult procedure we tried to find out whether there are other alternatives, that would temporize the hemoptysis in the sense that it should be readily available, cheap and simple to do, which would prepare the patient for a definitive procedure. We then thought of using platelet.
Platelet is readily available because every patient has them. Preparing them is also not expensive, what are needed is just the centrifuge and a container to store them. Lastly trying to instill platelet concentrate is a very simple procedure all that is needed is to identify the bleeding structure and instill it. Because of this, we embarked on a study using platelet rich plasma (PRP) for its usage and this would come from the patient himself/herself, thus autologous and is readily available. This is a pilot study undertaken to determine its feasibility in temporizing massive hemoptysis in preparation of the patient for definitive procedure. This report describes the outcome after instilling autologous PRP on patients with massive hemoptysis.
Methods
Patient selection and workup
Inclusion criteria
All patients admitted at Lung Center of the Philippines with massive hemoptysis as defined, who voluntarily gives informed consent for the procedure.
Exclusion criteria
- Patients intubated in acute respiratory failure;
- Hypotensive;
- Septic recently had a heart attack;
- Recent cerebrovascular accident (CVA);
- Bleeding from malignancy.
Pre-operative preparation
Detailed procedure
- Once the patient was seen at the emergency room (ER), criteria were assessed whether the patient had massive or non-massive hemoptysis and stable;
- After the patient was assessed that he/she was qualified for the study an informed consent was given;
- The patient is placed on intravenous (IV) fluid and on nothing per orem (NPO);
- Laboratories requested were complete blood count (CBC), platelet, blood typing, chest X-ray (CXR), electro-cardiogram (ECG), arterial blood gas (ABG);
- 50 cc of blood was extracted and placed in a test tube with Citrate Phosphate Dextrose Adenine Solution (CPDA-1) and then sent to the laboratory for centrifuge.
Equipment preference card
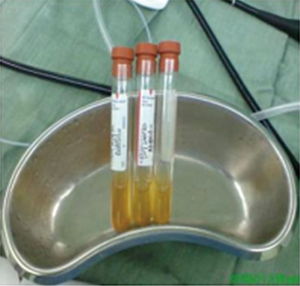
A centrifuge, Olympus bronchoscope and tower with monitor. Plastic tubing fit for the accessory port of the bronchoscope (Figure 1). Sterile test tube for the autologous PRP (Figure 2).
Procedure—role of team members
- The patient was brought to the operating room for fiberoptic bronchoscopy(FOB) under monitored anesthesia care (MAC). There was no sedation or general anesthesia.
- The thoracic surgeon was the one who did the bronchoscopy with the assistance of a nurse and a circulating nurse. Lidocaine was instilled to the bronchus from the utility or accessory port of the bronchoscope.
- Localization was done.
- The 3-test tube with autologous PRP were instilled on the affected bronchus using the irrigating plastic tube designed for the bronchoscope and allowed five [5] minutes to pass before instilling the next test tube (Figure 3).

Post-operative management
The patient was then sent to the SICU or ward afterwards. Monitoring was done whether there was recurrence of hemoptysis and the amount if massive or non-massive.
Results
Overall, 14 out of 20 patients (70%) were reported to have stopped bleeding immediately. Subsequent hospital days showed that 8 out of 20 patients (40%) had no hemoptysis. However, one [1] post-TB bronchiectatic patient had recurrence of massive hemoptysis, approximately 250 mL per expectorate, and expired within the 7 days observation and one [1] patient had lobectomy on the 2nd day. The rest had non-massive hemoptysis, wherein their expectorations were only streaks of blood. Moreover, there is one [1] patient noted to have recurrence of massive hemoptysis 1 week after autologous PRP infusion and eventually intubated. Majority of the subjects, eleven 11 (55%), were diagnosed to have post-TB bronchiectasis, five (25%) had active tuberculosis (TB), three (15%) had aspergilloma and one (5%) had multi-drug resistant tuberculosis (MDRTB). The rest of the patients were worked-up prior to operation.
Discussion
Massive hemoptysis is the expectoration of >600 mL of blood within 24 hours or when there is profuse bleeding that breathing is interrupted (generally more than 200–240 mL, or about 1 cup, in an hour) (3). Unquantified amount with hemodynamic instability or anemia requiring transfusion. The primary goal of management is prevention of asphyxia and cessation of bleeding (4,5).
Tsukamoto et al. in 1989 has been using fibrinogen-thrombin therapy (fibrin glue) or the use of thrombin therapy for massive hemoptysis by infusing through fiberoptic bronchoscope (6,7). The problem encountered here is the availability and possible reaction.
Platelets are known to perform multiple functions during injury and tissue repair.
Platelets initiate the body’s response to a normal sequence of events that provide clotting and healing of the damaged tissue.
The clotting cascade is initiated with the interaction of platelet membranes and receptors with damaged vascular endothelium. Underlying collagen is exposed to the blood, which acts as an agonist and triggers changes in the platelet membrane (8). Hemoptysis occurs similarly and with the application of the autologous PRP the clotting cascade starts faster than the normal considering that the autologous PRP is 4 to 5 times concentrated.
Platelet-rich plasma was first identified in the early 1990s through the use of plasmapheresis and PRP sequestration. It has been used in cardiothoracic surgery; cosmetic and plastic surgery; ear, nose, and throat surgery; general surgery; major vascular surgery; neurosurgery; obstetrics and gynecological surgery (i.e., cesarean section, hysterectomy); ophthalmology; oral surgery; orthopedic surgery; urology; and wound healing (8). Combining PRP with thrombin and calcium to create a gel is considered to be the practice of medicine (9). Autologous PRP also has potential for use as a hemostatic agent because it binds tissues and locally activates the coagulation cascade. When the coagulation cascade is activated, high concentrations of platelets adhere to the wound surface. Platelet activation and degranulation releases a number of hemostatic substances (10).
Autologous platelet-rich plasma is a safe, cost effective, autologous product. It is readily available at the point-of-care, provides antibacterial protection, and eliminates the concern of disease transmission and immunogenic reactions.
Recommendation
This is just a preliminary study and future randomized control trials with large sample size will be needed to recognize its effect for in-hospital management of massive hemoptysis and may be a suitable alternative to our standard Fogarty blockade.
Tips, tricks and pitfalls
Preparation of autologous PRP
- 50 mL of blood is extracted from the patient and placed in a five 10 mL test tube with 1.4 mL anticoagulant citrate phosphate dextrose adenine (cpda-1) solution each which I prepared personally aseptically. Fluid replacement may be needed for sensitive patient after extraction.
- This is centrifuged with a soft spin at 2,500 rpm in 5 minutes.
- The centrifuged is stopped to allow a 60-second count down to help loosen platelets. The concentrated platelet is collected with the buffy-coat and the RBC is discarded.
- After the 60-second countdown a hard spin follows at 3,500 rpm in 10 minutes and the PRP is collected which is in the bottom of the test tube and buffy coat is drawn up using a pipette and discarded. The test tube is then transported in the surgical field. Note: the remaining 1–2 cc of plasma is used to re-suspend the concentration of platelets and white cells.
This test tube is labeled PRP. It is also advice to continuously shake the test tubes while on transport or awaiting instillation.
Patients with massive hemoptysis were not sedated so that they can still expectorate pooled blood but the team was ready for intubation in case of desaturation as a result of asphyxiation. PRP was not recommended on malignant cases because of the growth factor contents and possible effect although no study was yet reported.
Precautions were also advised for severely infected area. Although studies reported it activates macrophages and migration.
Acknowledgements
Research and Development Committee, Lung Center of the Philippines for financial support for the study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional Ethical Committee in the Lung Center of the Philippines and written informed consent was obtained from all patients.
References
- Winter SM, Ingbar DH. Massive Hemoptysis: Pathogenesis and Management. J Intensive Care Med 1988;3:188. [Crossref]
- Sarmiento AG, Danguilan JL, Mariano ZM, et al. The autologous PRP. Asvide 2017;4:306. Available online: http://www.asvide.com/articles/1618
- Crocco JA, Rooney JJ, Fankushen DS, et al. Massive hemoptysis. Arch Intern Med 1968;121:495-98. [Crossref] [PubMed]
- Hiramatsu T, Okamura T, Imai Y, et al. Effects of autologous platelet concentrate reinfusion after open heart surgery in patients with congenital heart disease. Ann Thorac Surg 2002;73:1282-5. [Crossref] [PubMed]
- Algorithm for the initial management of hemoptysis. LCP 2006:15-21.
- Tsukamoto T, Sasaki H, Nakamura H. Treatment of hemoptysis patients by thrombin and fibrinogen-thrombin infusion therapy using a fiberoptic bronchoscope. Chest 1989;96:473-6. [Crossref] [PubMed]
- Floryan KM, Berghoff WJ. Intraoperative use of autologous platelet-rich and platelet-poor plasma for orthopedic surgery patients. AORN J 2004;80:668-74, quiz 675-8. [Crossref] [PubMed]
- Monteleone K, Marx R, Ghurani R. Wound repair/cosmetic surgery healing enhancement of skin graft donor sites with platelet-rich plasma. Presented at 82nd Annual American Academy of Oral and Maxillofacial Surgery Meeting, September 2000.
- Kevy S, Jacobson M, Benoit P. The biology of platelet concentrate as Prepared by the Harvest Technologies SmartPReP System. Presented at Techvest Conference on Tissue Repair, Replacement, and Regeneration, 3rd Annual Meeting, October 2001.
- Bhanot S, Alex JC. Current applications of platelet gels in facial plastic surgery. Facial Plast Surg 2002;18:27-33. [Crossref] [PubMed]
Cite this article as: Sarmiento AG, Danguilan JL, Mariano ZM, Barzaga MT. Use of autologous platelet rich plasma (PRP) in stopping massive hemoptysis at the Lung Center of the Philippines: a pilot study. J Vis Surg 2017;3:111.